Introduction
Childhood injury is an important public health problem that has been the focus of several World Health Organization (WHO) reports since 2005.1-3 It accounts for 9% of global mortality and is responsible for several hospitalizations, Emergency Department (ED) visits, and medical appointments.1-3 Globally, it has a major impact, not only on health costs, but also on temporary or permanent disabilities.1-3
Unintentional injuries (UI) are an important cause of death among adolescents and a major cause of morbility.4-8 Injuries are defined by WHO as “...the physical damage that results when a human body is briefly or suddenly subjected to intolerant energy levels”.3,9,10 When looking at the main etiologies of adolescent disability-adjusted life years lost, it becomes clear that UIs − mainly road traffic injuries − are an important factor.3 A recent WHO report pointed road traffic injuries as the leading cause of death in the 5−29-year-old population globally, with many inequalities between regions, and a rate of 9.3 deaths per 100,000 inhabitants in Europe in 2016.11 This rate has been declining in Europe since 2013, probably associated with improved road safety laws, safer infrastructures, adoption of vehicle standards, and improvement of access to post-crash care. 11
Adolescence is a vulnerability period for UIs, with a higher UI risk due to biological, social, and cognitive changes.4-6 The brain area participating in risk-benefit assessment and decision-making − the pre-frontal cortex − seems to be the last to mature, potentially accounting for adolescents’ impulsiveness and risk behaviors.12-20 This formative period of human brain development is key for the beginning or consolidation of protective or risk behaviors that will impact future adult life.3 WHO states that “investing in adolescent health will build on and sustain earlier gains in young child health, and will further enable adolescents to become healthy adults who are equipped to contribute positively to society”.8
To prevent injuries in adolescence, it is crucial to study their frequency and associated factors.6-8 Investing in adolescent health is crucial for improving public health indicators, as well as achieving economic and demographic benefits.21-24
To the best of our knowledge, this is the first Portuguese study assessing UI prevalence and characteristics in adolescents (10-17-year-old group).
Objectives
The main objective of this study was to identify and characterize UIs in adolescents attending the ED of two Portuguese hospitals. Secondary aims were to assess UI impact on adolescents’ health and life, and to investigate potential differences between second and third level hospitals.
Materials and Methods
Study design
A prospective, observational, two-center study was conducted to assess UI prevalence and characteristics in adolescents attending the ED. Throughout a 12-month period (September 2015 to October 2016), a survey of adolescents admitted to the ED of two Portuguese hospitals due to UI was conducted. Pediatrics Department of a second-level (A) and third-level (B) hospital participated. One month after the UI event, a telephone interview was performed to assess its impact on adolescents’ health and life.
Inclusion and exclusion criteria
Adolescents aged 10 to 17 years assessed in the ED for UI who consent to participate in the study were included. UIs were defined as:
accidental events, such as accidental falls (from own height or other heights);
traumatic injuries (excluding falls or road traffic injuries);
road traffic injuries (including with motor and non-motor vehicles or being runned over by a vehicle);
intoxication or poisoning (due to unintentional medication overuse, alcohol or drug use, carbon monoxide, farming pesticides, insect bites, sea animal bites, or dog or snake bites);
sun and non-sun burns (due to fire, contact with hot surfaces or liquids, caustic products, or electric burns);
asphyxia or suffocation (due to choking on foreign bodies, suffocation games, or self-suffocation);
drowning or near-drowning (including submersion in water or other liquids);
accidental use of fire weapons.
Unconscious adolescents or those with altered behavior due to unknown causes assessed in the ED were also included.
Adolescents with intentional injuries or suicidal ideation were excluded from the study.
The following adolescent developmental stages were considered: early (10 to 13 years old), middle (14 to 16 years old), and late (17 to 18 years old) stage.
Ethical aspects
Study was authorized by the Ethical Commitee of both hospitals and a written informed consent was retrieved from each participant and legal tutor upon hospital discharge.
Data collection
All data was recorded on a survey placed at the consultation room of each Pediatric ED. Patients meeting inclusion criteria were invited to participate in the study at the moment of hospital discharge. Adolescents signed a consent form and parental consent was also obtained. Information retrieved by the research team was recorded on a database with patient data pseudo-anonimization. Participants were contacted one month later by telephone to assess UI impact on their life.
Variables
Independent variables collected included adolescents’ demographic characteristics (age, gender, previous diseases) and accident context and characteristics (place, week day, association with alchool or drug use). Dependent variables included accident type, affected body region, diagnostic complementary exams performed, required treatment and follow-up, and school absenteeism.
Statistical analysis
Descriptive and inferential statistical analysis was performed with SPSS version 22 (IBM Statistics) considering a p value of 0.05 as statistically significant. Normality tests were performed for continuous variables, with parametric or non-parametric tests conducted accordingly. Categorical variables were assessed by Chi-square test. McNemar and Mann-Whitney tests were used to investigate differences between hospitals.
Results
A total of 1054 adolescents from the two hospitals consented to participate in the study (Figure I). In hospital A, a total of 6632 adolescents were evaluated in the ED throughout the 12-month study period, 1727 of which due to UIs. Therefore, this study allowed to identify 48.6% of UIs in adolescents in this hospital. Data for this analysis was not provided in hospital B. No statistically significant differences were found between hospitals regarding patients’ demographic characteristics, accident context, characteristics, and type, affected body region, diagnostic complementary exams, treatment and follow-up, or school absenteeism, thus corresponding data was jointly analyzed.
Figure I shows cohort distribution according to hospital, gender, and adolescence stage. Patients’ median age was 13 years (range 12−15). Prevalence of each accident type was independent of gender (p=0.17), although they were globally more frequent among males compared with females. Accident type varied according to adolescence stage (p <0.001). A higher prevalence of accidental falls and traumatic injuries was reported in early adolescence, whereas burns, traffic accidents, and intoxications were more frequent in middle adolescence. A lower prevalence of all accident types was reported in late adolescence.
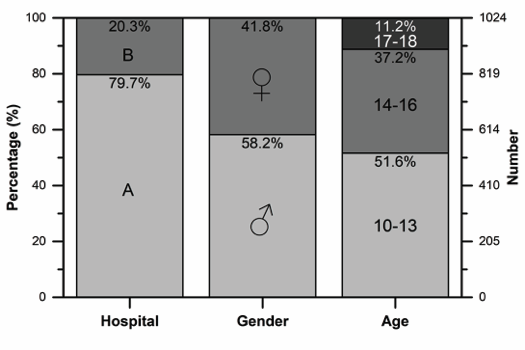
Figure I Patients included in the study according to hospital of origin, gender, and adolescence stage (early, 10 to 13 years old; middle, 14 to 16 years old; and late, 16 to 18 years old)
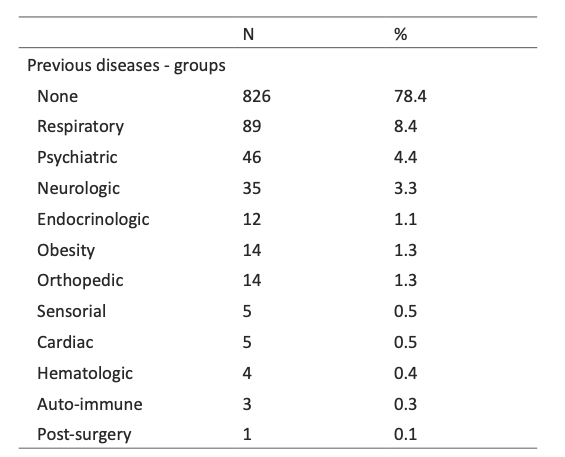
Distribution of previous diseases according to disease groups is depicted in Table I. No statistically significant differences were found between type of accident and previous diseases (p=0.99).
Most (83.6%, n=881) adolescents were brought to the ED without previous referral, but 11.7% (n=123) had been refered by the National Institute of Medical Emergency, 3.4% (n=36) by another hospital, 1.1% (n=12) by their pediatrician, and 0.2% (n=2) by linha saúde 24 (national health telephone line).
All adolescents were asked whether having consumed alcohol or drugs before the accident, with a self-report of alcohol or drug consumption of 2.3% (n=24). Of these, 1.9% (n=20) had consumed alcohol, and 0.4% (n=4) drugs. Most patients (1.9%; n=20) reported using these substances on school days rather than on weekends or holidays. Consumption was higher among males (p=0.03).
Groups of previous diseases included: respiratory (asthma - 56, 5.3% -, rhinitis - 33,3.1%), psychiatric (anxiety - 4, 0.4% -, depression - 4, 0.4% -, attention-deficit/hyperactivity disorder - 38, 3.6% -, opposition conduct disorder - 1, 0.1%), neurologic (cognitive deficit - 14, 1.3% -, epilepsy - 11, 1% -, migraine - 6, 0.6% -, cerebral palsy - 2, 0.2% -, Duchenne distrofy -1, 0.1%), endocrinologic (type 1 diabetes mellitus - 7, 0.7% -, thyroiditis - 2, 0.2% -, delayed puberty, policystic ovary syndrome, and precocious puberty - 1, 0.1% each); obesity - 14, 1.3%; orthopedic (hip or knee pain - 6, 0.6% -, plano-valgus feet - 4, 0.4% -, talipes equinovarus - 3, 0.3% -, feet syndactyly - 2, 0.2%), sensorial (hearing loss - 3, 0.3% -, visual acuity loss - 2, 0.2%), cardiac (congenital cardiopathy - 5, 0.5%), hematologic (anemia - 3, 0.3% -, hypogammaglobulinemia - 1, 0.1%), auto-immune (inflammatory bowel disease - 1, 0.1% -, auto-immune hepatitis - 2, 0.2%), and post-surgery (arteriovenous malformation - 1, 0.1%)
UI characterization
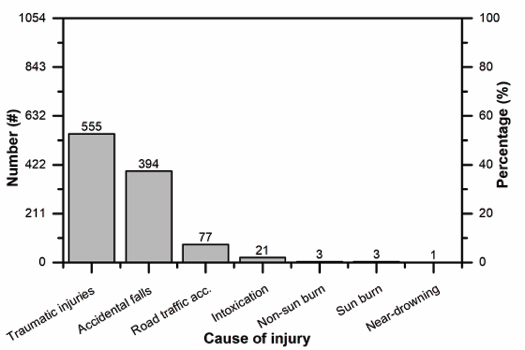
UI distribution is shown in Figure II. Most accidents (86.9%; n=916) took place on weekdays, with only 13.1% (n=138) occurring on weekends (p <0.001). Most (85.1%; n=897) happened during school hours, with a small percentage (12.4%; n=131) occurring on holidays (information was missing for 2.5% [n=26] of cases). UI frequency according to place of occurrence is described in Figure III.
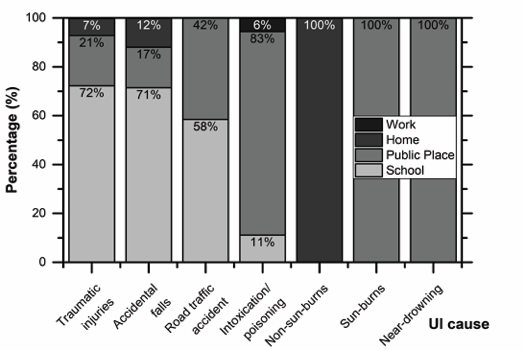
Figure III Relative UI frequency according to place of occurrence (work, home, public place, or school)
No traumatic injury was reported to be associated with alcohol or drug consumption. Most (72.3%; n=401) took place during school sports, followed by sports outside school, 24.5% (n=136) were violence-related, and 1.8% (n=10) were due to object fall, 1% (n=6) to electric chainsaw use, and 0.2% (n=1) to dog bite.
Most accidental falls (71.1%; n=280) happened at school, with 16.5% (n=65) occurring at a public space and the remaining (11.9%; n=47) at home. Most falls (86%; n=339) were from own height, 7.9% (n=31) of which from 1.5 to 2 meters and 1.8% (n=7) from more than 2 meters high. Two adolescents (0.5%) reported being under the effect of alcohol, and one (0.3%) under the effect of drugs.
Most road traffic accidents (58.4%; n=45) were reported on school days, on the journey to and from school, followed by 41.6% (n=32) on holidays. Most (77.9%; n=60) occurred in urban areas, and the remaining 16.9% (n=13) in rural areas (data was missing for 5.2% [n=4]). Alcohol use before the accident was reported by 2.6% (n=2) of adolescents, and drug use by 1.3% (n=1). A total of 37.7% (n=29) of adolescents were pedestrians crossing the street, 29.9% (n=23) were passengers on a motor vehicle, 20.8% (n=16) were bicycle riders, and 11.7% (n=9) were motor vehicle drivers. Use of seat belt or helmet (in a car or a motorcycle, respectively) was reported in 91.3% (n=21) of passengers on a motor vehicle and in 100% (n=9) of drivers. Helmet use was reported by 31.3% (n=5) of bycicle riders, with 68.8% (n=11) not using it.
Intoxication or poisoning was attributed to alcohol in 76.2% (n=16) of cases and to drugs in 9.5% (n=2). Of these, 71.4% (n=15) cases happened in public spaces, 9.5% (n=2) at school, and 4.8% (n=1) at work. Three (14.3%) cases were due to carbon monoxide inhalation and occurred at home. Most intoxications (57.1%; n=12) took place on weekdays, and 42.9% (n=9) on weekends.
Both non-sun and sun burns were reported on holidays. Non-sun burns happened at home, two by burning water and one by burning oil. Sun burns took place in public spaces (beach), were associated with no sunscreen use, and had a median sun exposure time of 4 hours.
The single near-drowning event was reported by an adolescent who could swim and took place in a cold-water private pool with lifeguard surveillance. The episode happened during holidays, with an imersion time of about five minutes and reanimation on scene.
No accidental use of fire weapons was reported.
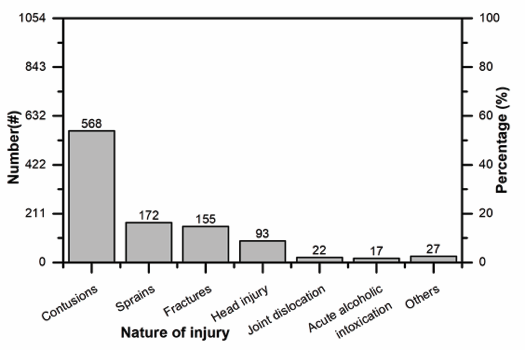
UI frequency according to their nature is shown in Figure IV. Most contusions, sprains, fractures, head injuries, and joint dislocations were associated with traumatic injuries (p <0.001; Chi-square Test).
The most frequent body region affected was the lower limbs (38.4%; n=405), followed by the upper limbs (36.6%; n=386), head (11.6%; n=122), spine (4.3%; n=45), thorax (2%; n=21), and abdomen (0.7%; n=7). Polytrauma was described in 6.4% (n=68) of cases. Isolated lesions on the lower limbs, upper limbs, head, thorax, and abdomen were more frequent with traumatic injuries, whereas polytrauma was more prevalent after accidental falls and road traffic accidents (p<0.001; Chi-square Test).
Most cases (50.7%; n=534) were classificated as urgent, 41.2% (n=434) as standard, 7.1% (n=75) as very urgent, and 1% (n=11) as non-urgent, according to Manchester triage system. Being referred by a health professional was associated with higher Manchester triage assessment (p<0.001), but this does not necessarily reflect clinical severity, as it is an expected software outcome whenever a patient is referred.
Glasgow coma scale score was 15 in 97.2% (n=1024) of adolescents, 14 in 1.4% (n=15), 13 in 0.5% (n=5), 12 in 0.6% (n=6), 10 in 0.2% (n=2), 8 in 0.1% (n=1), and 7 in 0.1% (n=1). Glasgow coma scale score was inferior (≤13) regarding intoxications compared with other accident types (p <0.001; Chi-square Test).
The most common diagnostic complementary exams were imaging exams (82.5%; n=870) and blood workup (1.6%; n=17). Most exams (91.8%; n=814) were normal and 8.2% (n=73) revealed abnormalities. Imaging exams were mainly performed in adolescents with traumatic injuries, acidental falls, or road traffic accidents, whereas blood workup was more frequent after intoxications (p <0.001; Chi-square Test).
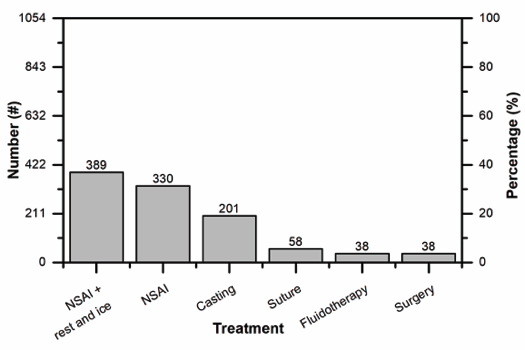
Treatment following UIs is depicted in Figure V. When analyzing required treatment for each case, most severe cases should be emphasized. Of these, two were due to traffic accidents in which adolescents were run over by a car, resulting in skull fracture in one case and hemoperitoneum in another, both requiring surgery. Two other cases resulted from accidental falls from an over 2-meter height, causing cranial and limb fractures, both requiring surgery. The last case resulted from a sports traumatic injury, causing limb fracture and also requiring surgery. Given injury complexity (requiring a neurosurgery team) and the need for mechanical ventilation, the first three cases were transferred to Intensive Care Units.
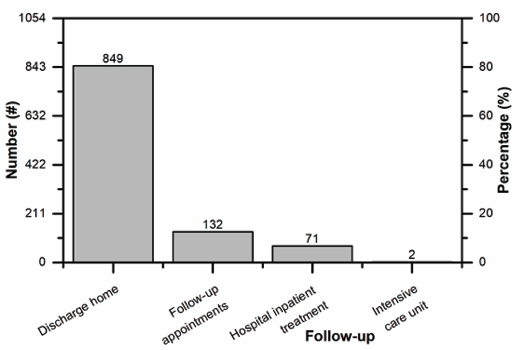
Follow-up upon discharge from the ED is shown in Figure VI. Adolescents were referred to medical follow-up appointments due to fractures (54.5%; n=72), head injuries (16.7%; n=22), contusions (12.9%; n=17), joint dislocations (6.1%; n=8), acute alcoholic intoxication (3.8%; n=5), sprains (3.0%; n=4), drug intoxication (1.5%; n=2), ligament rupture (0.8%; n=1), and piercing ingestion (0.8%; n=1). Inpatient treatment was mainly necessary in cases of injuries requiring cast immobilization (47.9%; n=34), surgery (33.8%; n=24), and fluidotherapy (18.3%; n=13). Two adolescents were transferred to other hospitals with Intensive Care Units due to head injury following a road traffic accident (bycicle rider) and traumatic injury during sports, respectively.
All adolescents included in this study survived.
School absenteeism resulting from UIs was reported in 31% (n=327) of cases. School absence duration is shown in Figure VII. UIs associated with school absenteeism included traumatic injuries (49.5%; n=162), acidental falls (40.1%; n=131), road traffic accidents (8.9%; n=29), intoxications (1.2%; n=4), and non-sun burns (0.3%; n=1). School absenteeism was not gender-dependent (p=0.83; Chi-square Test), but was higher in early adolescence (55.7%; n=182) compared with other adolescence stages (p=0.006; Chi-square Test). Main injuries resulting in school absenteeism were traumatic injuries (49.8%; n=163), followed by falls (40.1%; n=131). Longer absenteism (> 30 days) was due to head trauma (50.0%; n=4), hemoperitoneum (37.5%; n=3), and limb fractures (12.5%; n=1).
Discussion
Globally, injuries are considered avoidable and preventable, given the increased awareness and implementation of effective measures at the national level.3,8,9 A 2016 Cochrane review assessed the effects of school-based educational programes on injury prevention in children and showed that most studies had bias risk across multiple domains, retrieving only weak evidence suggesting that such programmes could improve safety skills, behavior, and knowledge.25
Alonso Fernández et al analyzed data from the Spanish National Health Surveys conducted in 2003, 2006, and 2011 including children aged 6 or above, and showed a higher prevalence of UIs in boys. This study further reported a higher frequency of UIs in the “workplace or place of study”. To reach these conclusions, data was retrieved from emergency centres, general practitioners’ consultations, and registered nurse information, what differs from the present study and overcomes one of its main limitations. This Spanish study showed that UI risk signifcantly decreased over the years, which could be related to preventive measure and policy implementation.6
The current study showed that 26% of adolescents assessed in hospital A ED had UIs. Considering that UIs are mostly preventable, it shows that there is room for improvement.
Regarding gender, the trend observed was consistent with other studies, despite not showing statistically significant diferences.6,7,10,26
When looking at different adolescence stages, middle adolescence was associated with a higher frequency of burns, road traffic accidents, and intoxications, which is in agreement with previous WHO reports.3,9 The reasoning behind this might be that in this stage there is still some inability to fully perceive risks and their future implications, increasing autonomous decision making, along with a sense of invulnerability.4,5,12,13 In contrast, late adolescence is characterized by improved impulse control and risk assessment, showing the lowest UI frequency.4,5 About half of UIs took place during early adolescence and 90.1% were either traumatic injuries or accidental falls. Therefore, a higher prevalence of these injuries was observed at this adolescence stage, which was also related to higher school absence rates.
When analysing UI causes, it becomes clear that most could have been avoided. Most traumatic injuries happened during school sports, and acidental falls took place mostly at school, which could have been prevented through better surveillance and sport pavillion improvement. Characteristics of road traffic accidents showed that using helmets or seat belts and stopping at crosswalks are basic measures for which awareness should be raised. In fact, when looking at bycicle riders, only close to one third revealed using appropriate personal protection equipment.
Even though consuming alcohol and using drugs is ilegal at ages considered in this study, 2.3% of participants reported using these substances, supporting the need to better supervise and accordingly refer this at-risk population. Non-sun and sun burns should also have been easily prevented through adequate protection while cooking and exposing to sun, respectively.
Most UIs were assessed through diagnostic complementary exams, and even though the majority did not require clinical follow-up, 19.4% did, with 6.7% requiring hospital inpatient treatment, and 0.2% requiring Intensive Care Unit admission. Not only these, but also school absenteeism reported in nearly one third of adolescents, represent important costs for the National Health System.
Study limitations
Most reported accidents took place at school and during school hours and required activating health insurance in school accidents, which may have led to an overestimate of accidents in this setting.
This study included only adolescents requiring ED evaluation, what may have underestimated the real frequency of UIs in this age group.
Questionnaire applied relied on alcohol and drug use self-report, what may also have underestimated their real frequency. Drug use was only verified through laboratory analysis in 18 out of 24 cases reported when there was cognitive impairment or a high index of suspicion regarding alcohol or drug use.
Socio-economic status, school performance, and previous school absenteeism were not evaluated, but could have been important in characterizing this population, given the higher UI frequency reported in lower social classes.
Conclusions
Overall, reported UI cases had preventable causes and could have been avoided, resulting in less ED admissions, diagnostic complementary exams, hospital inpatient admissions, and school absenteeism.
This study’s findings may contribute to planning and implementation of preventive, developmentally appropriate measures suitable for this at-risk population.
Further studies should assess prevalence and effectiveness of preventive measures on a nation-wide basis, as well as UI impact on quality of life.