Introduction
Physical examination is a fundamental part of children’s regular clinical evaluation and often one of the most useful and effective tools for establishing a specific diagnosis. Findings in physical examination of the external genitalia in children are often a source of concern for parents and caregivers, not only for the emotional significance attributed to these structures (partly due to their reproductive function), but also for the physical and psychological impact in the child.
In most cases, anomalies in the external genitalia are only normality variants and/or do not significantly affect function, therefore requiring only clinical surveillance and no intervention. However, some cases require medical intervention, either from a therapeutic or specialized point of view, and early intervention is key for the success of implemented measures.
Due to to the child’s close monitoring and periodic surveillance, the family physician has a crucial role in identifying and initially guiding these cases. By often being the first person to diagnose these anomalies and the first line of support for parents and caregivers, the family physician should acknowledge the specific guidelines regarding each case, not only for reassuring parents in cases without pathological significance, but also for properly referring the child to secondary health care when necessary.
Objectives
The aim of this work was to review available evidence on the main male external genitalia anomalies in pediatric age and discuss their accurate diagnosis, approach, and follow-up in primary health care. For being a more uncommon entity spectrum with highly variable, specific, and complex multidisciplinary approach, anomalies related to sexual differentiation (intersex) disorders are beyond the scope of this article.
Changes in physical examination of the male genital tract
Balanopreputial adhesions
Balanopreputial adhesions consist of physiological adhesions between the inner face of the foreskin and the outer face of the glans, being present in most newborns.1 Contrarily to what happens in phimosis, in balanopreputial adhesions there is no stenotic ring when the foreskin is retracted. They usually do not require treatment, spontaneous resolving with age. Natural detachment of adhesions and gradual preputial ring increase occur with smegma production and spontaneous erections.2-4 Foreskin retraction should be gradually and delicately performed to avoid excessive and forced detachment that may elicit continuity lesions, with consequent cicatricial phimosis risk.3
Smegma Pearls
Smegma is a physiological substance produced by the foreskin and glans mucosa, composed of desquamating epithelial cells and sebaceous substance.2 It should not to be confused with purulent exudate, usually associated with pain and local inflammatory signs.2 Smegma pearls consist of a benign collection of smegma in the subpreputial space, being common in uncircumcised boys with partial balanopreputial adhesions.28,29 It is a benign finding with spontaneous resolution.28,29
Phimosis
Phimosis is defined as the inability to completely retract the foreskin due to a constrictive preputial ring, hindering the total exposure of the glans.2 It is present in most newborns, gradually decreasing with age.4 Phimosis is classified into two types: physiological and pathological.3,4 During the diaper period, until around two years of age, physiological phimosis is believed to have a protective role of the glans and no additional care is required beyond normal hygiene.5-7 Pathological phimosis occurs as a consequence of aggressive and precocious prepuce manipulation, with anomalous preputial meatus scarring. It may also be secondary to inflammatory and infectious processes.8
Medical treatment can be started at the age of three years, when there are important adhesions with little probability of spontaneous resolution, or in presence of repetitive balanitis (Figure 1).9 Application of a topical corticosteroid − as 0.05% betamethasone cream − twice daily for four to six weeks, associated with non-traumatic retraction of the foreskin and hygiene care, are usually effective.8-10
The Portuguese General Health Board recommends surgical treatment after the age of five years, with circumcision being the most commonly used technique.11 Referral to pediatric surgery should occur early in cases of history of urinary tract infection (UTI), congenital malformation of the excretory system, repetitive balanitis, or urinary retention, since phimosis resolution decreases bacterial colonization of the glans and foreskin, thus reducing the probability of subsequent infections.2
Paraphimosis
Paraphimosis results from excessive retraction of the foreskin beyond the coronal groove without its replacement on the glans, causing a stenotic ring that decreases venous return and arterial supply to the glans.12 This vascular compromise causes edema, redness, intense pain and, in extreme cases, ischemia and necrosis, and represents a surgical emergency requiring immediate treatment.12 Diagnosis is clinical and treatment consists of immediate manual reduction.13 A topical anesthetic may be applied during the procedure for pain relief.12,13 If manual reduction is not effective, the subsequent treatment is surgical, aiming at dorsal venous discharge.13 Circumcision is usually not a therapeutic option in the acute phase, due to significant tissue edema with potential impact on subsequent healing and suture dehiscence risk. Nevertheless, it should be performed at a later phase to prevent recurrent episodes.12
Epispadias
Epispadias is a rare genital malformation in which the urethral meatus is located on the dorsal surface of the penis.14,15 It most frequently occurs in association with bladder exstrophy (exstrophy-epispadias complex) 15,16, with urinary incontinence being one of the main complications.14,17 Treatment is surgical and should be considered in view of the condition’s severity and associated complications.17
Hypospadias
Hypospadias is a congenital malformation in which the urethral meatus is located anywhere on the ventral surface of the penis, from the glans (40−50% of cases) to a more proximal position (Figure 2).2,18 As a general rule, the more proximal the meatus position is, the more severe the hypospadias degree, and this evaluation should be considered to decide on the surgical correction.2,19,20 Diagnosis is clinical and other physical findings are usually associated, as ventral curvature of the penis and emergence of a dorsal hooded prepuce (preputial skin over the dorsal surface of the penis) .18,19 Presence of other congenital anomalies, such as unilateral or bilateral cryptorchidism, should raise suspicion of a sexual development disorder.21
Surgical treatment consists of urethroplasty. It is indicated in cases of functional impairment and should be considered from the age of six months onwards, taking into account the specific features of each individual case .19,22 Prognosis is usually favorable from an esthetic and functional point of view, being always necessary to explain caregivers the potential postoperative complications, which can motivate future corrective surgical interventions.20,21
Hypospadias is a very rare congenital malformation consisting of two “true” urethral openings, in which the ectopic meatus corresponds to the functional urethra.18,23 Urethral duplication includes a wide spectrum of anatomical variants in which the urethra can be partially or completely duplicated.24 Likewise, the clinical presentation is also variable: patients may be completely asymptomatic or have associated abnormalities, such as double-flow, urinary incontinence, outflow obstruction, or recurrent urinary infections.24,25 Treatment is surgical and depends on the type of duplication, clinical manifestations, and coexistence of other associated abnormalities.24,25
Short Frenulum (Frenulum Breve of the Penis)
Short frenulum causes a ventral curvature of the penis and may cause pain during preputial retraction or erection.26 If symptomatic, it requires surgical correction (frenuloplasty).27
Cryptorchidism
Cryptorchidism refers to the absence of one or both testicles from the scrotal sac and represents the most common congenital abnormality of the genitourinary tract.30,31 Cryptorchidism includes different clinical entities, as undescended testicles (most common), retractile testicles, testicular ectopy, and absent testicles.32 Clinical history is crucial to guide the subsequent therapeutic approach, being important information whether testicles were palpable during the neonatal period and whether there is a history of inguinal surgery or relevant family history, among other aspects.32 Clinical examination is equally important. An empty scrotal sac, hypoplastic and poorly rugated, may indicate that the testicle was never in the scrotum.32 It is crucial to know whether cryptorchidism is uni or bilateral, if there are other associated genital tract anomalies (as hypospadias, often suggestive of a sexual development disorder), and if there are findings suggestive of endocrinologic, metabolic, or genetic pathology.33,34 Cryptorchidism diagnostic and therapeutic approach depends on whether the testis is palpable or not.30,35 Usually, undescended testicles complete their descent into the scrotal sac in the first four months of life, with spontaneous descent rarely occurring after this period.31 Imaging tests, as ultrasound, are usually not necessary, since they do not obviate the need for exploratory surgery.30,32 Regardless of whether testicles are palpable or not, cryptorchidism management holds better prognosis when carried out in the first year of life.36,37 Therefore, referral should occur as early as possible after the age of four months.32
Undescended testicles
Condition in which the testicles do not complete the normal descent into the scrotal sac, being more often unilateral than bilateral.36,38 Undescended testicles can be palpable or nonpalpable. Unilaterally nonpalpable testicles are predominantly left-sided.32 Nonpalpable testicles always require laparoscopic exploration to confirm presence of the gonad and attempt orchidopexy. If not feasible, orchidectomy is mandatory. Testicular location in the inguinal canal or abdominal cavity exposes the testicles to higher temperatures, conditioning an increased risk of infertility and testicular malignancy.30,35,38,39 Undescended testicles are associated with an increased risk of torsion, trauma, and psychological disturbance31,35,36,40 and have a high percentage of spontaneous resolution during the first six months of life.36 After this age, spontaneous resolution is uncommon and surgical treatment may be required. Surgical treatment (orchidopexy) is currently recommended between the age of six and 18 months.36 Orchidopexy is able to reduce but not prevent potential long-term complications, particularly testicular cancer, reason why ongoing clinical follow-up is essential.
Retractile testicles
Non-pathological, often bilateral condition, in which the normally descended testicles temporarily rise to a suprascrotal position due to cremasteric reflex.35 The differential diagnosis from undescended testicles is established by pulling the testicle to the scrotal position and confirming that it holds the position when loose. In most cases, spontaneous resolution occurs until puberty onset and only clinical annual surveillance is required.31,36 Annual follow-up until puberty is necessary, since this entity occasionally evolves to acquired undescended testicles, requiring corrective orchidopexy.
Ectopic testicles
In this condition, testicles are absent from the scrotal sac and located outside their normal descent path.32,36 Potential complications include blunt trauma from compression against the pubic bone and diminished spermatogenesis.32 Association with malignant transformation is not consensual32 and surgical exploration is usually required for diagnosis and treatment.41
Anorchia (congenital absence of testicles)
Anorchia may result from testicular agenesis or atrophy secondary to intrauterine vascular compromise (due to prenatal testicular torsion − “vanishing testis syndrome”).32,36 Exploratory laparoscopy is mandatory for diagnostic confirmation.36
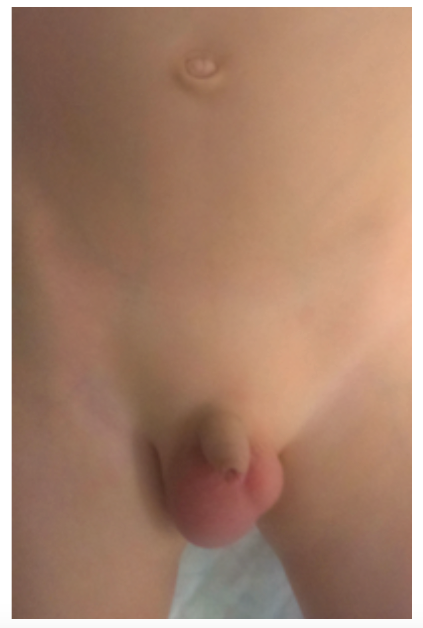
Hydrocele
Hydrocele is a very frequent condition in newborns in which fluid accumulation occurs between the visceral and parietal layers of the vaginal tunic of the testicles, being perceptible by transillumination of the testicular sac.42 Resolution is spontaneous and considered physiological until the age of two years.42 Hydrocele can be classified as communicating or non-communicating. In the first (Figure 3), peritoneal fluid accumulation around the testicles occurs as a consequence of late processus vaginalis closure and is usually characterized by volume variation throughout the day: in the morning, hydrocele is smaller, becoming progressively larger by the end of the day.42,43 In non-communicating hydrocele, processus vaginalis has already closed or narrowed. Sometimes there is no communication with the peritoneum and fluid accumulation may be idiopathic or secondary to testicular inflammatory/pathological processes (reactive hydrocele). In these cases, there is usually associated pain.42,43
Diagnosis is clinical. However, in an acute setting, particularly with associated pain, scrotal ultrasound may be useful in the differential diagnosis with inguinal hernia or testicular torsion. Due to the high probability of spontaneous resolution within the first 24 months of age, surgical treatment is not indicated before this period, except in cases in which an inguinal hernia is also present or suspected (such as in communicating hydroceles), which require earlier intervention.42
Varicocele
Varicocele is an abnormal and tortuous dilation of the pampiniform plexus veins, more common on the left (around 85−95% of cases).42,44 It is due to the anatomical difference between left and right testicular veins, the first entering the left renal vein at a 90 degree angle, and the second draining at a more obtuse angle directly into the inferior vena cava, facilitating more continuous flow.42 Varicocele can be subdivided into primary and secondary type. Primary/idiopathic varicocele, the most common, occurs spontaneously by incompetence of the venous valves, being more prominent in orthostatism and with the Valsalva maneuver and reducing in dorsal decubitus position.42,43 Secondary varicocele results from extrinsic compression and obstruction of the inferior vena cava, is generally of acute onset, and persists in the dorsal decubitus position.42,43 Clinically, varicoceles may present as asymptomatic findings or be associated with a sense of weight and scrotal pain that aggravate with orthostatism.42 If there is clinical suspicion of secondary varicocele (in cases that varicocele persists in the supine position, has an acute onset, or is located on the right side or bilaterally), ultrasound and abdominal computed tomography should be performed to exclude obstruction from a retroperitoneal mass compressing the vascular structures.45
Grade I varicocele is not visible and only palpable with Valsalva maneuver, grade II varicocele is visible in orthostatism only with Valsalva, and grade III varicocele is always visible in orthostatic position, even without Valsalva maneuver.
Varicocele is a common pathology in adolescence (10−15%), frequently associated with infertility in adulthood. Most varicoceles require no specific treatment, with only clinical follow-up and symptomatic treatment recommended. Surgical correction in adolescence is not unanimous. Open or laparoscopic surgical treatment with ligation of spermatic vessels is indicated in cases of grade II or III varicocele associated with more than 2 mL or 10% decreased testicular volume or evident symptoms of pain and discomfort that alleviate in supine position and bilateral varicocele. 42,44
Spermatocele (epididymal cyst)
Spermatocele consists of a cyst of variable dimensions located in the epididymis head with a liquid, painless content that may contain nonviable sperm.42 On physical examination, a cystic mass adjacent to the testicular structures is palpable.42 This entity is sometimes accidentally diagnosed during testicular ultrasound, considering that when a scrotal lump is found during clinical examination this radiological exam can be useful to confirm diagnosis. Spermatocele is not a cause of infertility and surgical treatment is only indicated for symptom relief.42
Conclusion
Physical examination is a crucial part of child assessment. Alterations in the physical examination of the external genitalia are frequently not pathological, having favorable prognosis and requiring no more than clinical surveillance. Conversely, some situations require specialized evaluation and sometimes surgical correction, and should therefore be referred to hospital consultation and follow-up.
The family physician, as a primary element of the child’s clinical follow-up, is often the first to diagnose these abnormalities and should be able to recognize those that are benign from pathological and requiring formal secondary care referral.
The anxiety that many of these changes elicit in caregivers should also deserve attention from the family physician, who should reassure that clinical issues are being properly addressed.