Introduction
Pustular eruptions are common in the neonatal period. The differential diagnosis is varied and includes infections, benign self-limited conditions, hereditary disorders, and other diseases.1 Differentiating between benign and transitory eruptions and severe and potentially fatal cases is crucial. Congenital candidiasis is a rare disorder included in this differential diagnosis.
Candida infection in the newborn can be divided in two forms: congenital and neonatal. Congenital cutaneous candidiasis (CCC) is an intrauterine infection and neonatal candidiasis is acquired when the baby goes through a contaminated vaginal canal. In both forms, the etiological agent is the Candida species, a pathogen found in the vaginal canal of at least 20% of women, rising to 30% in pregnancy.2 Despite this, congenital candidiasis seems to be an extremely rare condition of the term or preterm newborn.3
Invasive candidiasis describes all disseminated Candida infections, including candidemia (Candida isolation in blood cultures) and single-organ infections. Newborns with invasive candidiasis are most often extremely premature and immunocompromised.4 Congenital cutaneous candidiasis diagnosis is established through microscopic examination of skin scrapings and confirmed by fungal culture of lesions, umbilical cord, and/or placenta if available.5-7
CCC treatment remains controversial and is largely based on case reports.4,6 The condition is topically treated with azole agents, as miconazole or clotrimazole. Lesions peel off and disappear without residue, lasting approximately two weeks. Invasive candidiasis recognition treatment initiation are crucial for prognosis. Intravenous amphotericin B is the recommended drug.7,8
Case report
A 3200-g term female infant was born with vacuum extraction to a 32-year-old primigravida. The mother was diagnosed with Candida vulvovaginitis during pregnancy and received antifungal topical treatment, without symptom resolution. Maternal serological tests and viral markers, including hepatitis B virus surface antigen (HBsAg), human immunodeficiency virus (HIV), venereal disease research laboratory test (VDRL), rubella virus and toxoplasmosis in the third trimester showed no evidence of acute infection. Maternal group B streptococcus screening was negative. Membranes ruptured four hours before delivery and amniotic fluid was reported as having foul smell. Apgar scores were 9 and 10 at 1st and 5th minutes, respectively.
At birth, the newborn had a foul smell but was otherwise well-appearing, vigorous, afebrile, and without respiratory distress. Her skin showed erythematous macules, vesicles and pustules involving the trunk and extremities, including the palms and soles. An exfoliating burn-like dermatitis was evident around the neck (Figure 1), with mucous membranes and skin folds being spared. The remainder physical examination was normal. After birth, the newborn was admitted to the Neonatal Care Unit for investigation and treatment. The placenta could not be recovered for macroscopic examination and culture.
Laboratory workup and serological tests were performed, viral markers were investigated, and skin, blood, and urine cultures were collected and the newborn was started on empiric treatment with ampicillin, gentamicin, and acyclovir.
Complete blood count revealed 31,580 white blood cells/µL (50.3% neutrophils and 31.9% lymphocytes). Serum C-reactive protein concentration was normal (0.10 mg/dL) and liver transaminases were also normal.
On the third day of life mycological culture of skin lesions was positive for Candida albicans, prompting systemic intravenous fluconazole and topical clotrimazole administration. As blood culture was positive for methicillin-sensitive Staphylococcus aureus, ampicillin and gentamicin were maintained for ten days. Urine Cultures were sterile. Acyclovir was suspended on the fifth day of life following negative serological tests and viral markers, including HIV, cytomegalovirus, and herpes simplex virus (HSV).
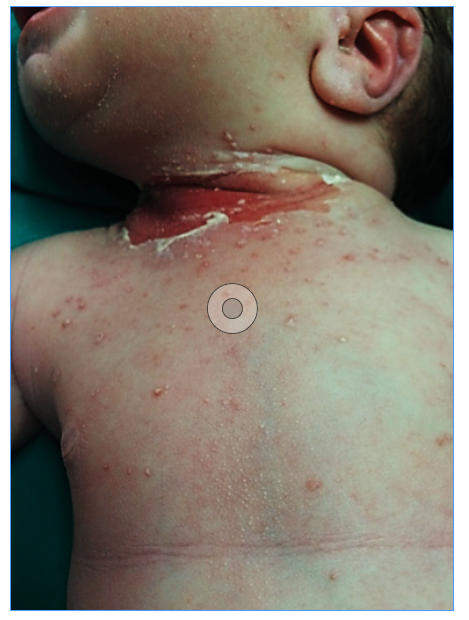
Figure 1 Erythematous macules, vesicles and pustules involving the trunk and cervical exfoliating burn-like dermatitis
The newborn remained well and thrived. At discharge, on the 12th day of life, lesion desquamation and absence of pustules or vesicles were evident and only slight erythema was present in the cervical region (Figure 2). Serial laboratory workup revealed a progressive WBC count decrease (13,940/µL at discharge).
Systemic fluconazole and topical clotrimazole were maintained for a total of 21 days. On the first follow-up visit, one month after discharge, no rash or skin lesions were observed. The newborn was well, with normal growth and neurodevelopment.
Discussion
Congenital cutaneous candidiasis is a rare intrauterine infection that may occur due to rise of Candida in the vagina, by penetrating the broken or intact pouch. Main risk factors include presence of foreign intrauterine bodies, such as intrauterine devices, or cervical cerclage.3Candida chorioamnionitis and peripheral funisitis with microabscesses are generally present.6 Lesions are present at birth or appear in the first 12 hours to six days after delivery.1,5 The rash generally spreads throughout the body, namely to the face, chest, back, extremities, and palms and soles, usually without oral or perineal region involvement. Lesions usually begin as macules and erythematous papules, which rapidly develop into pustules and vesicles. Rash may also develop as a bright red “burn-like” dermatitis, usually associated with positive cerebrospinal fluid, blood, and urine culture.4 Marked peeling with crusty exfoliations follows the acute phase.1
This type of candidiasis should be considered in the differential diagnosis of generalized neonatal maculopapular or pustular skin eruptions, along with other disorders such as Listeria monocytogenes infection, impetigo, varicella, herpes virus infection, syphilis and epidermolysis bullosa.1 For this reason, an extensive workup including laboratory and serology tests and cultures should be performed.
Although in this newborn skin lesions and maternal history of Candida vulvovaginitis were suggestive of congenital candidiasis, empiric treatment with antibiotic and antiviral agents was immediately started for other more common conditions, that can become severe when left untreated, including infectious causes of vesiculopustular skin lesions, as impetigo, group B streptococcal infection, varicella, and primary herpes virus infection. Additionally, foul smell at birth in an asymptomatic newborn and high WBC count (31,580/ µL) raised suspicion of an infectious cause. Because the newborn remained asymptomatic and there were multiple vesicles at the puncture site, lumbar puncture was not attempted in this case.
Cutaneous congenital candidiasis was confirmed after positive skin scraping culture for Candida albicans. Unfortunately the placenta could not be recovered for examination and culture to corroborate diagnosis.
It is acknowledged that the clinical course in full-term infants with congenital candidiasis and skin involvement only is often benign and the optimal treatment choice remains controversial.5 Systemic involvement is rare and more likely in extremely- and very-low-birth-weight (ELBW and VLBW) infants. An estimated 5 - 20% of ELBW newborns develop invasive candidiasis.7 Other factors that increase the risk of systemic disease include extensive instrumentation in the delivery room, invasive procedures on the neonate, and an altered immune response.5 Candidemia cannot be distinguished from bacteremia presentation easily, because signs and symptoms are often nonspecific and subtle and may include fever, lethargy, apnea, hypotension, respiratory distress, abdominal distension, hypertension, and poor feeding. 4 Definitive invasive candidiasis diagnosis requires organism isolation from a typically sterile body fluid or tissue (e.g., blood, cerebrospinal fluid, bone marrow, or biopsy specimen). However as blood culture is only 50% sensitive in some settings, a negative Candida species culture result does not exclude invasive infection.7
Systemic antifungal therapy should be considered in preterm newborns with VLBW and in all infants with respiratory distress and/or laboratory signs of sepsis, such as elevated WBC count with increase of immature forms or persistent hyperglycemia and glycosuria. Candida isolation from blood, urine, and/or cerebrospinal fluid cultures and/or presence of burn-like dermatitis should prompt systemic treatment.4,5
In the present case, a high WBC count, burn-like dermatitis, and instrumentation in the delivery room (vacuum suction) raised suspicion of invasive candidiasis. For this reason, systemic fluconazole in association with topical clotrimazole was started, even though the neonate was asymptomatic and blood and urine cultures were negative for Candida. Because the clinical course was benign and laboratory workup showed disease improvement, no other investigations, such as imaging exams, were performed. Nevertheless, target organ damage should be investigated in invasive candidiasis, namely through ophthalmologic examination and head, renal, and hepatic ultrasound. 4
Ampicillin and gentamycin were maintained, as blood culture for methicillin-sensitive Staphylococcus aureus was positive. Staphylococcus aureus infection can also present as vesicle-pustular skin lesions or bullae that rupture easily, commonly found in areas of trauma, such as the diaper area and skin folds.1
Amphotericin B deoxycholate (d-AMB) is the drug of choice for the treatment of neonates with systemic candidiasis, including meningitis. In candidemia, fluconazole is an alternative to d-AMB, provided the species is susceptible. The recommended treatment duration for uncomplicated candidemia is two weeks.6-8 In the present case, the benign disease presentation in a full-term newborn, led to the choice for fluconazole, which does not require prolonged venous access.
Most newborns, particularly full-term, follow a benign course and recover without long-term sequelae. On the other hand, invasive candidiasis is associated with prolonged hospitalization and neurodevelopmental impairment or death in almost 75% of affected ELBW infants.7
This report describes a case of congenital cutaneous candidiasis and Staphylococcus aureus bacteremia in a full-term infant, with successful recovery after treatment initiation. CCC rarity can lead to delayed diagnosis and unnecessary treatment and this report highlights that fungal infection should be considered in the differential diagnosis of vesiculopustular skin lesions in neonates. Due to the condition’s poor prognosis, systemic treatment should be initiated if invasive candidiasis is suspected.















