Imaging cases
Caso clínico imagiológico
Catarina Cristina1
Inês Serras1
Ema Santos2
Rui Alves2
Dulce Serrano1
1 Department of Pediatrics, Unidade de Portimão, Centro Hospitalar Universitário do Algarve. 8500-338 Portimão, Portugal, catarina.ccristina@gmail.com; inesserrasped@gmail.com; dulce_serrano02@hotmail.com
2 Department of Pediatrics Surgery, Hospital Dona Estefânia, Centro Hospitalar Universitário de Lisboa Central. 1169-045 Lisboa, Portugal, ema_js24@hotmail.com; ruialves252@gmail.com
Abstract
Hirschsprung disease is the most common congenital gut motility disorder and usually diagnosed in the neonatal period. It is caused by an aganglionic bowel segment resulting in absence of intestinal peristalsis and functional obstruction. Diagnosis should be considered in all patients with constipation that does not respond to conventional treatment. Radiography and contrast enema are important diagnostic exams, but the definitive diagnosis is established through histochemical analysis of aganglionic segment biopsy. Treatment is surgical and early recognition is important to avoid complications and improve prognosis.
Herein is reported the clinical case of a young infant presenting to the Pediatric Emergency Department with nausea, vomiting, constipation, refusal to feed, and important abdominal distension. Abdominal radiograph and contrast enema were compatible with Hirschsprung disease. Biopsy histochemical analysis confirmed the diagnosis and surgical treatment was performed.
Keywords: contrast enema; Hirschsprung disease; intestinal obstruction; meconium
Resumo
A doença de Hirschsprung é o distúrbio congénito de motilidade intestinal mais comum e habitualmente diagnosticado no período neonatal. É causado por um segmento intestinal aganglionar, que leva a ausência de peristaltismo intestinal e obstrução funcional. O diagnóstico deve ser considerado em todos os doentes com obstipação sem resposta ao tratamento convencional. A radiografia e o enema com contraste são exames importantes para o diagnóstico, mas este só é definitivamente estabelecido por análise histoquímica da biópsia do segmento aganglionar. O tratamento é cirúrgico e o reconhecimento precoce da doença é importante para evitar complicações e melhorar o prognóstico.
É reportado o caso clínico de um lactente que se apresentou no Serviço de Urgência Pediátrica com náuseas, vómitos, obstipação, recusa alimentar e uma importante distensão abdominal. A radiografia abdominal e o enema com contraste foram compatíveis com doença de Hirschsprung. A análise histoquímica da biópsia confirmou o diagnóstico e foi efetuado tratamento cirúrgico.
Palavras-chave: clister opaco; doença de Hirschsprung; mecónio; obstrução intestinal
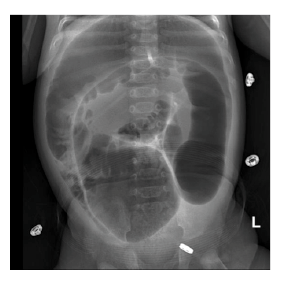
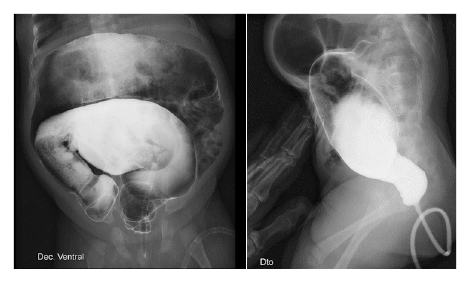
A two-month-old, previously healthy male infant was admitted to the pediatric Emergency Department with nausea, vomiting, constipation, and refusal to feed for two days. In the neonatal period, meconium passage with stimulation occurred at 18 hours of life. On admission, the infant had an important abdominal distension, bowel sounds, and painless abdominal palpation, with no palpable masses. Abdominal radiograph revealed exuberant bowel distension (Figure 1), with slight improvement after rectal decompression and exit of thick stools without blood or mucus. Contrast enema showed a recto-sigmoid transition zone with caliber inversion between the rectum and sigmoid (Figure 2).
What is your diagnosis?
Diagnosis
Hirschsprung disease
Patient orientation
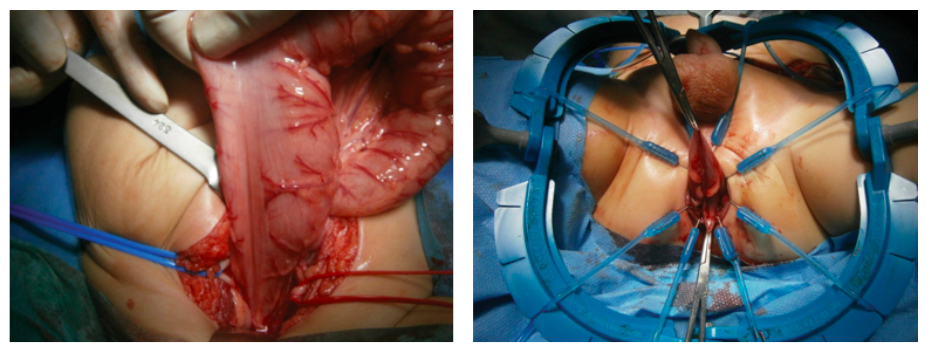
Contrast enema showed a recto-sigmoid transition zone (anatomical transition between the narrow distal aganglionic segment and the dilated proximal ganglionic segment), a pathognomonic finding of Hirschsprung disease (Figure 2). At seven months of age, extemporaneous histochemical analysis of sequential colonic biopsies revealed absence of ganglion cells in the sigmoid, compatible with Hirschsprung disease, and Swenson’s pull-through was performed (Figure 3).
Discussion
Hirschsprung disease is the most common congenital gut motility disorder, with a reported incidence of approximately one in every 5,000 live births and male preponderance (4:1).1-3 It is caused by failure of neural crest cell migration during intestinal development in fetal life or failure of neural crest cells to differentiate into mature ganglion cells, resulting in an aganglionic bowel segment that leads to absent intestinal peristalsis and functional obstruction upstream of the aganglionic zone.1-5 Rectum and sigmoid colon are the most affected segments.1-5 Diagnosis is suggested by meconium passage delay or history of constipation that does not respond to conventional treatment.1-5 Imaging exams, namely radiography and contrast enema, are important tools for early diagnosis.1-4 The definitive diagnosis is established through histochemical analysis of aganglionic segment biopsy showing absence of ganglion cells in the submucosal and myenteric plexus and, in most patients, hypertrophied nerve trunks.1
Hirschsprung disease treatment is surgical and involves resection of the aganglionic segment of the colon and reconstruction of the intestinal tract by bringing down the normal ganglionic bowel to the anus.2-5
Early recognition of this entity is important to avoid complications, such as Hirschsprung-associated enterocolitis, a potentially fatal pathology.1-5
Lessons from this clinical case
Hirchsprung disease is a congenital disorder that most commonly presents in the neonatal period as intestinal obstruction.
Diagnosis should be considered in all neonates or children with constipation that does not respond to conventional treatment.
Imaging exams are important tools for early diagnosis.
Early diagnosis decreases complications, improves prognosis, and positively impacts patients’ quality of life.
References
1. Nunes I. Doença de Hirschsprung. Trabalho Final do Mestrado Integrado em Medicina. Faculdade de Medicina de Lisboa. 2015/2016.
[ Links ]
2. Langer J. Hirchsprung Disease. Curr Opin Pediatr. 2013; 25:368-74.
[ Links ]
3. Wetherill C, Sutcliffe J. Hirchsprung Disease and anorectal malformation. Early Human Development. 2014; 90:927-32.
[ Links ]
4. Romaneli M, Ribeiro A, Bustorff-Silva J, Carvalho R, Lomazi E. Hirchsprung disease - Postsurgical intestinal dysmotality. Rev Paul Pediatr. 2016; 34:388-92.
[ Links ]
5. Wesson D, Lopez M. Congenital aganglionic megacolon (Hirchsprung Disease). Singer J, Hoppin A (editor). UptoDate 2018. [Consulted in August 2019]. Available in: https://www.uptodate.com/contents/congenital-aganglionic-megacolon-hirschsprung-disease.
[ Links ]