Introduction
Chronic otitis media with effusion (OME) is defined by the presence of fluid in the middle ear for more than 12 weeks in absence of acute inflammatory signs. It mostly affects children and is responsible for the most common surgical procedure in the ear, nose, and throat (ENT): placement of tympanostomy ventilation tubes (TT). In addition to the economic costs, the impact of the disease on children’s development and learning, the clinical consequences of the disease and its treatment, and the impact on quality of life must be considered.1
Nearly 33% of children in primary school and 20% of children younger than two years submitted to screening procedures test positive for OME.2,3
The most consensual OME treatment is TT placement, which enables not only fluid drainage but also tympanic cavity oxygenation.4 The American Academy of Otolaryngology-Head and Neck Surgery (AAO-HNS) clinical practice guidelines for TT placement were published in 2013 and represent an important consensus document resulting from many years of practice and experience sharing.5 The AAO-HNS clinical practice guidelines for OME, updated in 2016, represent a valuable complement to the former in this disease setting.6 More recently, the International Federation of Otorhinolaryngological Societies (IFOS) proposed a consensus statement very similar to the one from AAO-HNS, considering regional differences as minor and autoinflation as potentially beneficial for OME treatment.7
These guidelines are used as a reference, not only for otolaryngologists all over the world but also for other medical specialties treating children, such as Pediatrics or General Practice. However, clinical expertise and publications on the subject suggest that they do not consider regional specificities related to therapeutic alternatives, population socioeconomic conditions, or season.8-11 Therefore, doctors have the need to adapt their attitudes regarding OME to their environment. On the other hand, one must also remember that, regardless of the underlying cause, middle ear effusion may spontaneously resolve. For instance, after an acute otitis media episode, effusion resolves after three months in 74% of cases.12
Based on this information, this study’s authors hypothesized that the diagnosis, management, and therapeutic decisions of Portuguese ENT doctors regarding OME are based on international guidelines with adaptations regarding climatic and geographic features and sociological habits of the Portuguese population. For example, in Portugal students have the longest holiday period during summer, most public and private workers are compelled to have holidays during summer, and most people go to the beach at that time.
The main aim of this study was to evaluate the clinical practice of OME diagnosis and treatment by ENT practitioners working in Portugal. The most relevant international clinical guidelines for OME and TT are from AAO-HNS, which, despite being American, have an almost global application. However, regional differences exist between countries regarding climatic conditions and treatment methods. In this study, the authors proposed to assess a representative sample of ENT doctors working in continental and insular Portuguese territory, with different degrees of clinical specialization and Pediatric Otolaryngology backgrounds. The specific objectives of this study were to (i) evaluate the clinical practice of OME diagnosis and treatment of the ENT medical community working in Portugal; (ii) investigate whether the AAO-HNS international guidelines for OME are followed by ENT doctors working in Portugal; and (iii) investigate adjustments in clinical procedures performed by ENT doctors working in Portugal according to season or non-pharmacological treatments available in Portugal, as sea baths and crenotherapy.
Material and methods
An observational, descriptive, cross-sectional study was performed between January and December 2017. A questionnaire was developed based on AAO-HNS clinical practice guidelines about TT placement in children, by transforming each directive into a question. Additionally, questions were added to characterize OME diagnosis and treatment according to regional specificities, including:
-Usually, you don’t operate on children between… (you can select more than one option): 6 to 18 months // 18 months to 3 years // 3 to 6 years // 3 to 9 years // 9 to 12 years // My decision does not depend on age
-Usually you perform surgery in (you can select more than one option): Spring // summer // Autumn // Winter
-Do you wait for the end of the summer to decide on TT placement?
-Regarding treatment options, you recommend: Sea baths // Crenotherapy // Swimming indoors
-What are your drug treatment options for OME? Nasal corticoids // Systemic corticoids // Anti-histaminics // Alpha-amylase // Oral immunotherapy // Other
-Do you follow the AAO-HNS guidelines published in July 2013? If you answered NO, which ones do you not follow?
The questionnaire focused on children between six months and 12 years of age and was presented to a pilot group of 11 doctors of both genders with wide geographic distribution in the country and several degrees of specialization (including residents and heads of department). Processing of responses and suggestions reported by the group enabled questionnaire validation, which was subsequently applied in scientific events and clinical department meetings in paper form or by e-mail. Preliminary contact was made with ENT heads of department to explain the study subject and objectives and obtain authorization to conduct it. Data was processed in an aggregated and anonymous way.
Statistical analysis was performed with R software, version 3.3.2. All association tests were performed using chi-square or Fisher exact test, using a 5% significance level.
This research project obtained prior authorization from the Ethics Committee that oversees clinical investigation at Hospital da Luz - Lisboa.
Results
Data was self-reported by 281 doctors (about 47% of the Portuguese otolaryngologist population), 57% of whom were male and 41% female. Most respondents were younger than 40 (48.7%) and only 1.5% were older than 70 years.
The annual percentage of children in consultation was used to estimate the experience in the treatment of this condition in the pediatric population: only 8.6% of doctors were responsible for the follow-up of more than 60% of children annually (Figure 1). The high number of doctors still in the Otolaryngology internship (29.4%) was noteworthy.
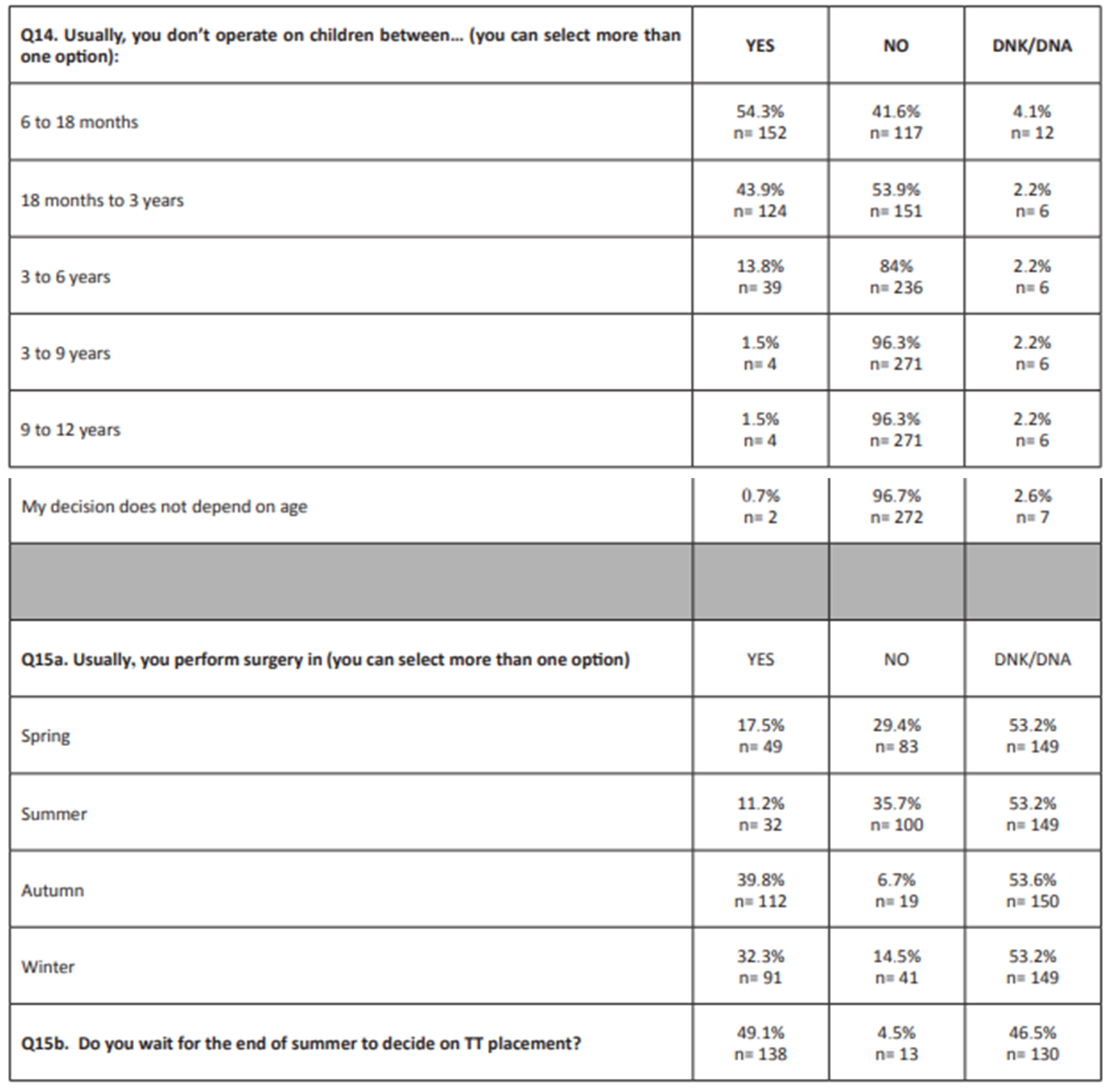
Answers to the questions on TT placement in children based on AAO-HNS guidelines were generally in accordance with the guidelines (Table 1). When questioned if they followed all guideline recommendations, 55.8% of doctors considered that they do, but also acknowledged the influence of other factors, such as children’s age at the time of the surgical indication. The surgical indication may also be influenced by season (Table 2).
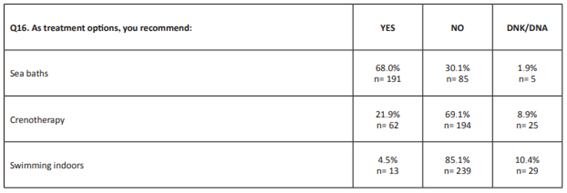
In Portugal, it is easy to reach the shore, there are multiple crenotherapy facilities with sulfurous water sources, and there is a generalized belief that going to indoor pools aggravates inflammatory respiratory episodes. Answers to whether these parameters were considered in OME recommendations are depicted in Table 3 and are according to the expected.
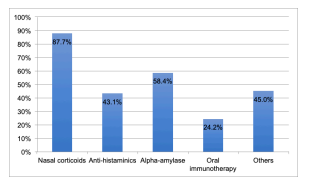
From a drug therapy perspective, current guidelines do not indicate a specific drug for OME treatment. Since there was a change regarding the previous recommendations, Figure 2 shows the current drug prescription profile for OME in Portugal.
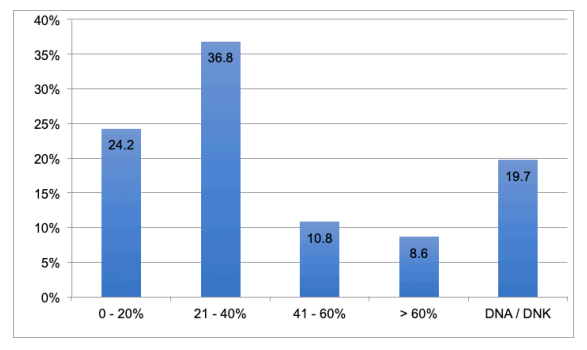
Figure 1 Annual percentage of children (six months - 12 years) followed in consultation. DNK/DNA: does not know/did not answer
Table 1 Questions based on AAO-HNS guidelines regarding TT placement in children
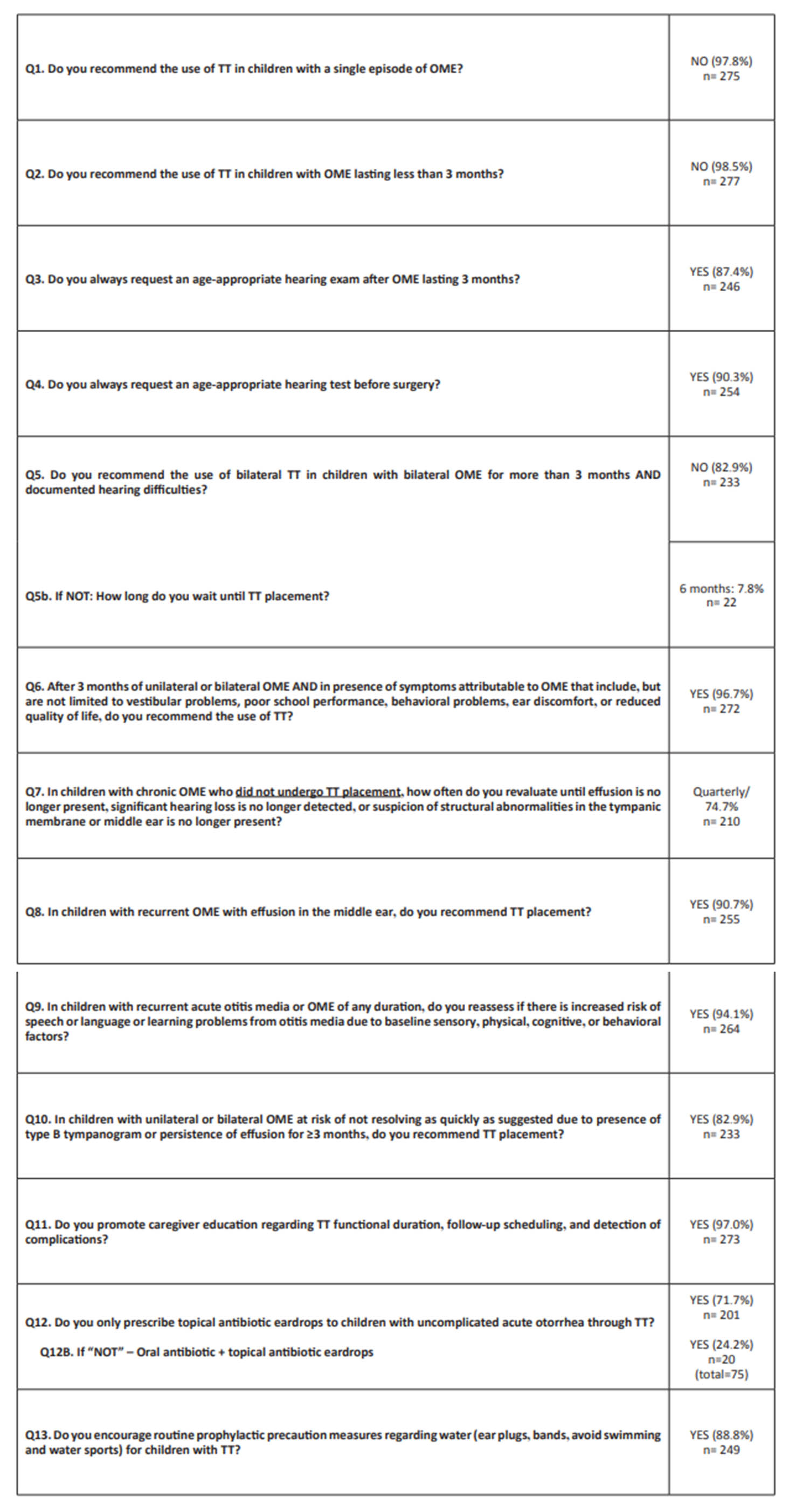
OME: otitis media with effusion; TT: tympanostomy tubes
Discussion
The number of answers retrieved in this study is relevant, given the population of approximately 600 doctors practicing Otolaryngology in Portugal. Questions labeled as “optional” were answered by 80% of the doctors surveyed.
In general, most answers agreed with the AAO-HNS guidelines. The exception was regarding the recommendation for preventive measures to avoid water entering the external ear canal of children with TT, with 88.8% of doctors promoting these measures despite guidelines recommending against them. This recommendation was statistically associated with being a specialist, having under 40 years of age, and working in non-coastal regions or the private sector (p< 0.05). This is an ancient recommendation made by doctors and the proposed change still lacks robust data.
The recommendation regarding bilateral tube placement in children with bilateral OME lasting for three or more months and with documented hearing difficulties was associated with having under 40 years of age, working in coastal regions, and working in the public sector (p<0.05), suggesting that younger doctors working in the public health system are potentially more likely to follow the guidelines.
The only “strong recommendation” in the guidelines concerned the sole use of antibiotic eardrops in otorrhea episodes in children with TT. This procedure is more associated with specialists than with residents. On the other hand, 28.3% of doctors opt for multiple drug therapy.
Questions asked outside the scope of the guidelines revealed that 96.7% of doctors consider children’s age when deciding on surgery for TT placement. Despite the guidelines being directed at children aged from six months to 12 years, 54.3% of doctors do not operate on children between six and 18 months and 43.9% between 18 months and three years. Another factor limiting surgical intervention is the season: nearly half (49.1%) of doctors wait until the end of summer to decide on ventilation tube placement and 35.7% do not perform the procedure during summertime and 29.4% during spring. This behavior suggests an expectation regarding the environmental impact on the natural history of the disease, probably derived from the fact that there are fewer respiratory infection episodes, more outdoor activities, and higher temperatures in spring and summer. Despite this, expecting improvements in OME during summertime may be considered “not rational”, as suggested by a study developed during a year in Berlin, Germany, based on the execution of a tympanogram.13 The contrary was suggested in a study in New York, USA, based on tympanogram and pneumatic otoscopy for three years and in another study in children aged one year in the Netherlands.14,15 These differences can be justified by the methodology used or by the fact that summer features vary according to geographic position. Portuguese summer is typically long, hot, and dry. Moreover, 68% of doctors recommend bathing in the ocean. There was a statistically significant association between the decision on surgery and season, on the one side, and the advice of bathing in the sea, on the other (p<0.05). Although there is no robust data in the literature regarding the influence of multiple consecutive beach days and sea bathing, there is a belief that this is a beneficial practice. In Portugal, this recommendation is easier to achieve in consecutive days, because civil servants are compelled to take a period of vacation during summer (July, August, and September) and most companies either are closed or make their employees go on vacation in august. The mild weather and hundreds of kilometers of accessible beaches encourage most individuals to go to the beach on holidays.
Crenotherapy treatments in sulphurous waters have been around for hundreds of years in Portugal and their medicinal use is based on scientific foundations since the 18th century.16 Despite not being included in the guidelines, crenotherapy has been used in the treatment of OME in children for a long time and emerged as a promising treatment option in recent publications.17,18 Given this, it is not surprising that 21.9% of participants in this study recommended crenotherapy for children with OME. The opposite was observed regarding indoor swimming: 85.1% recommended against it, probably due to the increased risk of middle ear acute infections.
The use of drugs has been completely excluded from the latest OME treatment recommendations6,7. This is a complex topic, due to the non-consensual literature results for some drugs, as oral corticoids.19 In the present study, topical nasal corticoids (87.7%) and alpha-amylase (58.4%) were found to be largely used, similarly to antihistaminics (43.1%) and oral immunotherapy (24.2%). This reflects a difficulty by Portuguese otolaryngologists in adopting a “watchful waiting” approach, possibly for taking into account OME pathophysiologic mechanisms: considering the hypothesis that lymphoid tissue hypertrophy contributes to eustachian tube obstruction, application of nasal corticoids is associated with a volumetric decrease20 and prevention of regrowth after adenoidectomy.20,21 In this study, corticoid use was associated with gender (with females using them more) and age (with individuals younger than 40 using them more) (p<0.05). Prevention of infections in the middle ear and pharyngeal lymphoid tissue, potentially relevant in OME pathophysiology, can be achieved through oral immunotherapy.22,23 Use of this treatment was associated with having less than 40 years of age, working in coastal regions, working in the public health sector, and being a specialist (p<0.05). The potentially beneficial effect of alpha-amylase on eustachian tube dysfunction (due to its efficacy in degrading polymicrobial bacterial biofilms) may be relevant, but evidence supporting its use is still very limited.24 Lastly, allergic etiology should also be considered in OME, due to its role in inflammation and increased susceptibility to infectious organisms of the upper respiratory tract.25 Because antihistaminics are standard in allergy treatment, it is difficult to explain their absence in the treatment of these patients. That can be justified by the fact that the guidelines do not recommend these drugs for OME treatment, regardless of its multiple possible etiologies. The authors, therefore, ask the opposite question: knowing the possible OME etiology and pathophysiology and the child’s clinical history, and adjusting to environmental and socioeconomic conditions, is it right to do nothing in face of an OME diagnosis?
This study has limitations that should be acknowledged, as a response rate under 50%, non-uniform questionnaire presentation, and limited knowledge about recent OME recommendations, and calls for a prospective study on the topic.
When considering OME, two therapeutic measures are highly influenced by regional features: sea bathing and crenotherapy. Because the decision to operate is also influenced by the children’s clinical status after the summer, it would be interesting to conduct a study exploring how many children avoid surgical procedures after being reassessed after a summer during which they bathed in the ocean on consecutive days.
Conclusion
Results from this study show that Portuguese otolaryngologists generally act according to the latest international guidelines in the management of OME. The only exceptions were regarding the persistence in recommending preventive measures for entry of water into the ear canal in children with TT and the use of drugs as treatment. Regarding the first, the position currently adopted by doctors should change over time, as new data from both fluid dynamics and the clinics emerges supporting guideline recommendations. Regarding the latter, decisions should be individualized according to the clinical case, considering the child’s age and clinical evolution, and risk/benefit of the medication.