A female preterm neonate with 1425 g of birth weight and fetal growth restriction in the third trimester was delivered by C-section at 34 weeks of gestational age. No trauma was described during pregnancy or delivery. Apgar scores at 1 and 5 minutes were 8 and 9, respectively. The head circumference was 29.5 cm (10th-50th centile for age) and the physical examination was unremarkable. The girl was admitted to the Neonatal Intensive Care Unit for late prematurity and very low weight.
On day three of life, a hard left parietal depression with approximately 3x3 cm of size and 2 cm of depth was noted (Figure 1). There was no evidence of pain or neurological impairment nor of other physical abnormalities. Calcium-phosphate metabolism was evaluated, with normal phosphate, calcium, and vitamin D values. Skull radiograph revealed an abnormal concavity in the left parietal bone. Head computed tomography (CT) showed a focal sinking of the left parietal bone posteriorly to the coronal suture, with no lytic or blastic bone lesions or epicranial or intracranial soft tissue component. A fracture line was also noted posteriorly and superiorly to this sinking and extending to the sagittal suture, most likely corresponding to the coaptated linear fracture (Figures 2 and 3). A watchful approach was adopted and the patient was discharged on day 28, maintaining follow-up at the Neurosurgery and Neonatology outpatient departments. At two months of chronological age, the parietal fracture was barely perceptible, and neurological examination was normal.
What is your diagnosis?
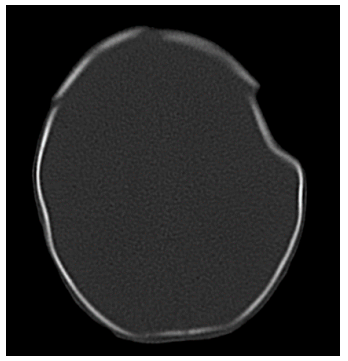
Figure 2 Head computed tomography showing focal sinking of the left parietal bone posteriorly to the coronal suture, corresponding to a probable "ping-pong" fracture
Diagnosis
Ping-pong fracture
Depressed skull fractures in newborns are rare, with an estimated incidence of 1-2.5 cases per 10,000 live births.1 These “green-stick” fractures are referred to as ‘ping-pong fractures’ because of the resemblance to an indented ping-pong ball.2 They develop in two distinct forms: iatrogenic (secondary to birth trauma) or spontaneous.1 Spontaneous intrauterine skull fractures are thought to be caused by compression against the maternal ischial bone, sacral promontory, symphysis pubis, uterine fibroid, fifth lumbar vertebrae, and fetal hands or part of a twin or asymmetrical pelvis.1
Regarding location, most fractures involve the parietal bone, with frontal and occipital bones less frequently implicated.3 This is due to immature ossification and prolonged focal pressure on a neonatal skull with membranous sutures, fontanelles, and low calcium levels, with consequent indentation of the bone surface and undisrupted bone continuity.1,2
Skull radiography can show the degree of deformity and cranial ultrasound can identify hemorrhages and/or hematomas, but computed tomography is the most accurate exam to describe the lesion and should be performed to confirm the diagnosis and exclude complications.4
The prognosis is good in spontaneous cases and those with a normal neurological examination.1,4,5 A watchful attitude is advised since many fractures can elevate spontaneously within four to six months.1,5
Available treatments include surgical elevation, elevation by digital pressure on the edges of the depression, and elevation by vacuum extractor or breast pump.5 Surgical treatment is reserved for selected cases with cerebrospinal fluid leak, wound infection, hematoma, bone fragments within the brain parenchyma, neurological deficits, signs of increased intracranial pressure, or cosmetically deforming defects.2,3,5
















