Introduction
Parotitis is defined as an inflammation of the parotid gland, characterized by swelling with or without pain, which can be accompanied by fever and malaise. It is usually associated with non-obstructive and non-suppurative sialectasis of the parotid gland. (1 The condition is defined as recurrent when two or more episodes occur without a defined time interval. Episodes are usually unilateral, but bilateral episodes can occasionally occur, with more prominent symptoms on one side. (2) Male are usually more affected than females, with a peak incidence between the ages of three and six years. Most patients experience complete and spontaneous resolution in the second decade of life. (1
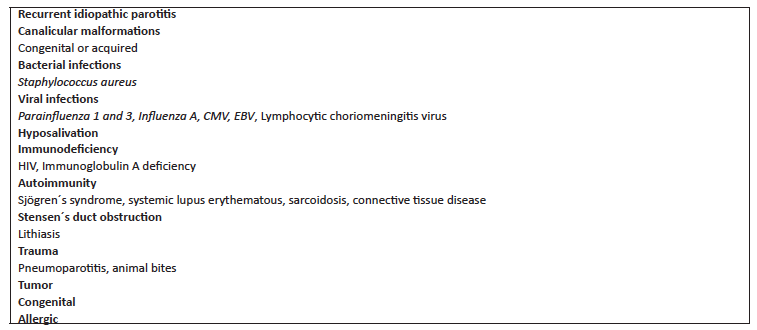
Although parotitis etiopathology remains unclear, a multifactorial origin, as suggested by Chirte and Premchandra is the present consensus. (1 The incidence of epidemic parotitis in Portugal has substantially decreased after the universal introduction of a vaccine. Consequently, recurrent idiopathic parotitis is currently considered the most common cause of parotid swelling. However, when approaching a patient with recurrent parotitis, various underlying causes have to be addressed (Table 1).
The diagnosis is based on clinical features, but imaging exams can be used to confirm it. Treatment aims at symptomatic relief (analgesics, sialogogues, massage, mouth rinses, oral hydration). In some cases, the use of antibiotics can be considered. A more aggressive approach to parotidectomy is reserved for serious situations that persist into adulthood. (3)-(4
The aim of this study was to investigate the clinical, laboratory, and imaging profile of children with recurrent parotitis.
Material and methods
A retrospective review of the medical records of patients referred to the Pediatric Outpatient Clinic of a level II hospital due to recurrent parotitis between January 2013 and June 2018 was conducted. Recurrent parotitis was defined by the presence of at least two parotitis episodes. Retrieved data included sex, age, date of first symptoms and referral, referral origin, and number of episodes. Clinical data regarding the presence of unilateral or bilateral swelling, presence of fever, and patients´ immunization status were also assessed. Data of imaging and analytical studies performed and final diagnosis of patients already discharged were also retrieved from medical records. Statistical analysis was performed using the Statistical Package for the Social Sciences (SPSS) software, version 22 (IBM Corporation, Armonk, NY, USA). Continuous variables were expressed as mean (minimum- maximum) or median (percentile 25-75).
Results
A total of 24 patients, predominantly male (66.7%), were referred to the Pediatric Outpatient Clinic in the considered time period, with a mean age of seven years and five months (minimum 18 months, maximum 14 years and five months). The Emergency Department was the most common referral origin (70.8%), followed by Primary Care (20.8%) and other hospital external consultations (8.3%). All patients had their immunization status updated according to their age. The median number of episodes per patient during follow-up was two (P25-75: two-four), and the median age of the first episode was five years and three months (P25-75: two years and ten months- seven years and six months). The mean number of episodes per year was two (minimum one, maximum five), and most episodes were unilateral (95.8%).
While all patients presented with parotid swelling and pain, only 58.3% of episodes were associated with fever- none presented with purulent discharge or macroscopically visible alterations in the Stensen´s duct ostium.
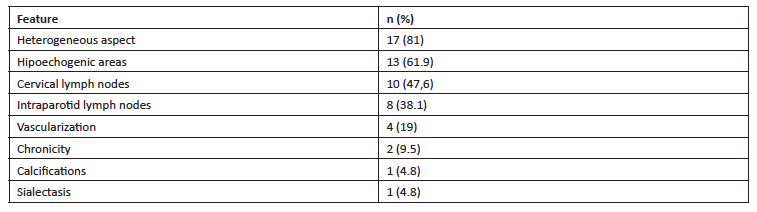
Acute- phase parotid and neck ultrasound was requested in 21 patients (87.5%) and mostly showed heterogeneous gland and hypoechoic areas in more than half of patients (Table 2).
Non-steroidal anti-inflammatory drugs (NSAIDs) were universally used to treat symptoms. Most cases had no associated complications. The only exception was the first episode of acute parotitis in a previously healthy 18-month-old male child, which was complicated with retropharyngeal edema, prompting hospitalization in the Pediatric Care Unit and treatment with intravenous antibiotics and corticoids.
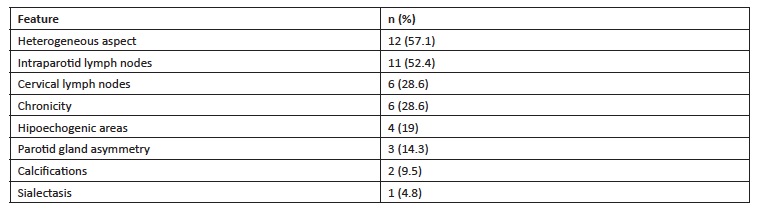
Non-acute phase parotid and neck ultrasound was requested in the non-acute phase in 87. 5% of patients, with a mean interval of five months after the acute episode. Contrarily to the acute-phase ultrasound, the most prominent features were the presence of a heterogeneous gland and of intraparotid lymph nodes (Table 3).
Parotid gland sialography was performed in five patients. The previous ultrasound had shown an enlarged parotid gland in two and calcifications in other two patients. Sialography was requested in the fifth patient due to young age of episode onset and high number of episodes. The exam showed alterations characteristic of chronic parotitis in two patients. In one case, an accessory diversification of the Stensen duct giving the appearance of a “tree in blossom” was described. Further investigation directed at Sjögren syndrome and sarcoidosis was suggested, and the patient was referred to a tertiary hospital. Although fulfilling three criteria for Sjögren syndrome diagnosis, he remains asymptomatic and currently maintains annual follow-up.
Magnetic resonance image (MRI) of the neck was performed in two patients after bilateral hypoechogenic areas potentially related to chronic parotitis or granulomatous disease were identified on ultrasound, showing characteristic features of chronic parotitis in one and no alterations in the other.
Among patients who underwent laboratory study, the one with suspected Sjögren syndrome showed immunoglobulin A deficit (Table 4) and tested positive for antinuclear antibodies (ANA). One patient had diminished levels of C3 complement, while another had diminished levels of C4 complement. The latter corresponded to the patient who had been admitted at 18 months due to an episode of acute parotitis with retropharyngeal edema. Because both showed only a discrete decrease in C3 and C4 complement levels, laboratory studies were not repeated during follow-up.
Cellular immunity study was performed in three patients, including in the patient with suspicion of Sjögren syndrome and in one patient with a high total number of episodes. One patient showed a mild decrease in T CD4+ cells, an increase in T CD45RO+ cells, and an increase in T CD4-/CD8- cells, possibly related to the recurrent parotitis episodes. No study indicated cellular immunodeficiency.
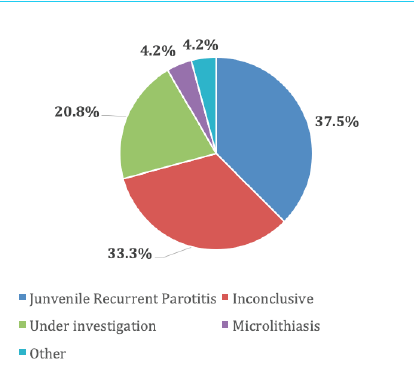
The most common final diagnosis in patients already discharged was juvenile recurrent parotitis (Figure 1). While a fifth of all patients was still under investigation, about a third maintained regular follow-up in the Pediatric Outpatient Clinic, despite inconclusive study up to that point. The median follow-up time was 22.5 months (P25-75: 5.5 - 31.25 months).
Table 4 Laboratory studies performed
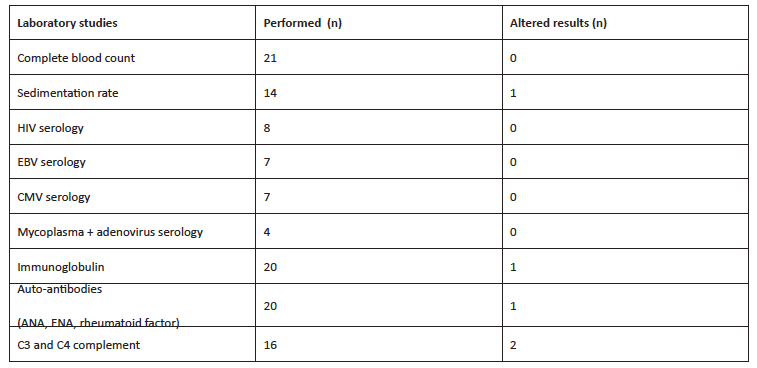
ANA, antinuclear antibodies; CMV, cytomegalovirus; EBV, Epstein-Barr virus; ENA, extractable nuclear antigen antibodies; HIV, human immunodeficiency virus
Discussion
Recurrent parotitis onset usually occurs between the ages of three and six years, although cases of earlier or later onset have been described. (6 Ericson et al. described a case series with an age of onset between three months and 16 years. (7) In this study, the mean age of onset of episodes was five years and three months, in accordance with the literature, as was the male predominance found. (7
The frequency of episodes is usually higher in the first school year, with a tendency to decrease until puberty and resolve after puberty. (1 According to Mandel and Kaynar, episodes usually occur one to five times a year, with Henriques et al. reporting a medium number of 5.8 episodes/year (mininum one, maximum 18/year). (8), (9 The present case series identified a lower incidence of annual episodes.
Symptoms are usually unilateral. When they are bilateral, there is usually a prominent side. (1 Findings of this study agree with this data, as most episodes identified were unilateral.
Painful swelling is frequently associated with fever, as observed in this sample. Most authors report the absence of purulent secretion through the parotid duct ostium, which was also observed in this study. An episode ranging from several days to two weeks was referred to by Henriques et al. (8 The present retrospective analysis did not allow to retrieve data regarding symptom duration.
Parotitis diagnosis is clinical. Ultrasound is the complementary exam of choice to confirm the diagnosis and for regular follow-up of children with recurrent parotitis, as proposed by Shimizu et al. (10
As reported by Rubaltelli et al., ultrasounds performed in the non-acute phase usually show an improvement of imaging features, which was observed in the present case series. (11
If calculi, duct dilatation, cysts, or gland enlargement are identified in ultrasound, sialography is recommended to rule out duct stenosis, obstruction, or other complications. (1 In addition, may play a relevant role in the treatment of patients with obstructive sialadenitis with recurrent infections. (12 However, it should be noted that glandular parenchyma and contralateral gland cannot be evaluated with sialography and that this method is contraindicated during acute episodes. Overall, the use of sialography is discouraged in children with self-limited conditions. (13
MRI provides a more detailed study of the parenchyma and canalicular system and helps differentiate between acute and chronic inflammatory processes. (4 It is a non-invasive method, but the elevated costs and need to sedate young children pose some limitations. (14 Magnetic resonance sialography is a new non-invasive technique with the purpose of evaluating the ductal system of salivary glands and producing sialographic images without using contrast media or radiation. It may be helpful in atypical cases and cases with bilateral presentation. (13
Laboratory study should be considered on a case-by-case basis. It is usually indicated in cases of late-onset recurrent parotitis, especially bilateral parotitis, suspicion of underlying chronic disease (Sjögren´s syndrome, systemic lupus erythematous, sarcoidosis) or immunodeficiencies (including acquired immunodeficiency, such as human immunodeficieny virus [HIV]), and in cases of frequent and severe episodes. (1), (9 Hence, the initial laboratory workup may include complete blood count, sedimentation rate, immunoglobulins, ANA, extractable nuclear antigen antibodies, and HIV serology. (3), (6), (9
Due to uncertainty regarding etiology, there are no universally accepted strategies or treatment guidelines for recurrent parotitis. Treatment of acute episodes aims at delivering symptomatic relief and preventing damage to the gland. (1 Analgesics and/or antipyretics, adequate oral hygiene, parotid gland massage, warmth, and use of chewing gum and sialogogue agents seem to be helpful in the acute phase. (15 Most authors agree on the use of antibiotics in cases of conservative treatment failure or severe symptoms. In a series of 50 patients, Landaeta et al. found out that the most common bacterial pathogens in salivary samples were Streptococcus pneumoniae, Haemophilus influenzae, and Streptococcus viridans. (16 Consequently, in the absence of evidence of staphylococci, penicillins, cephalosporins, or macrolide may be prescribed, with the first choice usually being aminopenicillin in combination with beta-lactamase inhibitors, as amoxicillin/clavulanic acid. (16
Surgical treatment includes parotidectomy, which is a relatively invasive procedure and carries the risk of facial nerve paralysis, and thus regarded as a last resort. Parotid duct ligation leading to gland atrophy represents another option and an alternative to parotidectomy in refractory cases. However, the success rate of this procedure is no greater than 50%.14
Recent studies suggest that sialendoscopy with steroids instillation may be successful in treating juvenile recurrent parotitis and autoimmune parotitis. According to Canzi et al., complete symptom resolution after sialendoscopic treatment was observed in 78% and partial regression in 22% of patients. This type of treatment is generally recommended in cases of frequent recurrence or pronounced symptoms. However, the true value of sialendoscopy in the diagnosis and therapeutic intervention in pediatric recurrent parotitis requires further studies. (17
In accordance with the literature, juvenile recurrent idiopathic parotitis was the most common diagnosis in this case series. Microlithiasis was the second most common finding. However, compared to the adult population, sialolithiasis or autoimmune disorders are less likely to be the pathologic condition for pediatric recurrent parotitis. (4), (5), (18
Recurrent parotitis prognosis depends on the underlying cause. Idiopathic parotitis has a favorable prognosis, with remission after puberty, although according to Cohen et al., 10-20% of cases may persist into adulthood. (19
Conclusions
Most recurrent parotitis etiologies in pediatric age are benign, and the most common diagnosis is juvenile recurrent idiopathic parotitis, which is usually a self-limited condition. In this report, the authors intend to remind that a more judicious request of complementary exams in the acute and non-acute phase can be time- and cost-effective. Laboratory and imaging studies should be requested in cases of suspicion of an underlying disease and not as routine studies. Implementation of a standardized approach could be the first step in that direction.