Introduction
Primary liver tumors are rare in the neonatal period, with vascular lesions as the most frequent. (1 Infantile hepatic hemangioendothelioma (IHH) is a benign vascular liver tumor commonly diagnosed within the first six months of life. (2), (3), (4 It is usually asymptomatic and may regress spontaneously within 12 to 18 months. (2), (5 Rarely, it can cause severe symptoms, such as liver dysfunction, congestive cardiac failure, and coagulopathy, requiring aggressive treatment. (2), (6 The diagnosis is established based on the child’s age, clinical features, serum α-fetoprotein level, and imaging findings. (4), (7
Herein the authors report the case of a preterm newborn with hepatic hemangioendothelioma incidentally diagnosed during echocardiographic evaluation in the context of sepsis.
Case report
Herein is reported the case of a male Caucasian newborn, born at 27 weeks of gestational age by spontaneous vaginal delivery after preterm premature rupture of membranes, weighing 1000 g. Physical examination was normal for age.
Eighteen days after admission, the boy developed a clinical-analytical condition compatible with sepsis, being prescribed cefotaxime and vancomycin.
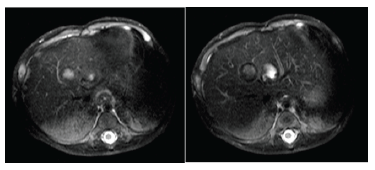
Two intrahepatic cystic lesions were incidentally identified at subcostal view during functional echocardiography. Abdominal ultrasound confirmed the presence of two adjacent cystic hepatic formations in segment VIII, with 13 and 17 mm, both without detectable vascularization (Figure 1). Considering the hypothesis of fungal liver abscesses, amphotericin B was added to antibiotic therapy and maintained for five weeks. In the absence of positive cultures and normal complete blood count, liver function tests, and serum alpha-fetoprotein (AFP) for age (16,692 ng/mL; normal range for age, 134,734 ± 41,444 ng/mL), the hypothesis of hepatic hemangioendothelioma was raised.
Abdominal magnetic resonance imaging (MRI) performed on the 66th day of life confirmed the presence of two hepatic hemangioendotheliomas in segments IV and VIII, with 14 and 12 mm, hypointense on T1- and hyperintense on T2-weighted images (Figure 2).
The boy was discharged home on the 75th postnatal day, clinically asymptomatic. Ultrasound control performed five weeks later showed stable liver lesions. At six-month follow-up, abdominal ultrasonography showed total regression of the previously described masses, and analytical control was normal.
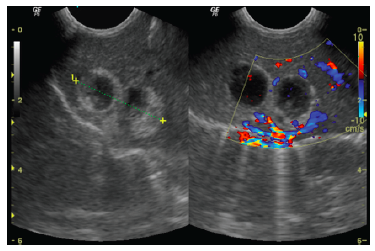
Figure 1 Abdominal ultrasound showing two adjacent cystic formations in segment VIII, with 13 and 17 mm, the largest with some peripheral hyperechogenic areas and the smallest more liquefied, and both without detectable vascularization.
Discussion
Functional echocardiography has become an invaluable tool in the Neonatal Intensive Care Unit and was crucial for the incidental diagnosis of the hepatic masses observed in the present case. (8
The differential diagnosis of hepatic masses in neonates can be categorized into congenital, neoplastic, or infectious. In this case, and given the clinical-analytical sepsis condition, the hypothesis of liver abscess was raised. The incidence of liver abscesses in preterm increased over the past two decades, probably due to their increased survival and use of invasive procedures (as umbilical catheterization and central catheters) and total parenteral nutrition. (9 In the present case, the absence of therapeutic response despite escalating therapy required an additional imaging modality to establish the diagnosis. As mass differentiation is complex, only MRI allowed a definitive IHH diagnosis in this case.
Benign liver tumors account for one-third of all hepatic lesions in children. IHH represents the most common benign vascular tumor of the liver, with female predominance and mostly apparent in the first six months of life. (3), (4), (10), (11 It is usually multifocal or diffuse, but single lesions may also be found. (3), (12
In most cases, IHH continues to grow during the first year of life, remaining asymptomatic and only incidentally detected in imaging assessment. During its natural course, spontaneous involution occurs within a few years. (2), (3 In the present patient, total regression occurred within the first year of life, without symptoms.
Despite its benign nature, multiple and diffuse lesions can present with life-threatening complications, including severe hypothyroidism, cardiac failure, fulminant hepatic failure, consumption coagulopathy, or intraabdominal hemorrhage, requiring aggressive treatment. (6), (11
Clinical manifestations ─ as abdominal distension, hepatomegaly, skin hemangioma, anemia, thrombocytopenia (Kasabach-Merritt syndrome), and rarely biliary and gastric outlet obstruction ─ can also occur. (3
The initial diagnostic approach consists of ultrasonography, but contrast-enhanced CT or MRI can provide a more definitive diagnosis. (3 MRI may identify IHH as hypointense on T1- and hyperintense on T2-weighted images and with centripetal or homogeneous enhancement. (13), (14
Some evidence suggests an increased risk of hepatoblastoma in preterm, with early exposure to oxidative stress potentially representing the main etiological factor. Consequently, a high index of suspicion for malignant liver lesions is essential. (15
Serum AFP has been used as an important tumor marker for hepatoblastoma, hepatocellular carcinoma, and germ cell tumors and should be tested in all cases. Although AFP levels may be elevated in IHH, they are never as high as seen in malignant lesions. (2), (4
Symptom severity and tumor size affect treatment decisions, which remain controversial. (6 While asymptomatic lesions may experience spontaneous regression and expectant management can be safely adopted, symptomatic lesions may require aggressive management to avoid severe complications. Several therapeutic options are available, including radiotherapy, hepatic artery ligation, and embolization, but systemic corticosteroids remain the mainstay of treatment. (2), (3
In the present case, nosocomial sepsis led to the diagnosis of hepatic masses, incidentally detected on functional echocardiography and initially interpreted as hepatic abscesses. However, lesion non-regression despite instituted therapy suggested other diagnostic hypotheses.
This case is an example of the diagnostic challenge that hemangioendothelioma represents in the neonatal period, particularly in extremely low birth weight preterm, and of successful conservative management with periodic radiological surveillance.