Introduction
Acute invasive fungal infection (AIFI) is a life-threatening condition with an annual incidence of 1.7/1 million inhabitants in the United States of America. (1), (2), (3), (4 The most common etiological agents are Aspergillus, Rhizopus, and Mucor species, which are often present in the natural environment and transmitted through inhalation or ingestion of spores, causing illness in immunosuppressed patients. (4 Their fungal hyphae are highly destructive for the mucosae, invade blood vessels and bones, and cause neutrophilic infiltration and tissue necrosis. (1)-(4
Mucormycosis is a rare AIFI infection caused by a group of fungi called Mucormycotina. Nineteen mucormycosis cases were identified in Portugal between 2001 and 2015, both in adults and children. Relevant risk factors associated with the disease include hematological disorders, HIV infection, transplant history, chemotherapy or corticosteroids exposure, prolonged antibiotic therapy, diabetic ketoacidosis, renal failure, and intravenous drug use. (3),(5), (6), (7)
The most common mucormycosis locations are rhino-orbital-cerebral sites (33-44%), skin (10-16%), and lung (10-11%). The most common agent is Rhizopus sp (37% of cases), followed by Mucor sp. and Rhizopus spp. Fungi are ubiquitous in the environment and a rare but substantial cause of infection in immunosuppressed persons and surgery patients. Frequent clinical signs of rhino-orbital-cerebral mucormycosis include fever, face swelling, diplopia, decreased vision, nasal discharge, facial pain, headache, decreased mental function, black nasal discharge crusts, turbine necrosis, ulceration, and palatal perforation. Cerebral infarction with neutrophilic infiltration and angioinvasion can also occur. (1)-(4
The diagnosis is established based on clinical symptoms combined with risk factors and imaging assessment, as well as tissue biopsy for culture (positive in 33-61%) and histopathology. (1)-(4), (8), (9
Regarding treatment options, lipossomal amphotericin B (L-Amb B) and posaconazol/isavuconazol are first- and second-line antifungal options that should be used in addition to aggressive surgical treatment. The choice of the agent for central nervous system (CNS) infection depends on CSF penetration and activity spectrum. L-Amb B has relatively limited distribution in CSF but achieves detectable therapeutic levels in CNS. Posaconazol achieves negligible concentrations in CSF, but isavuconazol has considerable efficacy in CNS infections. (3 Successful use of isavuconazol has been mostly reported in adults, but also in children. (3
Despite aggressive surgical debridement, immune restoration therapy, and long-term high-dose antifungal treatment, the risk of recurrence is high. (1)-(4), (8), (9 In the course of rhino-orbital-cerebral mucormycosis, morbidity varies between 30-97%, and mortality between 70-80%.3), (9), (10), (11), (12)
Case report
A 14-year-old male was diagnosed with acute T-lymphoblastic lymphoma (mediastinal mass, testicular and cutaneous disease at presentation; no CNS involvement). Chemotherapy was prescribed according to CLG-EORTC arm AR2 protocol (high average risk), with complete response after one month.
While in the seventh month of reinduction chemotherapy, the patient was admitted to the Emergency Department with discrete left facial paresthesia. No neurologic deficits were found, as well as no neutropenia in blood work. Cerebral computerized tomography (CT) scan disclosed no abnormalities, and the boy was discharged home with a reevaluation appointment scheduled for less than one week.
On the following day, the boy returned to the hospital with left peripheral facial paresis and neutropenia. Cerebral CT scan was repeated, showing rapidly progressive pansinusitis, and the patient was admitted for intravenous therapy with meropenem, vancomycin, and L-Amb B 3 mg/kg. On the next day, he developed diplopia, opthalmoplegia, and left ptosis, requiring neurological evaluation. CT scan showed a completely different image from the previous day, suggestive of mucormycosis with extension to the left orbit and nasal region. On day four, the patient developed fever, together with right deviation of the labial commissure and amaurosis. On day five, magnetic resonance imaging (MRI) of the brain confirmed pansinusitis with extension to pterygoids muscles and posterior part of the nasopharynx and orbit, facial cellulitis, thrombosis of the left cavernous sinus, venous congestion of the left orbit and proptosis, left carotid artery stenosis, and encephalitis of the left temporal lobe and orbital portion of the left frontal lobe. L-Amb B was increased to 5 mg/kg and prophylactic enoxaparin was started. On day six, microbiological analysis of a sample aspirate confirmed Rhizopus sp infection. Sequential blood cultures collected since admission were all negative, and CSF cytological and microbiological analysis was negative for other infections and malignant disease.
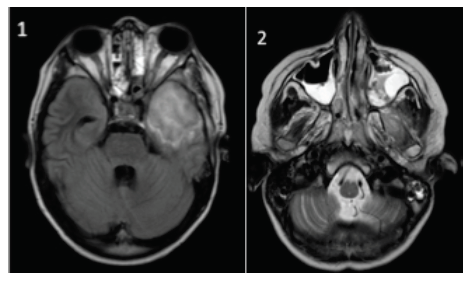
On day 12, control MRI (Figures 1 and 2) showed pansinusitis worsening and extension of the infection through muscular and adipose tissues, optic nerve, and optical chiasma; invasion of the II, III, IV, V, and VI nerves; and irregular fronto-temporo-insular cerebral abscess, with 51 x 42 x 46 mm, causing a mass effect. At this time, L-Amb B was increased to 10 mg/kg and posaconazol was added.
On day 13, successful multidisciplinary surgery involving Neurosurgery, Ophthalmology, and Otorhinolaryngology was conducted. The procedure included removal of the affected area of the brain and surroundings, lateral and upper orbitotomy, optical nerve section, enucleation of the left orbit, and endoscopic sinus surgery.
One week later, posaconazol was replaced by intravenous isavuconazol 200 mg twice daily, and fever decreased. Hyperbaric chamber treatment was also attempted to improve local tissue vascularization but was poorly tolerated, with nausea and vomiting, and suspended after four sessions. The patient developed severe hypokalemia, decreased renal clearance, nausea, vomiting (assumed as an adverse event of the antifungal agents), and stable thrombocytopenia (≈ 90.000x109/L platelets; no bleeding).
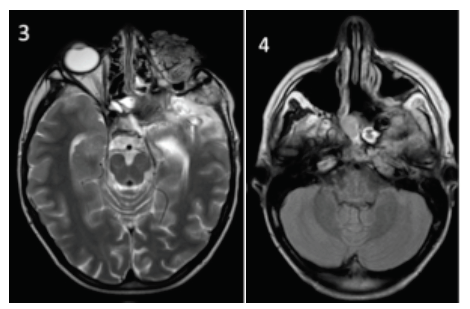
The need to remove the invaded orbital walls, together with orbital enucleation, left the patient with no anatomical support for the surrounding structures. Progressive left frontal herniation through the bony defect occurred, leading to a CSF fistula. Brain MRI performed two weeks later (Figures 3 and 4) confirmed cerebral herniation of the frontal lobe, with no ischemic tissue and slight improvement of fungal encephalitis. Persistence of osteomyelitis and infection of muscles and cerebral parenchyma were evident, besides multiple newly diagnosed mycotic aneurisms in the left internal carotid and middle cerebral arteries, and severe reduction of the left internal carotid artery flow.
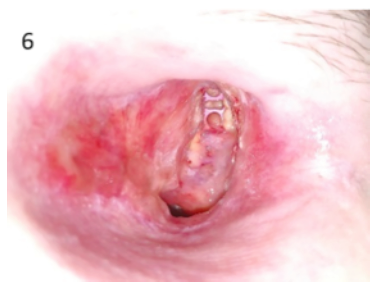
The day before scheduled angiography, the patient had a spontaneous severe mouth and nose bleeding that coursed with self-limited hypovolemic shock. He was transfused, intubated, and admitted to the Intensive Care Unit (ICU) for surveillance. Brain CT and angiography suggested post-hemorrhage spontaneous thrombosis of mycotic aneurysms, subsequently confirmed by MRI. This warranted neurosurgical reintervention through orbital reconstruction (with a titanium plate and patient’s abdominal fat) and correction of the CSF fistula and frontal lobe herniation, with extraction of devitalized tissues (Figures 5 and 6). After this surgery, the patient developed acute pancreatitis with small-volume bilateral pleural effusions, small-volume ascites, and decreased renal clearance with metabolic acidosis. He was discharged from the ICU one week later.
Overall, the boy remained in the hospital for four months since diagnosis, under L-Amb B and isavuconazol treatment, ionic supplementation, and physical rehabilitation. Subsequently, the same dosage of intravenous antifungal therapy was administered in outpatient setting. He is currently completely autonomous and cognitively able to have a normal social life, with initial concerns about cognitive frontal lobe impairment shown to be unfounded.
Chemotherapy was restarted four months after infection diagnosis, and the patient is currently in the maintenance phase (oral 6-mercaptopurine and methotrexate). L-Amb B was deescalated to 5 mg/kg six months after the infection (MRI showed a more limited infectious region), being stopped after 15 months. Intravenous isavuconazol was replaced by an oral formulation after 15 months, being still in use. The patient was reoperated two more times due to relapse of the frontal hernia and CSF fistula, with progressive fistula resolution.
Discussion
Case reports of mucormycosis infections in immunosuppressed patients are scarce, challenging the definition of the best approach. (13), (14), (15), (16), (17), (18), (19), (20), (21 This case highlights that immunosuppressive treatment is a relevant risk factor for fungal infection. With the availability of new and more potent drugs, the ideal prophylactic antifungal agent is yet to be defined.
Mucormycosis diagnosis demands a high index of suspicion and involvement of a multidisciplinary team to manage the accelerated destruction of infected structures, organ dysfunction, and mortality. Chemotherapy must be immediately stopped after diagnosis. Early and aggressive surgery seems to be the most relevant indicator of success, by controlling the infectious focus. Additionally, medical treatment must be optimized by selecting the most suitable agents against Mucorales − in the present case, L-Amb B in high dose (10 mg/kg/daily) and isavuconazol. The use of adjuvant therapies (such as hyperbaric chamber treatment) should be considered, if appropriate.
To the authors’ knowledge, this is the first report of (off-label) use of isavuconazol in the pediatric setting in Portugal. The drug is associated with less resistance compared to posaconazol and better CNS penetration. (22), (23), (24), (25 Side effects likely attributed to this agent have been reported, and include nausea, vomiting, hypokalemia, and renal impairment. In the present case, fever subsided as soon as the drug was started. A double antifungal strategy, previously described in similar case reports, was justified given the high disease severity in an immunosuppressed patient. (26)-(27 The combination of a new and highly effective option with limited use in pediatric patients (isavuconazol) and an old and well-known drug (L-Amb B) provided the rational for improved CNS penetration and patient outcomes, by using the most suitable antifungals available for this type of infection with no known interactions. The patient currently remains on oral isavuconazol and maintenance chemotherapy. L-Amb B proved to be a suitable first-line option for mucormycosis and an adequate agent to combine with isavuconazol. Although there are no guidelines stating for how long antifungal treatments should be maintained, waiting for chemotherapy completion and imaging resolution seems advisable.
After a long inpatient period, the boy’s functional status started improving with daily physical rehabilitation. He is currently accompanied by a multidisciplinary team including Pediatric Oncology, Neurosurgery, Otorhinolaryngology, and Ophthalmology. Chemotherapy was continued, with no other relevant adverse events. Psychological, psychiatric, social, and nutritional support were also provided. Close communication with the patient an family facilitated understanding and acceptance of medical team decisions, an important step to achieve success.