Introduction
Congenital dacryocystocele is a very rare condition, affecting 0.1−0.3% of newborns with nasolacrimal duct blockage. It is more prevalent in females and the mean age at presentation is seven days. (1)- (3
Although most cases spontaneously resolve in the first year of life, the condition can be associated with local complications, such as acute dacryocystitis, lacrimal abscess, fistula formation, or sepsis, making its early recognition crucial. (1
Case report
A female newborn with 24 hours of life and unremarkable family history was transferred to a tertiary pediatric hospital due to respiratory distress with onset in the first hours of life and worsening during breastfeeding. The girl remained calm and eupneic between meals and after aspiration of nasal secretions.
Pregnancy was uneventful, with no changes on ultrasound scans or evidence of congenital malformations.
On admission, the patient presented superior transmission noises at pulmonary auscultation, with peripheral oxygen saturation of 94% in room air. No other signs or symptoms were evident.
During flexible nasal endoscopy, some resistance was noticed in both nasal cavities after the nasal vestibule, but a patent nasal cavity without atresia was confirmed. Due to persistence of periodic respiratory distress episodes, computed tomography (CT) of the perinasal sinuses was performed, showing bilateral enlargement of lacrimal fossae creating a bulging in the inferior third of the lateral wall of both nasal cavities, suggesting dilation of the lacrimal sacs resulting in bilateral narrowing of nasal cavities (Figures 1 and 2). CT scan also confirmed the absence of bone or membranous atresia in choanae.
After evaluation by a multidisciplinary team including pediatricians, otolaryngologists, and ophthalmologists, the patient was kept under surveillance in the Intensive Care Unit (ICU).

Figure 1 Coronal image of computed tomography of the sinuses showing mucus accumulation in the nasolacrimal system and distention of the lacrimal sac to the Rosenmüller valve level
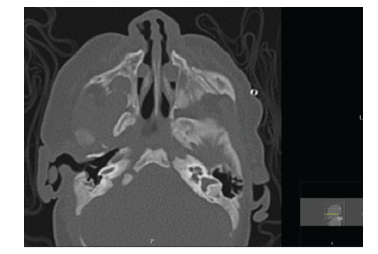
Figure 2 Axial image of computed tomography of the sinuses showing enlargement of the nasolacrimal channels, resulting in bilateral reduction of nasal cavity permeability
A conservative approach was decided, consisting of lacrimal sac massage (Crigler massage), regular nasal wash followed by aspiration, and regular peripheral oxygen saturation measurements.
After five days of uneventful admission, the patient was discharged.
She is currently periodically followed at Ophthalmology and Otolaryngology consultations, remaining asymptomatic and with no ophthalmic, respiratory, or eating distress.
Discussion
Since newborns are mandatory nasal breathers, any nasal cavity permeability reduction can lead to respiratory distress. (4), (5 In the present case, symptoms presented led to high clinical suspicion of obstructive pathology.
Dacryocystocele results from a persisting distal membrane of the nasolacrimal canal due to imperforation of the Hasner valve, leading to mucus retention in the nasolacrimal system and distention of the lacrimal sac to the level of Rosenmüller valve. (1), (2), (4), (5
The classic dacryocystocele presentation consists of a blue, cystic, firm mass below the medial canthus observed after birth. Other common symptoms include persistent tearing and ocular discharge. (2 None of these typical symptoms was observed in the present case.
Most cases are not associated with other syndromes or congenital anomalies. (1
Although the diagnosis is clinical, imaging tests can exclude other causes of nasal obstruction, such as choanal atresia or meningocele/meningoencephalocele 2), (4), (6) CT and MRI have similar sensitivity for identifying dacryocystocele. (4)-(6), (8) Nasal endoscopy also plays a relevant role, showing a bilateral polypoid lesion occupying the inferior nasal meatus in most cases. (4), (8
In the present case, a conservative approach was chosen after evaluation by a multidisciplinary team including pediatricians, ophthalmologists, and otorhinolaryngologists. Given the respiratory distress presented on admission, the newborn was admitted to the ICU for close surveillance.
Most dacryocystocele cases resolve spontaneously or with conservative treatment within the first year. (1), (2) When infected, treatment with systemic antibiotic may be necessary. (1), (5),(7)-(8
Periodic surveillance and expectant attitude represent the best management option in cases with no evidence of complications.
Few patients may require endoscopy-assisted probing of the lacrimal pathway. However, surgical intervention, either as first-line or end-of-line approach, is still a matter of debate in congenital dacryocystocele, with no conclusive evidence supporting its value. (1), (2















