Introduction
The number of children in the world currently exceeds 2.2 billion, accounting for approximately 28% of the world's population. Children aged between 10 and 19 years correspond to 16% of the world's population (UNICEF, 2019).
Besides the organic morbidity and mortality caused by the coronavirus disease 2019 (COVID-19), the pandemic also had an impact on the mental health of the general population. Although children and adolescents are at a lower risk of COVID-19 complications compared to adults, they suffer the indirect impact of the pandemic and associated restrictions.1
The COVID-19 pandemic led to strict infection prevention strategies, including mandatory mask-wearing, frequent hand sanitation, and social distancing. Moreover, several governments imposed nationwide quarantines, with closure of educational facilities and airports and cancellation of social events.2,3 Social distancing and quarantine had major negative psychological implications.3) These inexorable circumstances, which are beyond an ordinary experience, led to generalized stress, anxiety, and feelings of helplessness.2
Several studies have shown that young children seem to have increased levels of disturbed sleep, nightmares, poor appetite, inattentiveness, and significant separation problems due to the pandemic.2) Adolescents experience loneliness, anxiety, uncertainty, and compulsive use of internet gaming and social media, which puts them at higher risk of psychosocial morbidity.2
A systematic review of 63 studies including 51,576 children and adolescents with a mean age of 15.3 years found a clear association between loneliness and mental health problems in this population, and that loneliness was associated with depression and possible anxiety up to nine years after the event.4) Furthermore, the evidence suggests that the pandemic may have increased long-term adverse consequences on children and adolescents compared to adults.2
Anorexia nervosa (AN) is one of the most common mental disorders in adolescents. It is characterized by body image distortion and fear of fatness, driving significant caloric restriction, overexercise, and sometimes medically dangerous compensatory behaviors, such as postprandial vomiting and laxative or diuretic use.5,6 AN is often associated with other mental health comorbidities, such as depression, mood or anxiety disorders, and obsessive-compulsive disorders. It has the highest mortality risk of all mental health disorders, with deaths related to suicide and medical complications.3,5,6 For these reasons, it is predictable that the negative implications of COVID-19 restrictions will be more noticeable in individuals with AN, who more often experience emotional and physical isolation.7
The outpatient setting is considered to be the most appropriate for treating youth with AN, through specialized professionals who emphasize the role of the family.8
Three pathways by which the COVID-19 pandemic may exacerbate the risk of eating disorders (EDs) have been identified in a study about the impact of this pandemic.9 The first concerns disruptions to daily routines and constraints to outdoor activities that may increase weight and shape preocupations and negatively impact eating, exercise, and sleeping patterns. The second refers to a greater exposure to anxiety-provoking media, which may amplify the risk and symptoms of EDs. Lastly, fear of COVID-19 infection may increase health concerns, leading to the pursuit of restrictive diets focused on increasing immunity. In addition, elevated rates of stress and negative effects of social isolation due to pandemic may also contribute to an increased risk of EDs.9 Similar conclusions were drawn by Miniati and colleagues in a systematic review showing that restrictions in health care facilities were a contributor factor to increased anxiety and conflicts, and difficulties in relationships with "no way out" were the maintenance factors for ED symptoms, particularly in adolescents.10
Despite the substantial reduction in the number of children and adolescents taken to hospitals for medical assessment during the pandemic, numerous studies have reported increased pediatric mental health visits.11 Moreover, changes in healthcare delivery have been reported worldwide.
This study sought to assess the impact of the COVID-19 pandemic on the incidence, demographics, and clinical severity of AN and identify potential delays in the referral of these patients. It also aimed to compare the rate of pediatric consultations due to AN between the COVID-19 period and previous years and assess clinical parameters on the first consultation and comorbidities during pediatric appointments.
Material and methods
This was a retrospective cross-sectional study of adolescents with AN followed by the Multidisciplinary Group of Eating Disorders of a Portuguese tertiary hospital between January 1, 2017 and May 31, 2022. Adolescents were divided into two groups according to the beginning of their follow-up: pre- versus post-pandemic. The cut-off date was March 2, 2020.
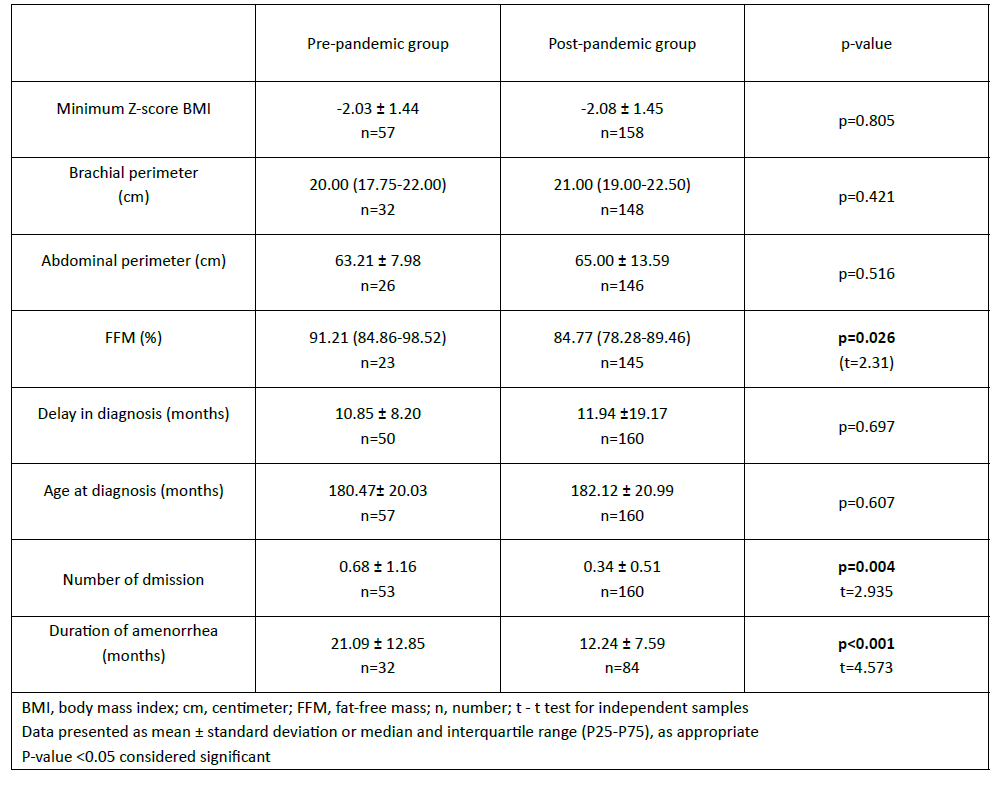
Demographic features, minimum body mass index (BMI) z-score, arm and abdominal circumference on admission, time of symptom onset, percentage of fat-free mass (FFM) by bioimpedance analysis, time to referral, presence of pericardial effusion, and number of hospital admissions were assessed and compared between groups.
All statistical analyses were performed using SPSS Statistics version 25. Descriptive analyses were performed for all variables in the pre- and post-pandemic groups. Categorical variables were presented as absolute frequency and percentage and analyzed using the Chi-square test. Continuous variables were analyzed using the t-test for independent samples. P values less than 0.05 were considered significant.
Results
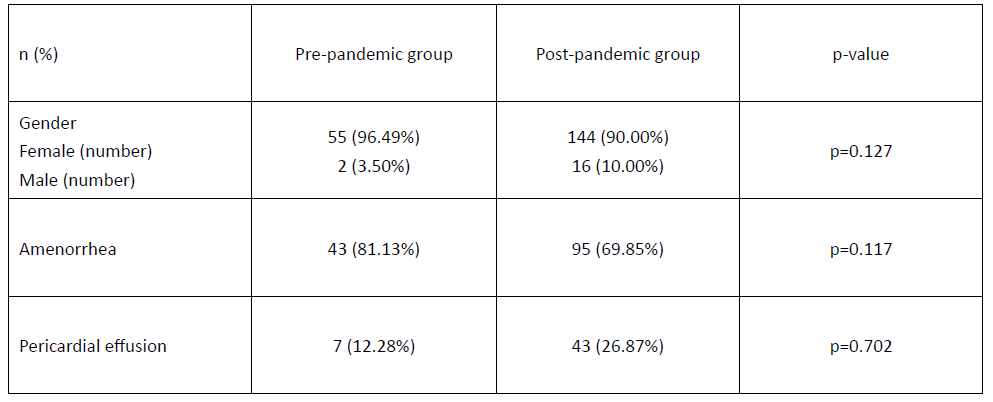
A total of 217 patients with AN were identified during the study period, 57 of whom were diagnosed over a 3-year period in the pre-pandemic phase, and 160 over a slightly longer than 2-year period in the post-pandemic phase (Table 1).
The average number of cases diagnosed per month increased significantly from the pre- to the post-pandemic period (1.55 vs. 5.89; p=0,005), as it is show in Figure 1, with a non-significant increase in the number of male cases (p=0.127; Table 1).
No statistically significant differences were found between groups regarding age at diagnosis, minimum BMI z-score, and arm or abdominal circumference. FFM percentage was significantly higher in the pre-pandemic group (91.21% vs. 84.77%; p=0.026). The time elapsed between the date of symptom onset and referral to AN consultation was one month longer in the post-pandemic group, but this difference was not statistically significant (Table 2). The number of admissions to the pediatric ward was significantly higher in the pre- compared to post-pandemic group (Table 2).
The percentage of girls with amenorrhea was 81.13% in the pre-pandemic group compared to 69.85% in the post-pandemic group, but this difference was not statistically significant. As expected, the duration of amenorrhea was longer in the pre- compared to the post-pandemic group during follow-up, justifying these results.
Although the number of male patients with AN was higher in the post-pandemic period, the difference to the pre-pandemic period was not significant (Table 3). A higher but also non-significant proportion of patients with pericardial effusion was identified after the pandemic (Table 3).
Table 1 Patients referred to the Multidisciplinary Group of Eating Disorders between January 1, 2017 and May 31, 2022 and mean number of patients admitted before and after March 2, 2020 cut-off
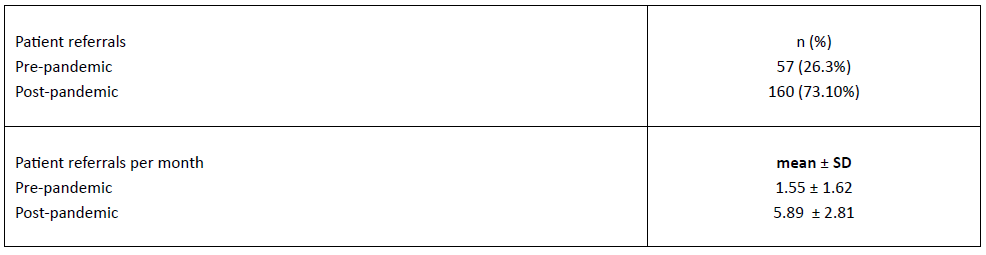
n, number; SD, standard deviation
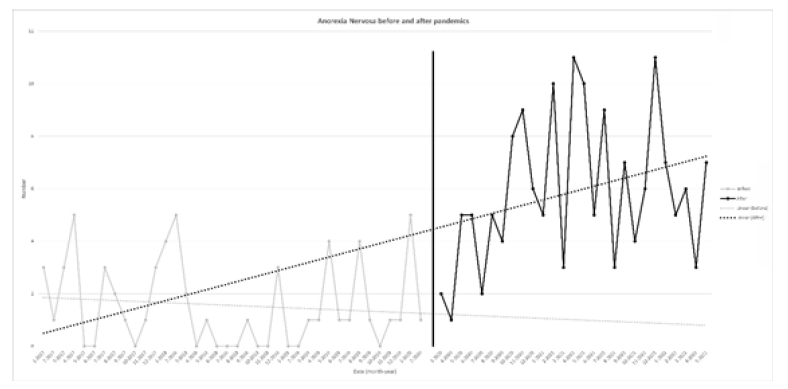
Figure 1 Evolution in the number of first referrals to the Multidisciplinary Group of Eating Disorders before and after the pandemic
Discussion
This study investigated children and adolescents referred to the Multidisciplinary Group of Eating Disorders of a tertiary hospital in Portugal. Most patients were referred from General Medicine, other medical specialties, or emergency services.
During the pandemic period, the incidence of AN referrals increased by more than threefold, in agreement with other studies also reporting an increase in the incidence of this condition.12,13 In addition, an increase in the number of male cases was also identified.
The number of hospitalizations was significantly higher in the pre-COVID compared to the post-COVID group, probably as a result of longer follow-up.
The percentage of FFM was also significantly higher in the pre-pandemic group (91.21% versus 84.77% in the post-pandemic group). Although BMI values were similar in both periods, the post-pandemic group seemed to have a higher percentage of fat at the time of minimum BMI assessment.
Despite the growing incidence of AN, this was not accompanied by an increase in clinical severity. Similar results were found by Springall G et al.,13 but not by Spettigue W and colleagues,14 according to whom hospital AN presented with higher rates of medical instability and need for hospitalization during the pandemic.14 Agostino et al. also reported that the worst markers of disease activity were found in patients diagnosed during the first wave of the pandemic.15
A multicenter European study revealed a higher overall admission rate during the pandemic in four of six representatives of European hospitals. (16 Clinicians in the study perceived a higher symptom severity in 2020 compared to 2019, mainly due to more social media usage, longer exercise duration, and more restrictive eating patterns.16 Although the number of inpatients during these periods was not assessed in the current study, unpublished data shows a trend towards a stable number of inpatients, as the maximum number of admissions had already been reached in 2019. These results are similar to those reported at a German center, where the number of admissions also did not increase and thereby the multidisciplinary team could get closer to patients to accompany them as outpatients.16
Another study measured the early impact of COVID-19 on the concerns of individuals with AN and reported an increase in restrictions and fears about being able to find foods consistent with their meal plans.17 The respondents described a marked increase in anxiety since 2019 and more significant concerns about the impact of COVID-19 on their mental than physical health.17 This issue should also be addressed and investigated in the population included in the present study to improve the understanding of the impact of the pandemic in these patients.
Conclusion
Despite the increase in the number of AN cases due to the pandemic, no significant changes were apparently noted in their severity at presentation. This suggests that, rather than exacerbating symptoms in patients with preexisting EDs, the COVID-19 pandemic may trigger the onset of disordered behaviors. It can also be speculated that ED behaviors were identified sooner due to the proximity of family members during lockdown, even though the time between symptom onset and the first consultation was almost the same.
Despite changes in the dynamics of health services due to the pandemic, this caused no delays in the referral and follow-up of patients with AN to the appropriate services.
The medical complications seen in youth with AN are extensive. While most complications are fully reversible with weight restoration, potentially irreversible damage to growth, bone, and reproductive health may occur.