Introduction
Kawasaki disease (KD) is one of the most common vasculitides in childhood, predominantly affecting children younger than five years old. It is a medium-sized arteries vasculitis with a predilection for coronaries.1 Despite being an acute and mostly self-limited illness, KD may cause serious complications, such as coronary artery aneurism (CAA). This is the most common cause of acquired heart disease in children in developed countries. In fact, the long-term prognosis is determined by coronary artery involvement, and prompt diagnosis and treatment are critical to reducing cardiovascular sequelae.2-4
The diagnosis of KD is clinical, as there are no specific diagnostic tests for the condition. According to the recently reviewed American Heart Association guidelines, the diagnosis of KD is based on the presence of at least five days of fever and at least four of the following criteria: (a) oral changes (erythema and cracking of lips, strawberry tongue, oral and pharyngeal mucosa erythema); (b) conjunctivitis (bilateral bulbar injection without exudate); (c) rash (maculopapular, diffuse erythroderma, or multiforme-like erythema); (d) extremity changes (erythema and edema of the hands and feet in the acute phase and/or periungual desquamation in subacute phase); or (e) cervical lymphadenopathy (≥ 1.5 cm in diameter, typically unilateral).4 Patients who do not meet the case definition of KD may be diagnosed with incomplete or atypical KD, which has a higher risk of coronary artery abnormalities.5,6
As the clinical features of KD manifest gradually and symptoms such as cervical lymphadenopathy and oropharyngeal mucosal involvement are frequent, the clinical presentation may be initially interpreted as a deep neck infection with unnecessary antibiotic therapy or surgical intervention, delaying diagnosis and treatment.7,8 Incomplete KD diagnosis may be even more challenging in this setting.
The authors report a case of incomplete KD presenting as complicated acute tonsillitis.
Case report
A four-year-old girl with a history of recurrent tonsillitis and acute otitis media presented to the Emergency Department with a history of fever, left cervical swelling, and torticollis with four days of evolution, receiving oral amoxicillin for two days for acute tonsillitis. No other significant medical or surgical history or previously known drug allergies were identified, and immunizations were up to date.
Physical examination revealed painful left cervical lymphadenopathies with restricted neck movements, and oropharynx examination showed an erythematous mucosa without exudates or swelling. Vital signs were within the normal range, and there was no evidence of other oral mucosa features, skin rash, or extremities or conjunctiva alterations.
Laboratory test results were notable for leukocytosis (23.370/uL, with 77.8% neutrophilia) and elevated C-reactive protein (CRP; 244.5mg/L). The remaining laboratory tests were normal, including platelet count (297.000/uL), alanine aminotransferase (18 U/L), and sodium (134 mmol/L) levels, and urinalysis showed no pyuria.
Cervical ultrasound showed an aggregate of multiple pericentimetric lymph nodes, with adjacent fat densification and no signs of necrosis. Cervical computed tomography (CT) revealed an enlarged left palatine tonsil without contrast enhancement, compatible with tonsillitis, with multiple reactive lymphadenopathies in the left internal jugular chain and left retropharyngeal space, one of which with initial signs of liquefaction (Figure 1-A). Liquid infiltration with a maximum thickness of 8 mm in axial plane was noted in the retropharyngeal space, suggesting an early retropharyngeal abscess (Figure 1-B).
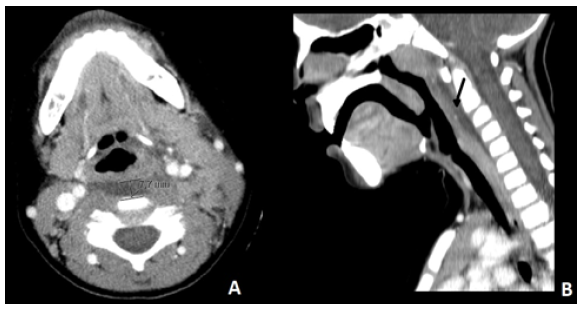
Figure 1 Cervical CT scan showing liquid infiltration in the retropharyngeal space suggestive of an initial retropharyngeal abscess. (A) Axial plan, with a maximum thickness of 8 mm. (B) Sagittal plan (arrow).
The child was evaluated by Otorhinolaryngology, with no surgical indication, and admitted with intravenous (IV) ceftriaxone and clindamycin.
Within 24 hours, clinical deterioration occurred, with increased cervical swelling and worsened torticollis. On oropharynx examination, posterior left pharyngeal wall swelling was observed. Left peritonsillar and parapharyngeal puncture was performed, without exudate drainage.
On day three of admission, cervical CT was repeated due to sustained fever and worsened CRP, with similar findings. Blood culture was negative, and Epstein-Barr, cytomegalovirus, and toxoplasmosis testing were also negative for acute infection. Surgical reintervention was decided, with peritonsillar and parapharyngeal drainage again negative for the presence of an abscess.
On day six (day ten of fever), non-specific generalized rash and mild hand edema were noted. At this stage, the child presented normal heart rate and blood pressure (50-90th percentile of systolic and diastolic blood pressure) and unremarkable cardiac auscultation.9 Incomplete KD was suspected, and the child was evaluated by pediatric Cardiology. The electrocardiogram showed sinus rhythm, normal heart rate, PR and QT intervals for age, and no ST or T-wave alterations. The echocardiogram showed normal structured heart, left ventricular size, and biventricular function without segmental disturbances, left ventricular ejection fraction of 70%, and shortening fraction of 43%. It revealed a small CAA of the left circumflex artery (z-score: 3.2) and of the CAA of the left anterior descending artery (z-score: 4.9), with no other changes. Z-score classification was as proposed by the American Heart Association.4
The girl was treated with IV immunoglobulin (IVIG) 2 g/kg, IV methylprednisolone 2 mg/kg/day, and low anti-inflammatory dose of acetylsalicylic acid (ASA), with apyrexia in less than 24 hours and significant clinical and laboratory improvement.
One week later, a coronary artery z-score reduction was noticeable, from 3.2 and 4.9 to 2.04 and 2.2 in the left anterior descending and left circumflex arteries, respectively. Corticotherapy was altered to oral prednisolone, and ASA was adjusted to an anti-aggregating dose.
The child was discharged home on day 15 of admission and completed three weeks of corticosteroids.
Six weeks after discharge, she presented mild hand desquamation and normal laboratory and echocardiogram (coronary arteries z-score: less than 2) findings. On one-year follow-up, she remained asymptomatic and with normal echocardiogram.
Discussion
Despite the increased knowledge about KD, its diagnosis remains challenging, with delayed diagnosis and treatment ultimately resulting in life-threatening complications, such as CAA.
When the initial clinical presentation is incomplete and only otorhinolaryngological manifestations are present together with fever, the child may be misdiagnosed with bacterial neck infection. In addition, persistent fever may be interpreted as treatment ineffectiveness and result in therapeutic escalation. On the other hand, new rash may be interpreted as an allergic reaction to antibiotics. All these factors can result in delayed KD diagnosis.8
In the present case, the child was already receiving oral treatment for acute tonsillitis and initially presented with persistent fever and lymphadenopathy, with no other cardinal signs of KD until day ten of fever. Although lymphadenopathy is the least common of KD clinical features, it may be the most notable and only clinical finding initially.4 In addition, besides significant torticollis and restricted neck movements, the child in the present case had a CT compatible with a retropharyngeal abscess. Retropharyngeal edema has been described in some KD patients, and once the diagnosis is established, the abscess-like lesion on CT scan should be interpreted as a type of inflammation rather than infection, explaining negative and sterile punctures.8,10 Particular CT findings, such as the absence of ring enhancement and mass effect on the airway, may help to differentiate retropharyngeal edema of KD from retropharyngeal abscess, sparing unnecessary surgical intervention.11-13
In cases of suspected complicated acute tonsillitis or other deep neck infections not responsive to adequate treatment, a high index of suspicion of KD should be maintained, at least prior to surgical intervention. In fact, KD should be considered in the differential diagnosis of persistent unexplained fever if associated with any of the main clinical criteria. The presence of two or three clinical criteria with supplemental laboratory criteria or a positive echocardiogram allow to establish the diagnosis of incomplete KD. The revised American Heart Association guidelines include an algorithm for this assessment, in order to ensure the diagnosis during the effective therapeutic window. 4 Supplemental laboratory criteria are summarized in Table 1.
Table 1 Supplemental laboratory criteria for the diagnosis of incomplete Kawasaki disease
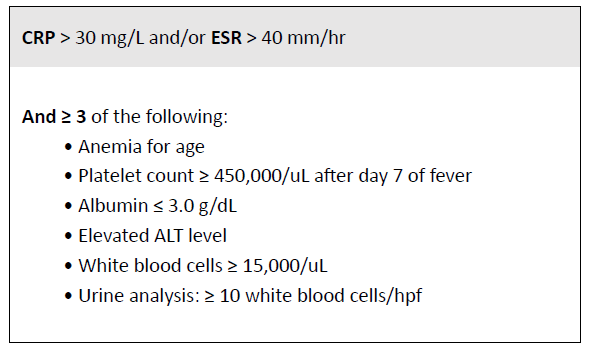
CRP: C-reactive protein; ESR: erythrocyte sedimentation rate
Regarding KD treatment, timely initiation of IVIG therapy reduces the incidence of CAA defined from absolute luminal dimensions from 25% to ≈4%, showing the importance of prompt treatment. In the particular case of early coronary involvement, the child should be aggressively treated with IVIG and corticosteroids.4 The evidence shows that, even with different corticosteroid regimens and prediction scores, first-line treatment of high-risk children with corticosteroids (in addition to IVIG and ASA) reduces the prevalence of coronary artery involvement and inflammation and fever duration. However, the identification of this high-risk group in the non-Japanese population remains controversial.4,14,15 In the absence of controlled data, the optimal initial dose of ASA remains debatable. Recent evidence strongly suggests that higher doses (>30 mg/kg/day) have no clear advantage in suppressing inflammation. Some authors further argue that, besides increasing the risk of adverse effects, they may also be associated with poor coronary outcomes, suggesting the use of antiplatelet doses of ASA (3-5 mg/kg/day) in the acute phase. This debate will predictably continue until more evidence becomes available.4,16 In the present case, in addition to the clinical and laboratory improvement, small CAA rapidly and persistently resolved with aggressive treatment.
After acute illness, long-term management should be individualized depending on the presence and severity of coronary alterations. Standard cardiological assessment should include physical examination, electrocardiogram, and echocardiography. Patients without consistent coronary involvement at one and four to six weeks after acute treatment can be discharged early from Cardiology, as they are not at risk for the development of new abnormalities. Conversely, patients with CAA of any size identified during any assessment should undergo regular Cardiology follow-up with a frequency depending on the degree of maximal and current CAA dimension and other risk factors for cardiovascular disease.4
This case occurred in September 2019, before the first reports of SARS-CoV-2 infection in China in December that year. Most children with COVID-19 are asymptomatic or present mild symptoms. However, a small subgroup develops a significant systemic inflammatory response known as pediatric inflammatory multisystem syndrome temporally associated with SARS-CoV-2 (PIMS-TS). PIMS-TS is associated with persistent fever and organ dysfunction, including CAA, and shares clinical features with other conditions, including KD, representing a new and challenging condition to consider in the differential diagnosis.17-19















