Introduction
Allergic diseases are common in pediatric age and one of the main morbidity causes.1) The last decades have witnessed a significant increase in the prevalence of these diseases2,3, namely asthma, allergic rhinitis (AR), and atopic eczema (AE), but also food allergies (FA) and drug allergies (DA).4 Estimates indicate that 4.3% of the EUA population has asthma, with a higher annual prevalence in children (9.5%) compared to adults (7.7%) according to U.S data from 2008-2010.5 AR is one of the conditions with higher prevalence worldwide,6 affecting about 40% of the pediatric population.3 AE has an estimated prevalence of 15−30% in pediatric age and a growing incidence primarily in industrialized countries.3 Hypersensitivity drug reactions have been associated with longer hospitalizations and are often under or overdiagnosed, leading to limitations in patients’ therapeutic options.7 Similarly to other allergic conditions, FA represents an important public health concern4 and is associated with a negative impact on patients’ quality of life.8,9
Developments in scientific research have improved the understanding of the pathophysiology, risk factors, and treatment of allergic diseases.10 Concurrently, advances in new technologies have also improved the diagnosis of these conditions and diversified the therapeutic options available in Allergy and Clinical Immunology (ACI).10 The allergist has thus become the most competent specialist in the individual management of allergic diseases.11
Understanding the patterns of referral of patients to the outpatient consultation (OC) of ACI is of great relevance, as ACI not only provides outpatient care, but is also responsible for diagnosing, treating, and managing allergic conditions. This study aimed to describe the origin and reasons for referral of patients to ACI OC, with the aim of improving the medical care provided.
Materials and method
This was a retrospective study comprising all pediatric age groups (0-18 years old) attending an ACI first consultation at a tertiary hospital between January and December 2020. Demographic data (gender and age), origin of referral, and reason for referral were collected from patients’ medical records. Statistical analysis was conducted using SPSS version 22.0.
Results
A total of 751 children were included in this study, 52.5% (n=394) of whom male, with a median age of nine years (P25 5 years−P75 13 years). The 0−5-year age group was the most frequently referred to consultation (Figure 1). Patients were referred to ACI OC by general practitioners (GP), pediatricians, and otorhinolaryngologists (ENT), among other specialists.
GP referred 41% (n=310) of patients, mainly for suspicion of rhinitis and/or asthma (n=164; 53%), followed by cutaneous pathology (n=59; 19%), DA (n=47; 15%), and FA (n=37; 12%). Allergy to Hymenoptera venom motivated three referrals (Table 1). Pediatricians referred 36% (n=274) of patients, of whom 69% (n=189) came from the GP’s outpatient consultation and Pediatric sub-specialities, 29% (n=80) from the Emergency Department (ED), and 2% (n=5) from hospitalization. Patients coming from GP’s outpatient consultation and from Pediatric subspecialities were referred due to rhinitis and/or asthma (n=98; 52%), FA (n=39; 20%), DA (n=26; 14%), or cutaneous diseases (n=26; 14%). Patients coming from the ED were mainly referred for DA (n=54; 67%), followed by FA (n=11; 14%), asthma and/or rhinitis (n=8; 10%), and cutaneous diseases (n=7; 9%). Regarding hospitalized patients, 80% (n=4) were seen due to DA and 20% (n=1) due to FA (Table 1). ENT specialists referred 20% (n=150) of patients, with respiratory diseases being the sole reason for referral (85% AR, 13% AR and asthma, and 2% only asthma; Table 2). In addition, a minor proportion of patients were also referred by Dermatology (1.5%), Stomatology (0,5%), and Medical Genetics (0.3%).
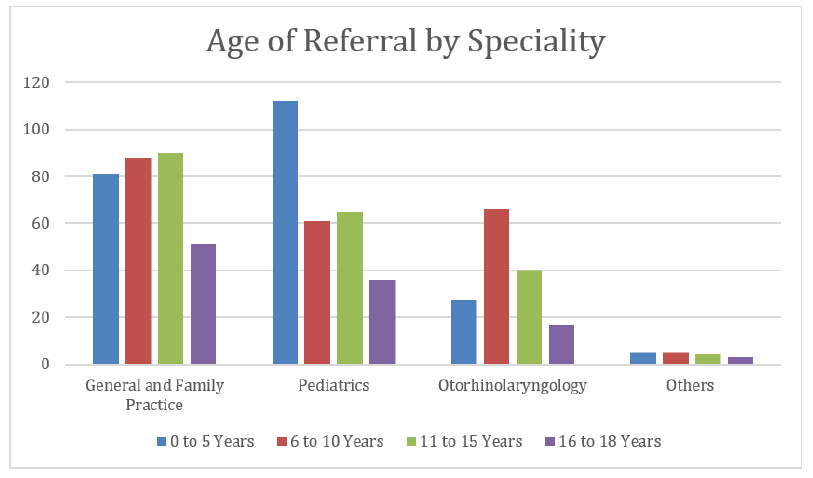
Figure 1 Number of patients referred to the Allergy and Clinical Immunology outpatient consultation, by speciality and age group.
Table 1 Reasons for patient referral to the ACI consultation by GP and pediatricians
| Rhinitis/asthma | Cutaneous diseases | Drug allergy | Food allergy | Hymenoptera venom allergy | ||
| GP 41% (n=310) | 53% (n=164) | 19% (n=59) | 15% (n=47) | 12% (n=37) | 1% (n=3) | |
| Pediatrics 36% (n=274) | Outpatient Department 69% (n=189) | 52% (n=98) | 14% (n=26) | 14% (n=26) | 20% (n=39) | -- |
| Emergency Department 29% (n=80) | 10% (n=8) | 9% (n=7) | 67% (n=54) | 14% (n=11) | -- | |
| Hospitalization 2% (n=5) | -- | -- | 80% (n=4) | 20% (n=1) | -- | |
ACI, Allergy and Clinical Immunology; GP, General and Family Practice
Discussion and conclusions
This study allowed to retrieve a global perception of the intercommunication between different medical specialities and ACI. The referral pattern to ACI OC denoted the general knowledge of other specialities regarding ACI and emphasized the need for a multidisciplinary approach to the diagnosis and management of ACI patients.
GP were responsible for the largest number of referrals to hospital services, highlighting the awareness of these physicians and the good cooperation between primary and secondary care. This cooperation has been continuously reinforced in conferences, courses, and training programmes directed at primary care. On the other hand, patients with allergic diseases are complex, and the care initiated by GP may require follow-up and optimization by the allergist/immunologist. The support provided by ACI is crucial both to patients and GP, as evidenced by the demand, not only during the 1994-1997 period, but also nowadays.12
After GP, pediatricians were responsible for referring the second largest number of patients to the ACI OC. Regarding age groups, pediatricians referred the largest number of patients under the age of five (Figure 1). Both Pediatric and ACI departments are located in a tertiary hospital centre, often sharing the same physical space in Day Hospital and OC. Moreover, ACI and Pediatric specialities share great proximity in terms of specific training, with ACI internships including a long rotation in Pediatrics. Close proximity between these professionals is therefore assured, promoting interactions that often display liminal characteristics when dealing with patients of pediatric age.
The third speciality referring the largest number of patients to the ACI OD was ENT. Respiratory diseases were the only reason for referral, showing the complementary approach of the two specialties to the study of airways.
AR and asthma have a high prevalence in pediatric age, being the most common chronic diseases in this population and having a great impact on patients’ quality of life and health care costs.14 In this study, respiratory diseases were the main cause fir referral to the ACI OD by all specialties. It is therefore crucial that these patients are referred early to ACI consultation, avoiding diagnostic and treatment delays.9 In 1998, Falcão H. et al. defined the criteria for admission and discharge of pediatric patients to the ACI OD.12 The authors also reported that most patients were referred to ACI from GP. As for the remaining specialities, the authors found ENT to be responsible for 18% of referrals, and pediatricians for 12%. In the present study, pediatricians referred 36% of cases, emphasising ACI’s increasing support to pediatricians. In both cases, the main reason for referral was respiratory diseases.12
Although DA were the second reason for general referral in this study (n=131; 17.4%), they were the main reason for referrals coming from pediatric hospitalization and ED (Table 2). Besides reflecting an increase in the incidence of these conditions, this also suggests that these cases should be more often investigated. DA suspicion frequently occurs while treating infectious diseases related to the respiratory system. The high variability of exanthematic reactions associated with infections, including viral ones, can often hinder the diagnosis.13 Clarifying suspected DA cases may prevent the use of drugs with low safety and efficacy and high cost.14 The number of cases referred to the ACI Department probably reflects a better targeted and justified referral to the ACI OD. On the other hand, the availability of distinct consultations for FA and DA may also partially account for the increase in referrals associated with both.12
Cutaneous diseases represented the third cause for general referral. These represent one of the first manifestations of allergic march, being the first step in the development and perpetuation of mechanisms leading to other conditions, such as FA, asthma, and AR.15,16
FA suspicion was the fourth reason for general referral and the third reason for pediatric referral. The frequency of referrals motivated by FA suspicion tripled within twenty years.12 Currently, FA is estimated to affect up to 10% of the pediatric population and 2% of the adult population globally with Europe reporting an increase in severe allergic reactions to food among children.19
Severe allergic reactions to Hymenoptera venom in children are scarce (0.15−0.3%), and in this study they comprised the fifth cause of referral to the ACI OD. Consultation for suspicion of this reaction was only requested by GP, who usually represented the first contact of patients after the sting, which generally occurs in rural areas.
The present study has the limitations intrinsic to a retrospective observational study, relying on the analysis of medical records, and to a unicentric study. Still, it provides insights that can contribute to improving the medical care provided by the ACI Department, namely through the development of protocols and implementation of measures to optimize the communication between medical specialities and ACI, avoiding diagnostic delays and improving patient management, with improved quality of life.
Authorship
Filipa Rodrigues dos Santos - Conceptualization; Writing - original draft; Data curation
Joana Gouveia - Data curation
Inês Falcão - Data curation
Maria Luís Marques - Writing - review & editing
Isabel Rezende - Writing - review & editing
Inês Cunha - Writing - review & editing
Eva Gomes - Writing - review & editing
Leonor Cunha - Writing - review & editing
Helena Falcão - Supervision; Writing - review & editing















