Introduction
Urinary tract infections (UTI) are among the most common bacterial infections in children.1,2 The overall prognosis for UTI is good, but early diagnosis and prompt antimicrobial treatment are needed to prevent renal scarring and progressive kidney damage.3 For this reason, children with suspected UTI should start empirical antibiotic therapy even before urine culture results are available.1 As antibiotic resistance increases worldwide, geographic variations in bacterial patterns and local antimicrobial resistance profiles are becoming apparent. Therefore, it is crucial for clinicians to know the local etiological agents of UTI and their susceptibility patterns in specific geographical areas.3,4 The aim of this study was to access community-acquired UTI pathogens in children and analyze their susceptibility patterns to the most commonly prescribed antibiotics in clinical practice in the area of influence of a hospital in northern Portugal during a three-year period.
Material and methods
A retrospective observational study was conducted between July 2017 and June 2020 in the Pediatric Emergency Department of Centro Hospitalar de Trás-os-Montes e Alto Douro, a secondary care hospital in the northern Portugal. Patients were children under 18 years of age. All urine samples obtained from patients with suspected UTI were analyzed, and if positive, data on age, gender, urine culture results, etiological agent, and antimicrobial susceptibility pattern were retrieved from the patients’ medical records. Etiological agent and antimicrobial susceptibility data were stratified by patient age and gender and classified into four age groups: less than one year, one to three years, three to 16 years, and 16 to 18 years. This stratification intended to account for the particularities and urinary sphincter control characteristics of each pediatric subgroup. For study purposes, only the first urine sample per UTI episode, monomorphic bacterial growth samples, and bacterial growth greater than 105 colony-forming units (CFU)/mL by midstream clean-catch, 104-105 CFU/mL by transurethral bladder catheterization or any growth by suprapubic needle aspiration were considered. For children with multiple confirmed UTI episodes, bacteria were excluded if they were isolated more than once in a four-week period. Descriptive statistics were used to describe the sample characteristics and for data analysis.
Results
Patient characteristics
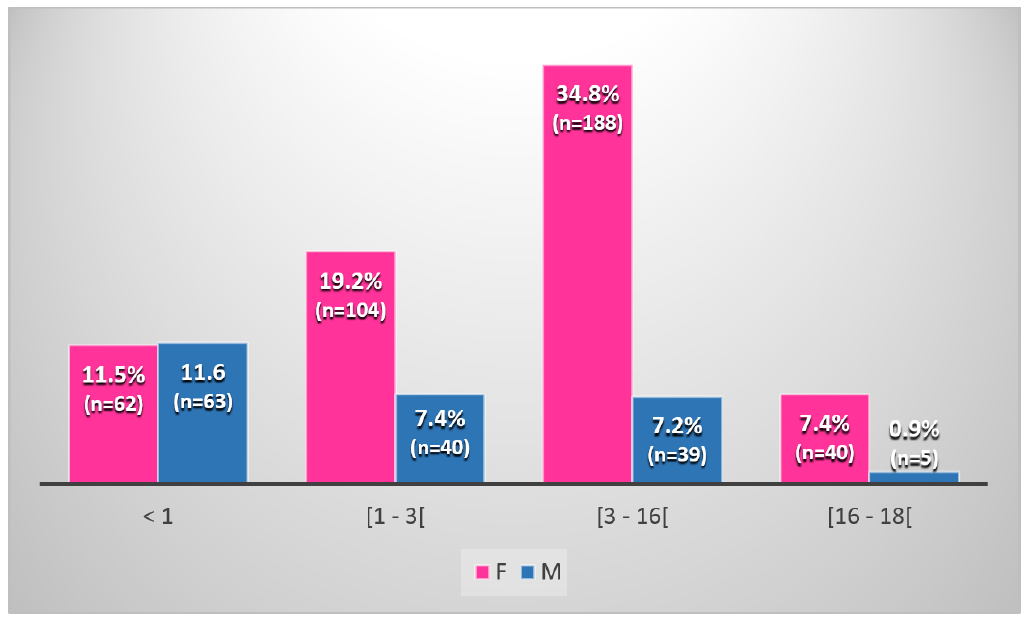
During the study period, a total of 2225 urine samples from children between two weeks and 17 years of age with suspected UTI were analyzed. Urine cultures were positive in 541 samples (24.3%), of which 394 (72.8%) were from female and 147 (27.2%) from male patients. The median age of females was three years and nine months, while the median age of males was one year and five months. A total of 125 patients (23.1%) were less than one year of age, 144 (26.6%) were between one and three years of age, 227 (42.0%) were between three and 16 years of age, and 45 (8.3%) were between 16 and 18 years of age. The male: female ratio in each subgroup was 1:1, 1:3, 1:5, and 1:8, respectively (Figure 1).
Etiological agents
Escherichia coli was the most frequently isolated uropathogen (n = 416, 76.9%), followed by Proteus mirabilis (n=82, 15.1%) and Klebsiella spp. (n=25, 4.6%). Although E. coli was the most commonly isolated pathogen in both genders, it was more prevalent in females (83.0%) than in males (60.5%). On the other hand, P. mirabilis was more prevalent in males (30.6%) than in females (9.4%), being the main etiological agent of UTI in male children between three and 16 years of age. Staphylococcus saprophyticus was the second most common uropathogen isolated from urine samples of females over 16 years of age (12.5%) but was not found in males. The distribution and frequency of uropathogens by gender and age group are detailed in Table 1.
Table 1 Distribution of isolates by microorganism, gender, and age group
| Microorganism | Age group | Global | |||||||||||||
| <1 | [1 - 3[ | [3 - 16[ | [16 - 18[ | ||||||||||||
| Total# (N=125) | Females§ (n=62) | Males§ (n=63) | Total# (N=144) | Females§ (n=104) | Males§ (n=40) | Total# (N=227) | Females§ (n=188) | Males§ (n=39) | Total# (N=45) | Females§ (n=40) | Males§ (n=5) | Total# (N=541) | Females† (n=394) | Males† (n=147) | |
| Escherichia coli | 84.8 | 91.9 | 77.8 | 72.9 | 80.8 | 52.5 | 75.3 | 82.4 | 41.0 | 75.6 | 77.5 | 60.0 | 76.9 | 83.0 | 60.5 |
| Proteus mirabilis | 5.6 | 1.6 | 9.6 | 22.9 | 15.4 | 42.5 | 16.7 | 9.6 | 51.3 | 8.9 | 5.0 | 40.0 | 15.1 | 9.4 | 30.6 |
| Klebsiella spp. | 7.2 | 4.8 | 9.6 | 2.8 | 2.9 | 2.5 | 4.8 | 4.2 | 7.7 | 2.2 | 2.5 | 0.0 | 4.6 | 3.8 | 6.8 |
| Staphylococcus saprophyticus | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.9 | 1.1 | 0.0 | 11.1 | 12.5 | 0.0 | 1.3 | 1.8 | 0.0 |
| Enterococcus faecalis | 0.8 | 1.6 | 0.0 | 0.7 | 0.0 | 2.5 | 0.4 | 0.5 | 0.0 | 0.0 | 0.0 | 0.0 | 0.6 | 0.5 | 0.7 |
| Pseudomonas aeroginosa | 0.8 | 0.0 | 1.6 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 0.0 | 2.2 | 2.5 | 0.0 | 0.4 | 0.2 | 0.7 |
| Others* | 0.8 | 0.0 | 1.6 | 0.7 | 1.0 | 0.0 | 1.7 | 2.1 | 0.0 | 0.0 | 2.5 | 0.0 | 1.1 | 1.3 | 0.7 |
| Total† | 23.1 | 11.5 | 11.6 | 26.6 | 19.2 | 7.4 | 42.0 | 34.8 | 7.2 | 8.3 | 7.4 | 0.9 | 100.0 | 72.8 | 27.2 |
# Frequency determined in relation to N; § Frequency determined in relation to n; † Frequency determined in relation to the total number of isolates. * Enterobacter cloacae, Enterobacter aerogenes, Citrobacter amalonaticus, Morganella morganii, Kluyvera ascorbata
Antibiotic susceptibility profile
In vitro susceptibility testing showed that the susceptibility of E. coli to cefuroxime was greater than 90% in all age groups, with all isolates from females under one year old and from males over three years old being susceptible to this antibiotic. In all age groups, E. coli isolates from females were more susceptible to amoxicillin-clavulanic acid than E. coli isolates from males. Males between one and three years old had a susceptibility rate to this antibiotic of only 38.1%. In children over 16 years old, all isolates were susceptible to fosfomycin and nitrofurantoin, showing susceptible rates above 90% to cefuroxime, gentamicin, and co-trimoxazole. E. coli antimicrobial susceptibility profile according to age group and gender is shown in Table 2.
Table 2 Antibiotic susceptibility patterns of Escherichia coli isolated from urine samples. Values in frequencies.
| Antimicrobial agent | Age group | ||||||||||||
| <1 | [1 - 3[ | [3 - 16[ | [16 - 18[ | ||||||||||
| Total | Females | Males | Total | Females | Males | Total | Females | Males | Total | Females | Males | ||
| Ampicillin | S I R | 40.7 0.0 59.3 | 42.2 0.0 57.8 | 39.0 0.0 61.0 | 26.9 0.0 73.1 | 31.1 0.0 68.9 | 11.8 0.0 88.2 | 36.2 0.0 63.8 | 34.0 0.0 66.0 | 54.5 0.0 45.5 | 30.4 0.0 69.6 | 30.0 0.0 70.0 | 33.3 0.0 66.7 |
| Amoxicillin/clavulanic acid | S I R | 88.6 0.0 11.4 | 89.5 0.0 10.5 | 87.5 0.0 12.5 | 77.1 0.0 22.9 | 86.9 0.0 13.1 | 38.1 0.0 61.9 | 91.8 0.0 8.2 | 92.3 0.0 7.7 | 87.5 0.0 12.5 | 79.4 0.0 20.6 | 80.6 0.0 18.4 | 66.7 0.0 33.3 |
| Cefuroxime | S I R | 98.1 0.0 1.9 | 100.0 0.0 0.0 | 95.9 0.0 4.1 | 93.3 0.0 6.7 | 94.0 0.0 6.0 | 90.5 0.0 9.5 | 98.8 0.0 1.2 | 98.7 0.0 1.3 | 100.0 0.0 0.0 | 93.8 0.0 6.2 | 93.1 0.0 6.9 | 100.0 0.0 0.0 |
| Gentamicin | S I R | 93.2 1.4 5.4 | 89.7 2.6 7.7 | 97.1 0.0 2.9 | 90.9 0.0 9.1 | 92.8 0.0 7.2 | 84.2 0.0 15.8 | 89.6 2.1 8.3 | 90.2 2.3 7.5 | 81.8 0.0 18.2 | 96.2 0.0 3.8 | 95.8 0.0 4.2 | 100.0 0.0 0.0 |
| Co-trimoxazole | S I R | 81.0 0.0 19.0 | 76.6 0.0 23.4 | 86.5 0.0 13.5 | 79.8 0.0 20.2 | 82.1 0.0 17.9 | 71.4 0.0 28.6 | 83.1 0.6 16.3 | 82.7 0.7 16.6 | 87.5 0.0 12.5 | 93.8 0.0 6.2 | 93.1 0.0 6.9 | 66.7 0.0 33.3 |
| Fosfomycin | S I R | - - - | - | - | - | - | - | - | - | - | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 |
| Nitrofurantoin | S I R | - - - | - | - | - | - | - | - | - | - | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 |
S - Susceptible, I - Intermediate, R - Resistant
P. mirabilis had a susceptibility of 100% to cefuroxime and amoxicillin-clavulanic acid in children under 16 years of age, except when isolated from females between one and three years of age, where susceptibility decreased to 93.8%. The number of P. mirabilis isolates was low in children over 16 years, with this agent being susceptible to all antibiotics tested except nitrofurantoin in females. In males, a high susceptibility rate was observed only for gentamicin and co-trimoxazole (Table 3). In all age groups, a high resistance rate to ampicillin was observed for E. coli and P. mirabilis, although it was higher for the former.
Table 3 Antibiotic susceptibility patterns of Proteus mirabilis isolated from urine samples. Values in frequencies.
| Antimicrobial agent | Age group | ||||||||
| <1 | [1 - 3[ | [3 - 16[ | [16 - 18[ | ||||||
| Females | Males | Females | Males | Females | Males | Females | Males | ||
| Ampicillin | S I R | - | 60.0 0.0 40.0 | 71.4 0.0 28.6 | 60.0 0.0 40.0 | 40.0 0.0 60.0 | 55.6 0.0 44.4 | 100.0 0.0 0.0 | 0.0 0.0 100.0 |
| Amoxicillin/clavulanic acid | S I R | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 93.8 0.0 6.2 | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 50.0 0.0 0.0 |
| Cefuroxime | S I R | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 50.0 0.0 0.0 |
| Gentamicin | S I R | - | 100.0 0.0 0.0 | 100.0 0.0 0.0 | 68.8 0.0 31.2 | 70.6 17.6 11.8 | 73.7 10.5 15.8 | 100.0 0.0 0.0 | 100.0 0.0 0.0 |
| Co-trimoxazole | S I R | 100.0 0.0 0.0 | 80.0 0.0 20.0 | 93.8 0.0 6.2 | 64.7 5.9 29.4 | 72.2 0.0 27.8 | 85.0 10.0 5.0 | 100.0 0.0 0.0 | 100.0 0.0 0.0 |
| Fosfomycin | S I R | - | - | - | - | - | - | 100.0 0.0 0.0 | 0.0 0.0 100.0 |
| Nitrofurantoin | S I R | - | - | - | - | - | - | 0.0 0.0 100.0 | 0.0 0.0 100.0 |
S - Susceptible, I - Intermediate, R - Resistant
All Staphylococcus saprophyticus were susceptible to amoxicillin-clavulanic acid, gentamicin, co-trimoxazole, and nitrofurantoin, and 25.0% resistance to fosfomycin was observed in females over 16 years of age.
Table 4 Antibiotic susceptibility pattern of Staphylococcus saprophyticus isolated from urine samples. Values in frequencies
| Antimicrobial agent | Age group | ||||||||
| <1 | [1 - 3[ | [3 - 16[ | [16 - 18[ | ||||||
| Females | Males | Females | Males | Females | Males | Females | Males | ||
| Ampicillin | S I R | - | - | - | - | 0.0 0.0 100.0 | - | 50.0 0.0 50.0 | - |
| Amoxicillin/clavulanic acid | S I R | - | - | - | - | 100.0 0.0 0.0 | - | 100.0 0.0 0.0 | - |
| Gentamicin | S I R | - | - | - | - | 100.0 0.0 0.0 | - | 100.0 0.0 0.0 | - |
| Co-trimoxazole | S I R | - | - | - | - | 100.0 0.0 0.0 | - | 100.0 0.0 0.0 | - |
| Fosfomycin | S I R | - | - | - | - | 0.0 0.0 100.0 | - | 25.0 0.0 75.0 | - |
| Nitrofurantoin | S I R | - | - | - | - | 100.0 0.0 0.0 | - | 100.0 0.0 0.0 | - |
S - Susceptible, I - Intermediate, R - Resistant
Discussion
Of 2225 patients with suspected UTI, 24.3% had a positive urine culture. This is a higher rate compared to other studies, which reported values ranging between 7.2% to 17.0%.4,5 Although 49.7% of patients were under three years of age and thus unable to specify symptoms, this may be explained by the common practice at the study hospital of collecting urine from all children with non-specific symptoms early in the course of the disease.
UTI have been described as being more common in female and uncircumcised male infants because of the shorter female urethra, shorter distance between the anusand the urethra in females, and the surface area of the foreskin in uncircumcised males.2 In this study, the prevalence of UTI was higher in females than in males in all considered age groups, except in infants under one year of age, where the male-to-female ratio was 1:1. The female-male disparity increased with age. In contrast to this finding, UTI have been reported to be more common in males under one year of age, with male-to-female ratios of 1:2 to 1:4.4 A possible explanation for this could be a lower incidence of congenital anomalies of the kidney and urinary tract (CAKUT) in males in this study population compared to other studies, as CAKUT is more common in males and has been associated with a higher incidence of UTI.6,7 Nevertheless, this warrants further investigation.
Several studies have identified E. coli as a leading cause of bacterial UTI in pediatric patients. In Portugal, the prevalence of E. coli varies between 53% and 81%.5,8-10E. coli was the most frequent uropathogen identified in northern Portugal in all age groups (76.9%), which is in agreement with other country regions.10
Some studies have identified Pseudomonas aeruginosa or Klebsiella spp. as the second most prevalent etiological agents of UTI in pediatric age,5,8 while others have identified P. mirabilis instead.9 In the present study, P. mirabilis was the second most common uropathogen isolated (15.1%) and was the leading cause of UTI in males between three and 16 years of age, in line with various other studies identifying this agent as the most common in males.9,11,12
In female adolescents over 16 years of age, Staphylococcus saprophyticus was the second most common pathogen after E. coli. This is consistent with other studies reporting that this agent is common in female adolescents, especially sexually active ones, and accounts for 3.6% to 42.3% of UTI in women worldwide.11,16
E. coli and P. mirabilis accounted for 92.0% of isolates in this study’s sample, suggesting that the chosen empirical antibiotic therapy is highly active against these agents. According to the 2012 Portuguese recommendations for UTI in pediatric age, resistance rates of E. coli to cefuroxime range from 1.2% to 4%.10 This study’s results document a high resistance to this second-generation cephalosporin in the region, highlighting that the antibiotic susceptibility profile of microorganisms is changing and should be further explored in additional studies. Notwithstanding, cefuroxime should be considered as a first-line option for uncomplicated UTI in this region, as its effectiveness against E. coli and P. mirabilis is higher compared to other antibiotics tested, including amoxicillin-clavulanic acid. Although the use of amoxicillin-clavulanic acid is very common in UTI in pediatric age, the results of this study indicate that it should be avoided in males aged from one to three years in this region of Portugal, since E. coli has a lower susceptibility to this antibiotic in this age group. To the authors’ knowledge, this low susceptibility rate has not been previously described and is the most important finding of this study. A possible explanation for this could not be found as the percentage of children with CAKUT, urological dysfunction, or taking chronic antimicrobial prophylaxis in this group was low. Further studies should thus be performed in the subgroup of males aged one to three years. Males over 16 years of age also showed low susceptibility to amoxicillin-clavulanic acid, but the ability to draw conclusions is limited by the reduced number of isolates in this study.
In Centro Hospitalar de Trás-os-Montes e Alto Douro, fosfomycin and nitrofurantoin are used only in children over 16 years of age, as they are mostly indicated in adolescents.10 Data from males over 16 years of age were limited in this study due to the small sample size, but in females, all E.coli and P. mirabilis isolates were susceptible to fosfomycin. The same was not true for Staphylococcus saprophyticus, which showed high resistance to this antibiotic, as expected. Data on nitrofurantoin were also limited in this study, but this agent was active against all 31 female E. coli isolates. The Portuguese recommendations state that both fosfomycin and nitrofurantoin are excellent treatment options for uncomplicated cystitis in adolescents, but nitrofurantoin seemed to be a better option in this study.10
This study has some limitations that should be acknowledged, including the low number of positive urine cultures in some age groups, the analysis of urine cultures without considering all patients’ clinical data, and the limited number of antibiotics tested in some age groups. Despite these limitations, study results showed that although amoxicillin-clavulanic acid is the first choice for UTI in the region, cefuroxime can be considered for empirical treatment of febrile and afebrile UTI in pediatric patients, especially in males between one and three years of age, given the low susceptibility rate of E. coli in this group.
Conclusions
Patients’ age and sex, as well as knowledge of the local prevalence of bacterial organisms and the respective antibiotic susceptibility profile, should always be taken into account for the best empirical antibiotic selection. Given the lack of recent data in the Portuguese pediatric population, local and national studies should be conducted to optimize empirical antibiotic therapy in this population.
Authorship
Susana Cláudia Teixeira - Conceptualization; Data Curation; Methodology; Software; Writing - original draft;
André Coelho Almeida - Data Curation; Formal Analysis; Writing - review & editing;
Joana Carvalho - Methodology; Validation; Writing - review & editing;
Aida Sá - Validation; Writing - review & editing;
Angela Martins - Formal Analysis; Software; Writing - review & editing;
António Trindade - Validation; Writing - review & editing