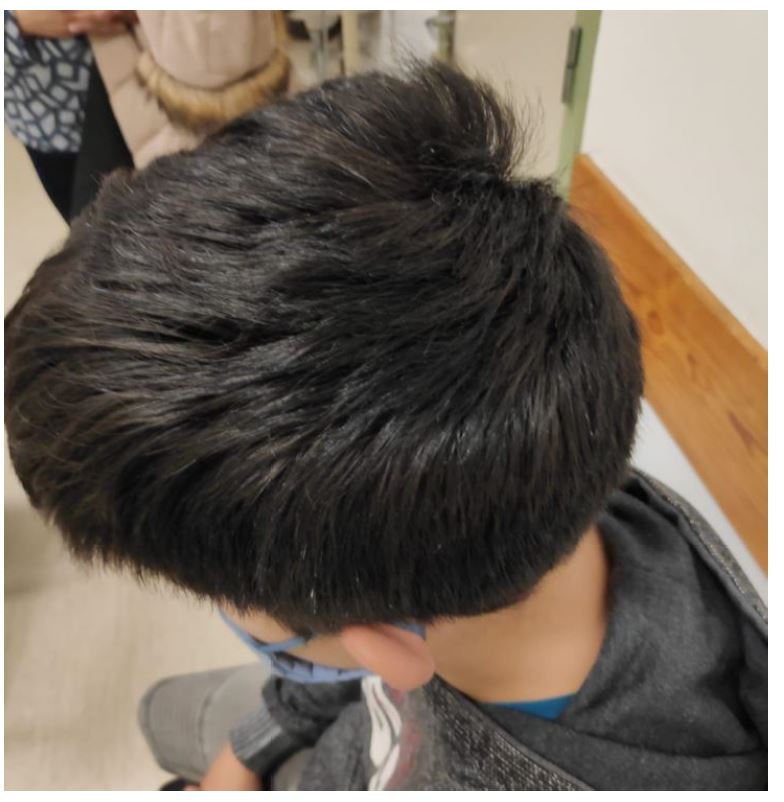
A previously healthy eight-year-old boy was referred to the pediatric consultation with a chief complaint of asymptomatic, non-scarring scalp hair loss with seven months of evolution. The hair loss had started as circular patches in the frontal region only, later spreading to the occipital region and then to the parietal and frontal regions (Figure 1 and 2). There was no scalp erythema, desquamation, or edema; no involvement of eyelashes, nasal hair, or nails; and no other clinical manifestations. No similar cases in family members, systemic diseases, history of drug use, or trauma were reported, and no contact with pets was mentioned. Hair examination with potassium hydroxide showed no fungal elements, and fungal culture was negative. Physical examination was otherwise unremarkable. The condition had a significant impact on the patient’s life, causing him to wear a hat to cover his scalp at all times.
What is your diagnosis?
Discussion
The diagnosis of alopecia areata was easily established in this clinical case due to the progressive hair loss. Alopecia areata is an autoimmune disease that targets the hair follicles, causing nonscarring hair loss through inflammation of the hair follicles. Treatment is often challenging. Several off-label options are available for children.1 In this case, the child was initially treated with topical minoxidil 2% once daily and the dietary supplement Ecophane®, with no significant improvement after a few months of treatment. Due to lack of response, he was referred to the Dermatology consultation and started on topical tacrolimus 0.1% ointment twice daily and topical hydrocortisone 1 mg/mL ointment every morning.
Because of the significant impact on daily life and because alopecia areata is often associated with psychiatric disorders, the patient was also referred to a child and adolescent mental health clinic. Although he had never exhibited psychiatric symptoms before, the development of alopecia patches led to oppositional behavior, agitation, and initial insomnia. He also began to have difficulty relating to peers, isolating himself from others, becoming disobedient, with disruptive behavior and poor concentration that ultimately affected his school performance. He confided that he was being bullied at school, with kids calling him bald. The child’s mother was overly protective and admitted to a difficult family background, with both parents unemployed and the father spending a lot of money on cigarettes. The boy underwent a Conners evaluation with a diagnosis of attention deficit hyperactivity disorder and was started on methylphenidate. He was also diagnosed with depression as a result of the physical impact of the disease on his self-image and was medicated with fluvoxamine.
The patient was reevaluated seven months after treatment initiation, still with no hair growth, and started on a stronger topical corticosteroid, clobetasol proprionate 0.5 mg/g ointment, and increased minoxidil to the 5% formulation once daily, while maintaining tacrolimus 0.1% twice daily (Figure 2). It was only after this very aggressive treatment and significant mood improvement with intensive psychotherapy that hair growth was observed in the parietal region. After four years of intensive treatment, the boy achieved complete hair regrowth and all treatments were discontinued (Figure 3). His mood improved significantly and he stopped wearing a hat.
Because alopecia areata is a chronic, immune-mediated, inflammatory disease that is often associated with other autoimmune disorders, such as vitiligo, thyroid abnormalities, and diabetes, the patient was screened for other autoimmune diseases at diagnosis and was positive for antithyroid antibodies and anti-neutrophil cytoplasmic antibodies (ANCA), despite the absence of clinical manifestations or changes in thyroid function.1 Currently, the boy has now been followed for five years with no changes in thyroid function, although he remains positive for antithyroid antibodies and negative for ANCA several months after starting treatment.
The authors raise awareness that alopecia areata may be an early sign of an autoimmune disease that may later manifest with other symptoms, and thus follow-up is warranted.1,2 Although most patients experience spontaneous hair regrowth within one year, the present patient required four years of treatment to achieve complete regrowth. Duration of disease and onset in childhood are poor prognostic factors.3 Thyroid dysfunction may be present at diagnosis or develop later in life, so reassessment is warranted if symptoms recur.4
Despite a variety of treatment options, alopecia areata remains difficult to treat and relapse is often difficult to prevent.5 The authors emphasize the importance of psychotherapy in these cases, as the condition can have a significant impact on children’s mental health, with several studies linking alopecia areata in adolescents to an increased rate of psychiatric symptoms.6 The present patient experienced a negative impact of the disease on his self-image, which likely affected his recovery.