Introduction
Childhood obesity has become a major public health problem in many developed countries around the world.1)
As the prevalence of obesity increases, so does the prevalence of associated comorbidities. Therefore, it is imperative that health care providers identify overweight and obese children so that counseling and treatment can be provided as soon as possible. Evaluation should include a complete history and physical examination, as well as an assessment of associated comorbidities and treatable causes.2
Family, school, and community involvement are critical to ensuring better outcomes by providing an environment and opportunities for healthy choices.2 Therefore, cases of extreme obesity are often associated with the inability of caregivers to adhere to a previously established plan, despite having been educated and warned about the health risks associated with this condition.
Clinical case
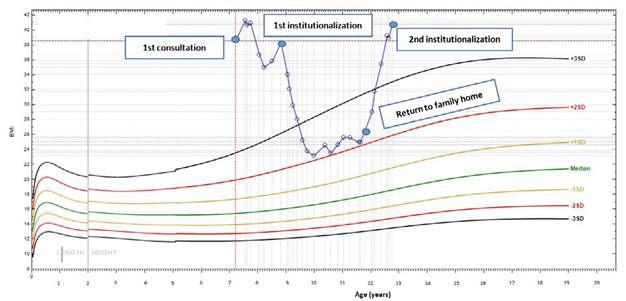
A seven-year-old girl was referred to the Pediatric Nutrition consultation for obesity since the first year of life with recent worsening. She presented with a weight of 76.3 kg (above the 97th percentile), a height of 140.6 cm (above the 97th percentile), and a body mass index (BMI) of 38.6 kg/m2 (BMI z-score +7.3; >+3 standard deviation [SD]). At the time of evaluation, the girl was Tanner 2, without menarche (which occurred at the age of eleven). She presented with hepatic steatosis with normal transaminases, hyperinsulinism (insulin 25.4 mg/dL [normal below 15 mg/dl]3), and obstructive sleep apnea.
The girl was in the second grade, with reasonable school performance. She slept an average of 9-10 hours per night and had no access to electronic devices at bedtime. Screen time was age appropriate. A family history of obesity in the parents and paternal grandparents was reported. She came from a dysfunctional family with an undefined primary caregiver and hostile interactions among adult family members. The household consisted of her parents, paternal grandparents, and paternal great-grandmother. Her maternal brother had been removed from the household as a child.
Her health condition continued to deteriorate over the next year despite multiple attempts to control weight gain. Multiple nutrition education sessions and articulation with her school teachers and school cafeteria were conducted to maximize intervention results. Psychological support was provided using techniques such as motivational interviewing to try to change her behavior.
Despite a thorough attempt to change her diet at home, there was no improvement, so the girl was admitted to pediatric inpatient care during her summer vacation. With the help of nutritionists and physical therapists, the two-week inpatient stay was designed to show her family that a balanced diet and regular exercise would have a positive outcome.
Despite the remarkable changes the girl made in this short period of time, losing 3 kg, her caregivers were unable to maintain a lasting behavioral change at home. The girl began to miss several medical appointments, her health deteriorated, and she was diagnosed with hypertension and hypercholesterolemia. She eventually reached a maximum BMI of 41.3 kg/m2 (BMI z-score +7.43; >+3SD).
A multidisciplinary group meeting was held with pediatricians, nutritionists, and social workers, and the girl was removed from her family and placed in a children’s home, with follow-up at the hospital over the next few months.
In one year, she managed to lose an extraordinary amount of weight through regular physical activity (with dance and gym activities for one hour two/three times a week) and adequate nutrition, reaching a BMI of 23.5 kg/m2 (BMI z-score +2.06; between +3SD and +2SD). For the first time since the beginning of her follow-up, the girl appeared to be a happy child, with positive interactions and excellent academic performance.
After three years, she returned to her parents' home by court order and resumed her previous eating habits and lack of physical activity. This led to a worsening of her BMI, which reached 40.7 kg/m2 (BMI z-score 4.07; >+3SD) in one year, despite continuous information from the medical team to social services and the court.
Discussion
Childhood obesity is commonly caused by excess caloric intake combined with a genetic predisposition to weight gain. It should be emphasized that most children do not have an underlying endocrine or genetic predisposition to weight gain.1 Childhood obesity has become a global pandemic in developed countries, leading to a variety of medical conditions that contribute to increased morbidity and premature death.2,4 Obesity is essentially a multifactorial disease, as documented by several studies showing that it results from an interaction of environment, genetics, and social context.1,5,6 Today, children have more sedentary lifestyles, in part due to excessive use of electronic devices and less free time to play outdoors.
Although this is well documented, fewer studies have focused on environmental aspects, such as the impact of emotional and psychological distress on overweight/obesity. One study conducted in Germany found that parental monitoring was associated with more meals spent together, and consequently less screen time and less nutrient-dense food intake.5 There is also a focus on the relationship between a supportive and loving family and the development of self-regulatory skills and adaptive coping behaviors that lead to less binge eating and appetite upregulation.1,6
In extreme cases, such as the one presented, it is important to define whether the behavior of the parents/caregivers can be considered child neglect. In the last decade, there have been several cases around the world, as serious or more serious, that have raised this question, so there has been an urgent need to define criteria. An American study conducted by pediatricians and a bioethics department defined three conditions that must be met in order to remove a child from his/her home: a high probability that serious imminent harm will occur; a reasonable probability that coercive state intervention will result in effective treatment; and the absence of alternative options to address the problem.5 In Portugal, a hospital committee composed of a pediatrician, a pediatric nurse, a social worker, and a legal advisor has been created to deal with children and/or adolescents at risk. They enable hospital doctors to report cases such as the one described and then discuss them with the Public Prosecutor’s Office.
According to the Committee for the Protection of Children and Adolescents, the primary objective should be to ensure support for the caregivers or, secondarily, to enable them to help the child to the best of their ability.7 The laws that protect children from this particular situation are: “Intervention for the promotion of the rights and protection of children and adolescents at risk occurs when parents or guardians put their safety, health, education, or development at risk, or when this risk results from an act or omission of a third party or the child/adolescent and they do not take appropriate action to eliminate it”.8 It also states that “a child or adolescent is at risk when he/she does not receive care and affection appropriate to his/her age or particular situation”.9)
In this particular case, all available resources had been exhausted and the patient met all of the above criteria. Despite arguments that it may not be fair to hold parents solely responsible, it should not be forgotten that parents or caregivers are responsible for their children, regardless of the cause of the disease, whether it is medical, behavioral, or interactional, or both.5
Prevention and management of childhood obesity is a challenging task that requires urgent attention and commitment from society, health care providers, and other stakeholders in related disciplines.
The cornerstone of pediatric weight management is behavioral strategies aimed at reducing total caloric intake, decreasing sedentary time, and increasing physical activity. In this process, parental involvement appears to be critical in changing habits.1)
Motivational interviewing is a patient-centered counseling technique that involves reflective listening, addresses the patient’s ambivalence about change, and uses the patient’s values to guide that ambivalence.1 A randomized clinical trial of motivational interviewing for the treatment of childhood obesity concluded that the use of motivational interviewing was able to achieve significantly greater reductions in BMI than other interventions.(10) Many studies support the use of this technique as an important tool in the treatment of childhood obesity, usually in combination with face-to-face counseling.11,12
Simple approaches to obesity prevention include promoting a balanced diet, sleep hygiene, and healthy lifestyle. The home, school, and community are critical settings in which behavioral and educational interventions can be implemented.4,13
In conclusion, removing children from their parents should be a multidisciplinary decision made after weighing the threshold of protecting the child and enabling him/her to lead a healthier life against the risk of psychological harm.
Authoship
Inês Azevedo - Writing - review & editing
Benedita Bianchi Aguiar - Writing - review & editing
Joana Silva - Writing - review & editing
Elizabeth Marques - Writing - review & editing
Maria José Silva - Writing - review & editing
Virgínia Monteiro - Writing - review & editing
Lúcia Gomes - Writing - review & editing
Miguel Costa - Writing - review & editing