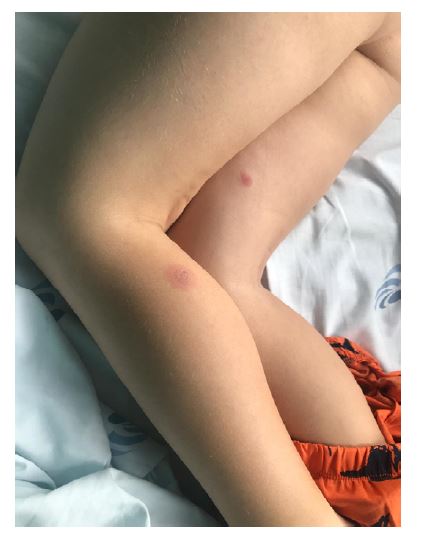
A previously healthy eight-year-old boy was admitted to the Emergency Department with a twelve-day history of worsening painful oral mucositis, a four-day history of low-grade fever, and a rash that appeared on the day of admission. He was on his fourth day of acyclovir for suspected herpetic gingivostomatitis. No other drugs were administered. On physical examination, the patient presented with bilateral purulent conjunctivitis, exuberant oral mucositis with diffuse oral mucosal sloughing, and hemorrhagic crusting on the lips. Scattered atypical target lesions characterized by rounded erythematous plaques with a central vesicle/blister were found on the neck and limbs (Figures 1, 2, and 3). No genital or palmo-plantar lesions were found.
Blood tests revealed mild neutrophilia (8600 neutrophils/µl), monocytosis (1500 monocytes/µl), and elevated C-reactive protein (10.78 mg/dl). Mycoplasma pneumoniae (MP) immunoglobulin M and G were positive. Serologic tests for herpes simplex I and II, cytomegalovirus, Epstein-Barr virus, human immunodeficiency virus, and Chlamydophila pneumoniae were negative.
What is your diagnosis?

Figure 1 Eight-year-old boy with hemorrhagic crusting of the lips and atypical target lesions in the left mandibular area
Discussion
A multidisciplinary team composed of pediatricians, a dermatologist, and an ophthalmologist was involved in the diagnosis and management of this patient. Supportive care was provided, including analgesia, intravenous hydration, and oral mucosal care - application of fusidic acid and a soothing balm to the lips and mouthwash with a lidocaine, nystatin, and sodium bicarbonate elixir. Ophthalmic examination revealed bilateral conjunctival hyperemia. Topical oxytetracycline ointment was applied. Oral prednisolone (0.5 mg/kg/day) was administered for five days and then tapered over fifteen days.
Complete resolution of the ophthalmologic findings was achieved in four days. There was significant resolution of the skin rash and oral mucositis, allowing for a gradual increase in oral intake. The patient was discharged on day 6. Complete healing of the mucosal and cutaneous lesions was observed ten days after admission.
MP infections affect the upper and lower respiratory tract and are usually mild. Up to 25% of patients with MP infections may have extrapulmonary complications, including mucocutaneous manifestations.1) Over the years, patients with this condition have been misdiagnosed within the spectrum of erythema multiforme (EM), Stevens-Johnson syndrome (SJS), and toxic epidermal necrolysis (TEN) due to overlapping clinical features.2
Classical SJS is more easily recognized, with the ill-appearing patient presenting with severe mucositis, atypical target lesions, and skin detachment associated with drug exposure. On the other hand, EM presents with variable mucosal lesions and acral or generalized typical target lesions, most commonly associated with herpes simplex virus infection. Between these two classic scenarios, there are many cases with overlapping features and different triggers (such as MP) that have historically been associated with SJS or EM.
In 2015, Canavan et al. reviewed 202 published cases and proposed the designation of MIRM as a distinct clinical entity.2
The demographic characteristics of the present patient are consistent with the epidemiology described in the literature, as MIRM is predominantly seen in young males (mean age: 11.9 ± 8.8 years).2 A recent pediatric study reported a MIRM frequency of 6.8% in children with community-acquired pneumonia who tested positive for MP.3
Although not fully understood, the pathophysiologic mechanisms responsible for MIRM are likely different from those of EM spectrum disorders involving type IV hypersensitivity reactions. In MIRM, skin damage is thought to result from immune complex deposition and complement activation leading to polyclonal B cell proliferation and antibody production. Another proposed mechanism is molecular mimicry between mycoplasma P1 adhesion molecules and a keratinocyte antigen.2
Despite many similarities, the clinical manifestations of MIRM are distinct from those of EM spectrum diseases. Typically, patients report a history of prodromal symptoms, including cough, malaise, and fever, up to one week before the mucocutaneous eruption. Except for fever, the present patient was asymptomatic. The most common clinical features of MIRM are marked mucositis and sparse skin involvement. Since EM rarely presents with mucositis and SJS/TEN presents with prominent cutaneous lesions, the extent of the eruption is a distinguishing feature of MIRM. Pronounced involvement of more than one mucosal membrane occurs in the majority of cases. The oral mucosa is most commonly affected, followed by ocular and genitourinary involvement. Mucosal lesions include erosions, ulcers, vesicles, bullae, and sloughing. Ocular findings include purulent bilateral conjunctivitis, eyelid edema, and photophobia. Skin lesions typically occur in a scattered, acral distribution, but truncal and generalized involvement is possible. Many patients present with polymorphic lesions. The most common morphologies are vesiculobullous and targetoid lesions. Papules, macules, and morbilliform eruptions are less common. A significant proportion of patients have no skin findings; moderate to severe cutaneous involvement is rarely documented.2,4
Ancillary studies are useful to confirm MP infection and may include MP immunoglobulin M antibodies, oropharyngeal or bullae culture, MP detection by PCR, or cold agglutinins. It is unknown whether there are pathognomonic histopathologic features of MIRM. The usefulness of biopsy is controversial.2,5)
The diagnostic criteria proposed by Canavan et al. for classic cases include the following: rash with less than 10% detachment of body surface area; two or more mucosal sites involved; vesicles, bullae, or scattered atypical target lesions; clinical or laboratory evidence of atypical pneumonia, including fever, cough, auscultatory findings, and laboratory markers of MP infection.2 This patient met all criteria except for clinical features of pneumonia.
There are currently no guidelines for the treatment of MIRM. Supportive care is generally accepted and includes analgesia, hydration, mucosal care, and ophthalmologic treatments. Most cases reported in the literature have been treated with antibiotics, systemic corticosteroids, and intravenous immunoglobulin, but there is no robust evidence to recommend them for the treatment of MIRM.2,5-7)
MIRM appears to have a good prognosis, which is another important difference from SJS/TEN. Most patients make a full recovery and relapses are rare.7 Mucosal synechiae and pigmentary changes are the most commonly described sequelae. Rare systemic complications include persistent cutaneous lesions and B-cell lymphopenia.2)
Authorship
Vera Gonçalves - Conceptualization; Investigation; Methodology; Writing - original draft
André Costa e Silva - Methodology; Writing - original draft
André Azevedo - Methodology; Writing - original draft
Isabel Martinho - Writing - review & editing
Sandrina Martins - Writing - review & editing
Vera Teixeira - Conceptualization; Investigation; Methodology; Supervision; Writing - review & editing