Introduction
The COVID-19 pandemic had a major impact on health care utilization and hospitalization.1,2 It is recognized that SARS-CoV-2 infection is usually mild in children, and the number of hospital admissions to pediatric units directly attributed to the disease is low.3,4 However, the indirect effects of SARS-CoV-2 on children’s health were substantial, and the restrictions imposed by pandemic containment dramatically changed the incidence of non-COVID-19 diseases.5
Since the emergence of SARS-CoV-2, Emergency Department admissions and hospitalizations from all causes decreased.6 In pediatrics, this was mainly due to a decrease in all common respiratory illnesses, such as bronchiolitis and pneumonia.7 However, admissions for invasive bacterial infections, such as meningitis and osteomyelitis, also decreased. This decrease was not as evident for admissions due to non-infectious conditions, such as pyelonephritis.6
The incidence of respiratory syncytial virus (RSV), which was responsible for many hospitalizations in young children before the pandemic, declined during the spread of SARS-CoV-2, even after major restrictions were lifted.8 The same was true for other common respiratory viruses, such as influenza.9
The first cases of COVID-19 in Portugal were diagnosed in March 2020, and the lockdown and school closure were announced the same month. Childcare centers and nurseries gradually opened from May 2020, and schools from mid-September 2020. However, sanitary measures were still mandatory, namely the use of face masks for staff, parents, and older children, physical distancing, and quarantine and isolation according to recommendations. These restrictions were lifted in May 2021.10
The aim of this study was to evaluate the impact of the pandemic on children’s hospitalizations and diagnoses in a level II hospital. This is the first Portuguese study to analyze the impact of COVID-19 on children´s admissions for other diseases.
Material and methods
A retrospective analysis was conducted including all children admitted to a Portuguese level II hospital between March 2020 and December 2021. Data were collected from medical records and included demographics (gender and age), number of admissions and diagnoses, and hospital length of stay. These data were analyzed and compared with the homologous period before the COVID-19 pandemic, from March 2018 to December 2019.
During the study period, no children with SARS-CoV-2 infection were admitted to the study hospital because the health authorities declared that they should be admitted to level III hospitals. Therefore, all children who tested positive for SARS-CoV-2 before or after admission and required inpatient care were transferred to other units.
In the two periods analyzed, screening for respiratory viruses in nasopharyngeal secretions by antigen search (which includes RSV, influenza A and B, and adenovirus) was performed in cases with an indication for hospitalization in which the diagnosis of bronchiolitis was considered.
Diagnoses were classified according to the International Classification of Diseases, 10th Revision (ICD-10), and statistical analysis was performed using Microsoft Excel®.
Results were presented as absolute and relative frequencies for categorical variables and as medians for continuous variables. The chi-squared test was used to compare categorical variables, with the level of statistical significance set at p-value <0.05.
During hospitalization, caregivers were informed that their children’s anonymous data could be used for clinical research purposes.
Results
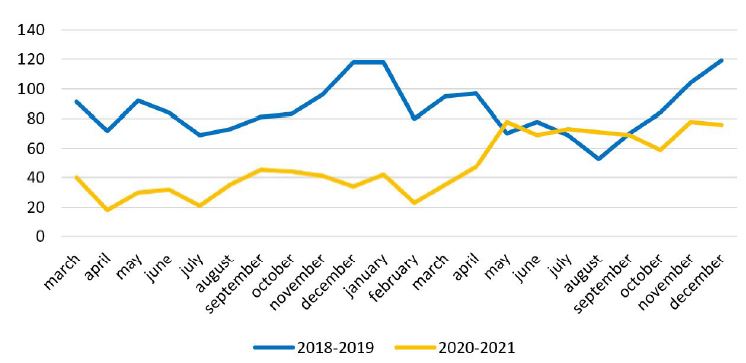
A total of 2956 admissions were analyzed: 1060 from March 2020 to December 2021 and 1896 from March 2018 to December 2019 (before the pandemic). These numbers show a 44.1% decrease in hospital admissions with the onset of the SARS-CoV-2 pandemic. The number of admissions per month during the years considered is shown in Figure 1.
A total of 166 children were admitted to the Intermediate Care Unit in 2020-2021, compared to 623 in 2018-2019 (Figure 2).
Patient demographics, hospital length of stay, Intensive Care Unit transfer, and mortality in the two time periods are described in Table 1.
Respiratory diseases were the most common during the pandemic period (n=331; 31.2%), followed by the group of symptoms, signs, and abnormal clinical and laboratory findings not elsewhere classified (n=126; 11.9%). From March 2018 to December 2019, respiratory diseases were already the most common (n=700; 36.9%), but their incidence was higher compared to 2020-2021. The incidence of infectious diseases was 12.5% (n=237) in 2018-2019 and decreased to 8.2% (n=87) in 2020-2021. The most common diagnoses and their incidence are shown in Table 2.
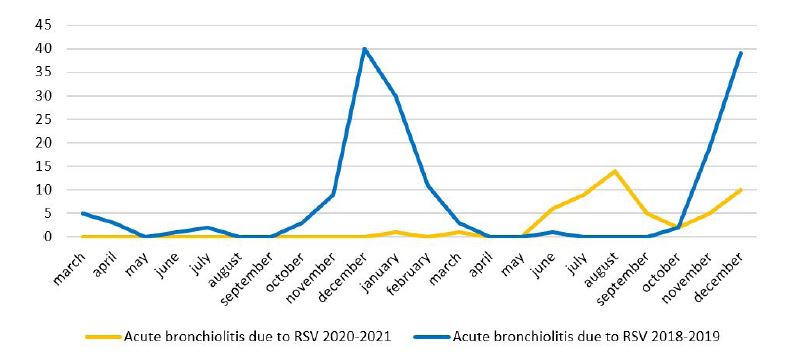
From March 2018 to December 2019, the incidence of acute bronchiolitis was 19.6% (n=372), and this number decreased to 17.1% (n=181) during the pandemic. However, this difference was not statistically significant (p: 0,089). The peak of bronchiolitis in late spring and summer 2021 was mainly due to RSV infection, as shown in Figures 3and4.
From March 2020 to December 2021, RSV was responsible for 5.0% (n=53) of all admissions and 29.3% (n=53) of all acute bronchiolitis episodes. No admissions due to influenza virus were observed during this time interval. Compared to the 2018-2019 reference period, 9.1% (n=172) of all admissions were due to RSV infection, and this virus was responsible for 46.2% (n=172) of all acute bronchiolitis episodes. The incidence of influenza virus infection was 1.2% (n=23).

Figure 2 Monthly Intermediate Care Unit admissions from March 2018 through December 2019 and from March 2020 through December 2021.
Table 1 Demographics, hospital length of stay, Intensive Care Unit transfer, and mortality of patients admitted before and after the SARS-CoV-2 pandemic.
| March 2018 - December 2019 | March 2020 - December 2021 | p-value | |
|---|---|---|---|
| Number of admissions, n | 1896 | 1060 | |
| Sex, n (%) | 0.183 | ||
| Male | 1034 (54.5%) | 605 (57.1%) | |
| Female | 862 (45.5%) | 455 (42.9%) | |
| Age (years), median | 2.6 | 4 | |
| Age group, n (%) | <0.001 | ||
| Newborn (<30 days) | 115 (6.1%) | 29 (2.7%) | |
| 1 to 12 months | 554 (29.2%) | 233 (22.0%) | |
| >1 and ≤5 years | 482 (25.4%) | 301 (28.4%) | |
| >5 and ≤10 years | 282 (14.9%) | 178 ( 16.8%) | |
| >10 and <18 years | 463 (24.4%) | 319 (30.1%) | |
| Length of hospital stay (days), median | 3 | 3 | |
| Transfer to the Intensive Care Unit | 10 (0.5%) | 4 (0.4%) | |
| Mortality | 0 (0%) | 0 (0%) |
Table 2 Incidence of the most common disease diagnoses from March 2020 to December 2021 and in the homologous period of 2018-2019.
| Group of diseases - n (%) | March 2018 - December 2019 | March 2020 - December 2021 | p-value |
|---|---|---|---|
| Diseases of the respiratory tract | 700 (36.9%) | 331 (31.2%) | |
| Acute bronchiolitis | 372 (19.6%) | 181 (17.1%) | 0.089 |
| Asthma | 33 (1.7%) | 22 (2.1%) | 0.518 |
| Pneumonia | 103 (5.4%) | 36 (3.4%) | 0.012 |
| Symptoms, signs, and abnormal clinical and laboratory findings not elsewhere classified | 157 (8.3%) | 126 (11.9%) | |
| Seizures | 70 (3.7%) | 36 (3.4%) | |
| Fever of unknown origin | 42 (2.2%) | 34 (3.2%) | |
| Wheezing | 25 (1.3%) | 20 (2.8%) | |
| External causes of morbidity and mortality | 164 (8.6%) | 123 (11.6%) | |
| Bone fracture | 131 (6.9%) | 97 (9.2%) | |
| Anaphylaxis | 12 (0.6%) | 1 (0.1%) | |
| Diseases of the digestive system | 189 (10.0%) | 123 (11.6%) | |
| Acute appendicitis | 128 (6.8%) | 85 (8%) | |
| Stomatitis | 19 (1.0%) | 12 (1.1%) | 0.739 |
| Infectious and parasitic diseases | 237 (12.5%) | 87 (8.2%) | |
| Infectious gastroenteritis | 155 (8.2%) | 51 (4.8%) | <0.001 |
| Bacteremia | 4 (0.2%) | 15 (1.4%) | |
| Sepsis | 11 (0.6%) | 4 (0.4%) | |
| Chickenpox | 33 (1.8%) | 0 (0.0%) | <0,001 |
| Diseases of the genitourinary system | 121 (6.4%) | 85 (8%) | |
| Acute pyelonephritis | 104 (5.5%) | 61 (5.8%) | 0.706 |
| Nephrotic syndrome | 0 (0.0%) | 9 (0.8%) | |
| Diseases of the skin and subcutaneous system | 117 (6.2%) | 51 (4.8%) | |
| Cellulitis | 68 (3.6%) | 35 (3.3%) | |
| Acute lymphadenitis | 18 (0.9%) | 8 (0.8%) | |
| Endocrine, nutritional, and metabolic diseases | 30 (1.6%) | 29 (2.7%) | |
| Type 1 diabetes mellitus | 21 (1.1%) | 24 (2.7%) | |
| Diseases of the nervous system | 49 (2.6%) | 22 (2.1%) | |
| Epilepsy | 19 (1.0%) | 12 (1.1%) | |
| Headache | 7 (0.4%) | 6 (0.6%) | |
| Diseases of the blood and blood-forming organs | 34 (1.8%) | 21 (2.0%) | |
| Immune thrombocytopenic purpura | 5 (0.3%;) | 8 (0.8%) | |
| Iron deficiency anemia | 8 (0.4%) | 7 (0.7%) |
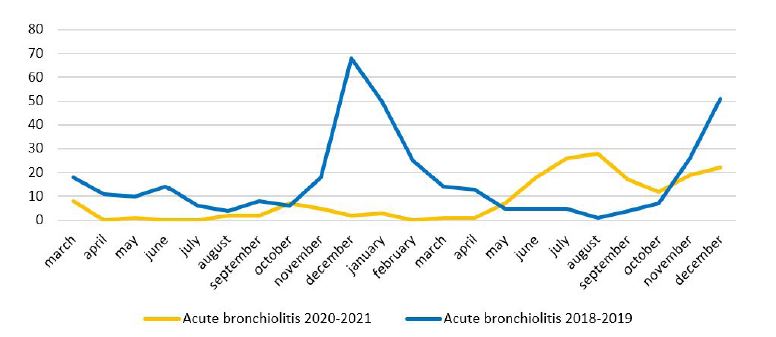
Figure 3 Monthly admissions for acute bronchiolitis from March 2020 to December 2021 and from March 2018 to December 2019
Discussion
Since the onset of the COVID-19 pandemic, there has been a significant decline in pediatric hospital admissions.6 The present study showed a 44% decrease in admissions during the pandemic compared to the same period in 2018-2019. Several studies conducted worldwide have shown similar results.2,11 This decrease may be multifactorial. School closure, along with social distancing measures, limited the transmission of common infectious diseases that were previously responsible for hospital admissions. In May 2021, when the use of face masks was no longer mandatory in schools and social distancing restrictions ended, there was a rebound in pediatric admissions.
Regarding demographic data, this study’s results show a higher percentage of adolescents admitted to the hospital after the onset of COVID-19 compared to the reference period of 2018-2019 (p <0.001). At the same time, the relative number of newborns and infants admitted was lower (p<0.001). Stricter isolation of younger children, with higher parental control, could explain these figures. In addition, younger children are more susceptible to complications of respiratory infection,12 so the decrease in these diseases may have contributed to the lower number of admissions in this age group.
No hospitalizations due to RSV were recorded in 2020. Similar to other studies, this study found an increase in respiratory infections, mainly caused by RSV, when restrictions were eased in June 2021.13,14 RSV usually occurs in the fall and winter.8 However, the COVID-19 pandemic and social distancing measures delayed the RSV season until spring 2021. In addition, lack of immunity due to lack of exposure may have led to an increase in severity.13
As this study shows, during the pandemic there was an additional decrease in pediatric admissions due to other communicable diseases, such as acute gastroenteritis (p <0.001), chickenpox (p <0.001), and stomatitis (p: 0.739).15-17 This indicates that the measures used to contain the SARS-CoV-2 virus were also effective in preventing the spread of other infectious microorganisms.
Although not statistically significant (p: 0.706), the number of admissions for acute pyelonephritis was lower during the pandemic period. This finding was surprising because urinary tract infections are not communicable. However, this decrease has been seen in other studies and may be due to improved hygiene measures.18,19
This study has some limitations that should be acknowledged, such as the fact that the data were collected in a single center where no COVID-19 pediatric patients were admitted, and its retrospective nature, due to which the possibility of some diagnostic misclassification cannot be excluded.
Conclusions
In agreement with previous reports, this study showed that the COVID-19 pandemic had a major impact on pediatric hospital admissions, which decreased by 44%. Isolation and hygiene measures were effective not only in controlling the spread of SARS-CoV-2, but also in preventing other common and potentially serious communicable diseases. As the burden of other diseases decreased, this also allowed health services to better prepare for and manage the novelty and uncertainty of COVID-19.
Future studies are needed to understand whether the changes in respiratory virus epidemiology were only temporary.
Authorship
Maria Garrotes - Conceptualization; Data Curation; Formal Analysis; Writing
Madalena Ferreira - Data Curation; Formal Analysis; Writing
Luzia Condessa - Data Curation; Formal Analysis; Writing
Carolina Guimarães - Conceptualization; Data Curation; Formal Analysis; Writing
Madalena Fialho - Conceptualization; Writing
Manuel Sousa e Cunha - Conceptualization; Writing