Introduction
Malignant spinal cord compression (MSCC) is a rare but serious complication of pediatric malignancies that is a major cause of morbidity in children with cancer.1 Spinal cord compression-related symptoms may be the presenting feature of a new malignancy or the consequence of metastatic disease progression or recurrence.2) MSCC is associated with a poor prognosis and can lead to permanent neurologic deficits, including paralysis, sensory deficits, or sphincter dysfunction.2,3 Motor deficit is the most common initial symptom, followed by back or radicular pain and sphincter dysfunction.2,3 Prognosis appears to be related to the severity of symptoms at diagnosis, and treatment delay may result in preventable loss of function.2,4 Overall, MSCC represents an oncologic emergency, and timely diagnosis and treatment are essential to prevent permanent sequelae.
Case report
A nine-year-old girl with a history of constipation but otherwise healthy presented to the Emergency Department (ED) with left anterior iliac spine pain with one month of evolution and worsening over the previous three days. The pain was initially nocturnal but had become persistent. Constipation had worsened in the previous month, with no bowel movements in the previous week. Other symptoms such as fever and motor or sensory symptoms were denied. There was no history of trauma, recent infection, or drug ingestion. No significant personal or family medical history was reported. The girl had a previous outpatient pelvic and spine radiograph, which showed a slight lateral pelvic tilt with no other findings.
On admission, the patient was clinically well, with normal vital signs for her age and apyretic. She had a normal neurological and osteoarticular examination and palpable stool in the left iliac region on abdominal examination. Blood tests, including complete blood count and inflammatory markers, were normal, and the girl was discharged with a scheduled medical appointment.
She returned to the ED two days later with worsening pain associated with lower back pain in the supine position and progressive gait instability. She reported no other symptoms and remained apyretic, clinically well, and with normal vital signs for her age. She had lumbar pain on cervical flexion with negative meningeal signs. On neurological examination, the girl had normal mental status and cranial nerves. She had gait instability, no motor, sensory, or proprioceptive disturbances, normal knee and ankle reflexes, and flexor plantar reflex. The remainder of the neurological examination was unremarkable. Blood tests including inflammatory markers, lactate dehydrogenase, uric acid, alkaline phosphatase, vitamin B12, and folic acid were normal, as was the head computed tomography scan.
During the two days of hospitalization, she developed decreased strength (4/4 proximal, 4+/4+ distal) and sensation in the lower limbs, hyperreflexia with clonus in the lower limbs (grade 3/4 knee reflexes), proprioceptive disturbances, bilateral Babinski sign, and progressive inability to walk unassisted. Magnetic resonance imaging (MRI) of the head and spine performed 48 hours after admission revealed an extensive anterior intracanalicular lesion at D8-12 level measuring 63 mm in height and 15 mm in anteroposterior diameter. It caused left posterolateral deviation of the spinal cord with significant structural deformity compatible with compressive myelopathy (Figure 1).

Figure 1 Spinal magnetic resonance imaging showing an extensive epidural intracanalicular lesion from D8-9 to D12 measuring 63 x 15 mm, with low T2 signal and contrast enhancement, causing compressive myelopathy.
The patient was started on corticosteroid therapy and underwent surgical decompression by right D10-11 hemilaminectomy with partial removal of the tumor, with symptomatic improvement. In the postoperative period, she showed improvement in lower limb strength, no sensory disturbances, and was able to walk with minimal assistance with instability. At this time, the girl began chemotherapy. Anatomopathologic examination revealed Ewing sarcoma (Figure 2).
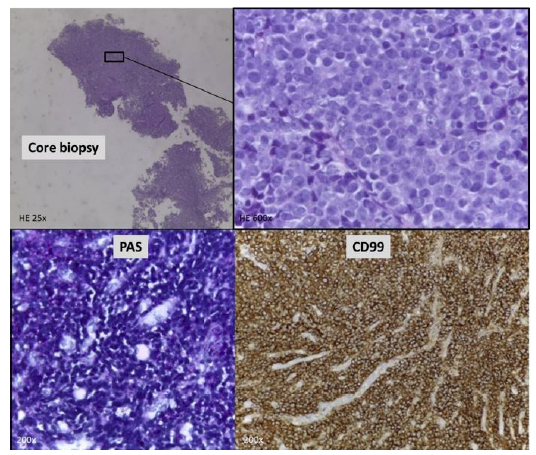
Figure 2 Core needle biopsy (HE 25x) - Higher magnification shows nests of small round blue tumor cells (HE 600x). Characteristic CD99 immunoreactivity of cell membranes and the presence of intracytoplasmic glycogen (PAS+) confirmed the diagnosis.
Bone marrow biopsy and myelogram showed no tumor involvement. Positron emission tomography showed only local involvement, and scintigraphy showed no bone metastases. Computed tomography of the lungs, abdomen, and pelvis showed no lesions. Three months after starting chemotherapy, she had normal muscle tone, 5/5 strength in the upper limbs, 4/4 proximal and 5/5 distal strength in the lower limbs, normal deep tendon reflexes, and no clonus, sensory disturbances, or ataxia. She was able to walk unassisted with slight instability. After completing six cycles of chemotherapy, she was able to walk unassisted with no instability and could stand on one leg. The MRI showed no evidence of residual tumor, and she was started on maintenance chemotherapy and radiotherapy. She repeated the MRI eight months later, which showed a good response to treatment and no evidence of malignancy. At the end of treatment, two years after diagnosis, the girl was asymptomatic and had 5/5 global upper and lower limb strength, normal reflexes, no sensory disturbances, and could walk normally without assistance or instability.
Discussion
MSCC is a rare but serious cancer complication that represents a medical emergency because it can lead to irreversible loss of neurological function if not treated promptly. Acute spinal cord compression occurs in 35% of children with cancer, more often at the time of initial cancer diagnosis, as in the present case, although it may also occur as a result of metastatic progression or relapse.5
The most common causes of MSCC are extramedullary tumors, most commonly neuroblastoma and soft tissue sarcomas (especially Ewing sarcoma), which are more commonly located in the thoracic and lumbosacral regions.1-3,6
The median age at diagnosis ranges from four to eight years, with an older median age of 10 years described for cases of MSCC secondary to soft tissue sarcomas.1-3) The incidence is similar in both genders.1,3
Motor deficit is the most common presenting symptom, usually developing in the time to diagnosis even in the few cases where it was not present initially, followed by pain and sphincter dysfunction.2,3) Pain is usually located in the back or limbs and is more common in older patients (>5 years).1,2) In the present case, the presenting symptom was pain in an unusual location (left anterior iliac spine), and ataxia and motor deficit developed later. There was no evidence of nerve root compression, especially L1 or L2 roots, although the spinal cord showed significant structural deformity at the D8-D12 level. Therefore, the referred pain mechanism was the most likely cause for the specific pain location, as no other causes were identified. At the second ED visit, the patient presented with gait instability, which was the first neurologic manifestation. Although no strength or proprioceptive disturbances were evident at this time, both developed over the following days, suggesting that the cause of gait instability was a combination of sensory ataxia due to probable posterior column dysfunction and strength deficit due to corticospinal tract damage.
The gold standard for MSCC diagnosis is spinal MRI, which has a high sensitivity and should ideally be performed within 24 hours.3,7) In the literature, the interval between the onset of symptoms and diagnosis ranges from 0 to 360 days.1,2) In this case, the interval was one month, but only two days after the onset of motor deficits.
Treatment modalities for MSCC depend on the tumor type and may include chemotherapy, radiotherapy, and neurosurgical decompression. Once the diagnosis is established, corticosteroids should be administered and a multidisciplinary team including oncology and neurosurgery specialists should be consulted.7) Most patients show clinical improvement with treatment.1
Prognosis and survival rates are intrinsically related to tumor type, with lymphoma having a better outcome after definitive therapy, followed by soft tissue sarcomas.1) They are also related to neurologic symptoms at diagnosis, with more severe motor deficits associated with worse neurologic outcomes after surgery.2,3) In a systematic review, the severity of neurologic motor deficit at diagnosis was the main predictor of neurologic outcomes.4) In another retrospective study, better functional outcomes were associated with slower development of motor deficits before treatment.8) Thus, prompt diagnosis and treatment are essential to reduce morbidity. In the present case, rapid diagnosis and management after the onset of motor deficit allowed complete recovery of neurologic function, reinforcing the importance of prompt action in these cases.
In conclusion, it is important to keep in mind that MSCC may have an atypical presentation, such as pain in an unusual location, and motor deficit may present later. Therefore, it is important to maintain a high index of suspicion for the manifestation of pain with warning signs, such as pain progression despite analgesic treatment and nocturnal symptoms, and to keep these patients under close observation. Pre-treatment neurologic function is the best predictor of post-treatment function, so early detection is essential to initiate timely treatment and improve prognosis.
Authorship
Maria João Gaia - Conceptualization; Writing - original draft
Vilma Lopes - Data curation; Writing - review & editing
Joana Tenente - Data curation; Writing - review & editing
Janine Coelho - Validation
Marta Vila Real - Supervision; Writing - review & editing
Fátima Santos - Supervision; Writing - review & editing















