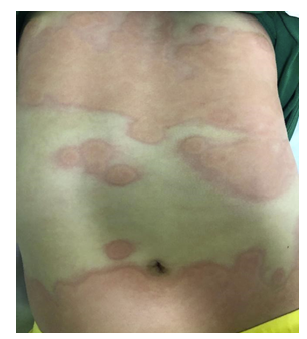
A previously healthy four-year-old boy was admitted to the Emergency Department (ED) for transient, annular, erythematous wheals on the face and trunk, sparing the palms and soles, with intense pruritus for the past six hours (Figure 1). First-generation antihistamines and oral corticosteroids were administered, and he was discharged home. Two days later, the boy returned to the ED with fever with four hours of evolution, persistent rash, and an episode of vomiting. On physical examination, he presented with an erythematous rash involving the face, trunk, and testicles (Figure 2), associated with mild edema of the lower limbs. The upper palate and buccal mucosa were intact and no other changes were present.
Due to the presence of a dusky ecchymotic rash and fever, laboratory tests were performed and revealed normal coagulation, platelet and white cell counts, and an elevated C-reactive protein of 28.8 mg/L (normal range <0.5 mg/L). The boy remained clinically stable and was discharged the next day on oral antihistamines. The rash gradually resolved with complete clearance of all lesions by day 5.
Discussion
Urticaria multiforme (UM), also known as acute annular urticaria, is an allergic hypersensitivity reaction classified as a morphologic subtype of urticaria. It is characterized by the acute onset of polycyclic and annular wheals with ecchymotic centers.1,2
The condition is more common in children between the ages of four months and four years, and its most known precipitating factors are infections, vaccinations, and medications, including systemic antibiotics and antipyretics.2-4 In the present case, no specific precipitating factor was identified.
Individual lesions usually last less than 24 hours and present initially as macules, papules, or plaques that rapidly progress to large, annular, and polycyclic wheals. They may present with central clearing or a dusky ecchymotic hue. Pruritus is an almost universal finding and was present in this child. Self-limiting angioedema of the face, hands, and feet is common in UM and is due to subcutaneous vascular leakage.1 Children present with a non-toxic appearance, and systemic symptoms are limited to a few days of mild fever.5 Diagnosis is clinical and does not require laboratory testing or skin biopsy.2 When blood tests are performed, acute phase reactants (white blood cell count, erythrocyte sedimentation rate, C-reactive protein) may be normal or mildly elevated.3) In this case, there was only a mild elevation of C-reactive protein with a normal complete blood count.
UM is probably underdiagnosed because it is often mistaken for erythema multiforme (EM) and serum sickness-like reaction. A thorough clinical diagnosis and complete physical examination can provide important clues to differentiate UM from these two skin conditions. Children with UM often have dermatographism, an allergic-like reaction that produces a red wheal after scratching or rubbing the skin, which is not seen in the other two conditions. In addition, acral and facial edema are rarely seen in patients with EM or serum sickness-like reactions.1,5
Erythema multiform classically presents with lesions surrounded by an inner ring of pale edema and an outer ring of erythema, and with a dusky center of epidermal necrosis, which may be confused with the lesions seen in UM.1 A distinction can be made when lesions progress to blistering or crusting necrosis, which does not occur in UM. In addition, mucous membranes are typically involved in EM, and symptoms such as burning and pain are common, whereas pruritus is seen only in UM.1,2
A serum sickness-like reaction may also manifest with polycyclic urticarial lesions, but the cutaneous findings are fixed. Children usually present with high fever and systemic symptoms such as myalgia, arthralgia, and lymphadenopathy.3
Cutaneous manifestations are very common in pediatric patients and may have a variety of differential diagnoses. Polycyclic annular lesions with an ecchymotic center presenting with an evanescent nature, associated with acral angioedema, pruritus, and dermatographism, and a favorable response to antihistamine therapy support the diagnosis of UM.
Treatment goal is to improve patient comfort − as the rash is typically pruritic − and may include discontinuation of all known triggering medications and administration of second-generation H1 antihistamines. Systemic corticosteroids are rarely required and should be reserved for severe cases refractory to antihistamine therapy.5
With this report, the authors aim to alert clinicians to this often misdiagnosed condition to avoid unnecessary laboratory testing and medication.
Authorship
Diana Alba - Conceptualization; Bibliographic search; Writing - original draft; Writing - review & editing
Sofia Pimenta - Conceptualization; Bibliographic search; Writing - original draft; Writing - review & editing
Ângela Machado - Validation; Writing - review & editing
Jorge Abreu Ferreira - Validation; Writing - review & editing