Introduction
Pediatric fractures of the proximal humerus typically occur through the growth plate and are most often classified as Salter-Harris type I fractures, with type II fractures being less common. These injuries result in separation of the epiphysis from the metaphysis.1 Birth-related injuries are rare, occurring in less than 1% of live births, with the incidence of birth-related humerus fractures estimated at 0.1 to 0.2 fractures per 1,000 live births.2
In neonates, fracture separation of the proximal humeral epiphysis due to birth trauma is a very rare injury, and its diagnosis can be challenging. In the absence of a visible epiphyseal ossification center, radiographic signs of epiphyseal dislocation (such as an enlarged joint space, nidus displacement, increased metaphyseal-epiphyseal distance, and metaphyseal bony fragments) may be missed.3-9
In this article, a literature review on this topic was conducted to better understand the diagnostic approaches and treatment options for this rare condition.
Case report
A 1085 g preterm male neonate was born at 28 weeks' gestation after an abnormal course of labor and emergency cesarean section due to fetal malpresentation. After a difficult extraction, the newborn presented with multiple areas of ecchymosis, particularly on the upper and lower limbs and penile region. Apgar scores were 0 at 1 minute, 2 at 5 minutes, and 6 at 10 minutes. After stabilization, the neonate was transferred to the Neonatal Intensive Care Unit.
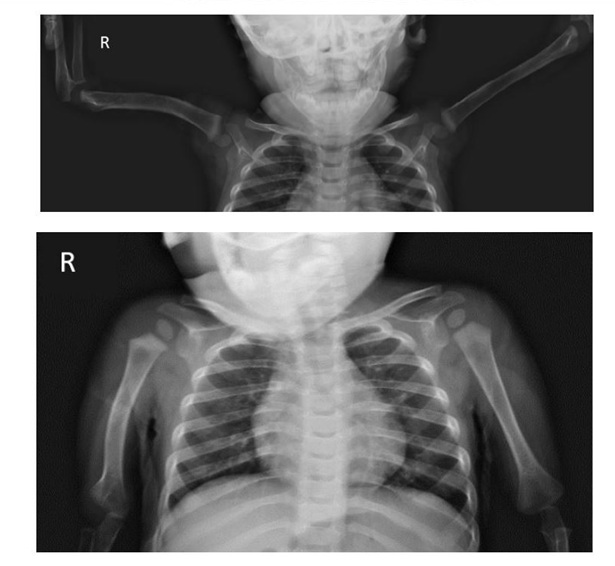
Internal rotation of the right upper arm was noted along with swelling and ecchymosis of the proximal soft tissues. Physical examination of the neck, clavicle, shoulder, and arm revealed no palpable abnormalities. Discomfort was noted with shoulder mobilization. Active range of motion and muscle strength could not be properly assessed. No abnormalities were observed in elbow, wrist, or finger motion. Neonatal brachial plexus palsy was initially considered; however, a shoulder dislocation was suspected after an initial radiograph on the first day of life (Figure 1).
On the second day of life, a shoulder ultrasound was performed to confirm the diagnosis. Instead, it revealed a separation of the proximal humeral epiphysis from the diaphysis, classified as Salter-Harris type I. The proximal end of the humeral shaft was found to be lateral and posterior to the humeral head (Figure 2).
After consultation with a pediatric orthopedic specialist, the fracture was managed with a splint for two weeks. The arm was stabilized against the lateral chest with the shoulder in adduction and internal rotation. In the following weeks, spontaneous movement of the arm and subjective improvement were observed.
Subsequent radiograph confirmed slippage of the humeral epiphysis, as evidenced by hypertrophic callus formation at the proximal metaphysis (Figure 3).
Follow-up radiographs at 13 months of age showed anatomic reduction of the fracture, as well as mild shortening of the right humerus and anterior bowing of the diaphysis. The ossification center of the humerus was symmetrical to the contralateral side, with no evidence of avascular necrosis (Figures 4 and 5). Physical examination revealed symmetrical range of motion in both arms.
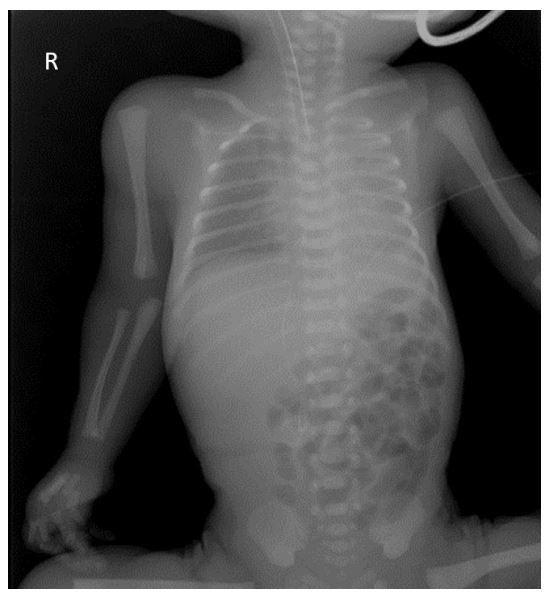
Figure 1 Plain chest radiograph showing no apparent fracture of the right arm. The asymmetry in the joint spaces of the shoulders with lateralization of the right humerus in the shoulder joint falsely suggested a shoulder dislocation.
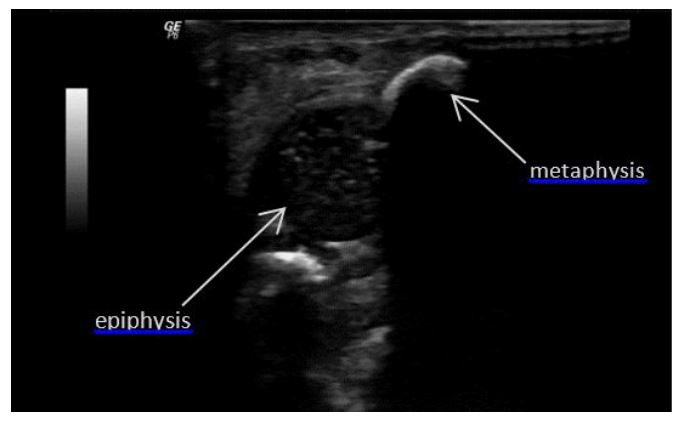
Figure 2 Longitudinal sonography of the right shoulder showing separation of the left humeral epiphysis from the metaphysis.
After two years, the patient shows no functional limitations, with only a slight shortening of the right humerus remaining. He continues to be followed by pediatric orthopedic surgery.
Discussion
Neonatal proximal humeral epiphyseal fractures, also known as epiphyseal separations, are rare.2,3,5,6-10
In neonates, such injuries typically result from traction on the upper limb during difficult vaginal or cesarean deliveries.2,3,8,10 Risk factors for obstetric injury include large or very small fetuses, shoulder dystocia, breech presentation, external cephalic version, difficult delivery, small uterine incision, inadequate uterine relaxation, prematurity, twin pregnancies, osteogenesis imperfecta, and osteoporosis.2,4,6 In the present case, the patient was a preterm newborn with malpresentation, which led to a difficult extraction and facilitated the occurrence of the fracture at birth.
The differential diagnosis for pain-induced postnatal arm posture includes rare humeral epiphysis fractures, diaphyseal fractures of the humerus or clavicle, brachial plexus injury, arthritis, and bone infection (osteomyelitis).5-7
A proximal humeral epiphysis fracture may present clinically with a bruised shoulder, swelling, tenderness, decreased active range of motion, and painful passive motion.4,6,7,10 In this case, all of these signs were present, but due to the extreme prematurity of the patient, active range of motion could not be adequately assessed.
Early diagnosis of this type of fracture is a significant challenge for clinicians. Because the center of humeral ossification is typically not visible on radiographs before 36 weeks of gestation, interpretation of these imaging studies can be difficult. As a result, the diagnosis of neonatal slipped epiphysis relies heavily on maintaining a high index of suspicion.2-6,9
Radiographic signs of a proximal humeral epiphyseal fracture (such as enlarged joint space, abnormal alignment, increased metaphyseal distance, and metaphyseal fragmentation) can be subtle and are often misinterpreted as shoulder dislocation.4-8 In cases where radiographs suggest shoulder dislocation, as in this case, clinicians must consider that neonatal epiphyseal cartilage is less resistant to trauma than ligaments or joint capsules. This fragility should rather raise suspicion for epiphyseal separation.4,6-8
Ultrasonography is an inexpensive, portable, simple, noninvasive, and readily available imaging modality for evaluating the periosteum, epiphysis, joint space, glenoid cavity, and vascular integrity of the neonatal shoulder.3-7 It provides clear visualization of the proximal humeral epiphysis and its relationship to the humeral metaphysis, facilitating early diagnosis and avoiding delays until callus formation, which typically becomes visible on radiographs at 10 to 14 days of age.6-8
Magnetic resonance imaging may also be helpful, and in rare situations, diagnostic arthrography may be required.4,6,8-10
Due to the rarity of this injury, treatment strategies are not well established, and the long-term prognosis is uncertain. The most effective treatment approach is still under debate.8-10
Although growth plate fractures of long bones generally require only conservative management, treatment can range from splinting to open reduction.4,8 Because of the remarkable remodeling potential of the proximal humerus during the neonatal period, these types of fractures are typically managed conservatively.3,8,9 Immobilization is usually achieved with a cast, traction, splint, or plaster cast, with the shoulder usually placed in adduction with neutral rotation or slight internal rotation and immobilized for 7 to 14 days.7,8,10
Although rare, closed reduction may not always be successful. El-Adl et al. reported eight cases of epiphyseal fractures that failed closed reduction and required reduction with Kirschner wires, with good outcomes.9 In the present case, nonsurgical management was chosen due to the critical condition of the neonate.
The overall prognosis for neonatal proximal humerus fractures is favorable, with minimal risk of vascular compromise of the epiphysis.3,10 Potential sequelae, although uncommon, include residual pain, limited shoulder abduction with residual varus deformity, humeral shortening (usually less than 2 cm and typically well tolerated), and malunion with residual angulation.6,7 The risk of complications increases with severe dislocation or delayed diagnosis.10 Therefore, accurate and early diagnosis is essential to ensure appropriate treatment and minimize the risk of long-term complications.6,10
Conclusion
Neonatal long bone fractures are of particular interest to obstetricians, neonatologists and pediatric orthopedic surgeons. Epiphyseal separation of the proximal humerus due to birth trauma is a rare condition with few cases reported in the literature. Traumatic injury to the proximal humeral epiphysis, especially after difficult vaginal or cesarean delivery, should be considered in newborns with limited or absent spontaneous shoulder joint function or when brachial plexus injury is suspected. A high index of suspicion is essential for early detection and treatment, and physicians should remain aware of this possibility.
Ultrasound plays a critical role in the diagnosis, as radiographs can be misleading due to the unossified epiphysis. If a proximal humerus epiphyseal fracture is suspected, ultrasonography is highly recommended as the diagnostic method of choice. Treatment is generally conservative and the prognosis is usually favorable.
This case highlights the importance of accurate and early diagnosis of such injuries in newborns following birth trauma. Early recognition allowed this patient to be managed conservatively, successfully preventing serious sequelae to date.
Authorship
Sara Rodrigues - Methodology; Investigation; Writing - original draft
Diana Reis Monteiro - Investigation; Writing - original draft
Rosário M. Cunha - Investigation; Writing - original draft
Inês Casais - Writing - review & editing
Sandra Silva - Supervision; Writing - review & editing
Mafalda Santos - Supervision; Validation; Writing - review & editing