Introduction
Teratomas are tumors composed of tissue derived from all three embryonic germ layers: ectoderm, mesoderm, and endoderm.1-3 Based on histologic analysis, they are classified as mature or immature, with the latter accounting for only 1% of cases.1-3 Although rare, with an incidence of 1:20,000 - 1:40,000 live births, teratomas are the most common congenital neoplasms.1-3 These tumors typically occur along the midline of the body, with the sacrococcygeal region being the most frequent site (40%).1,2 Mediastinal teratomas are much less common, accounting for only 2.6-4% of cases.1-4 The diagnosis is most often made during the second or third trimester of pregnancy by ultrasound (US), which typically shows a heterogeneous mass with mixed cystic and solid components, including hyperechoic foci with acoustic shadowing corresponding to areas of calcification within the lesion.3-6 Fetal magnetic resonance imaging (MRI) provides additional anatomic detail, allowing to characterize the internal contents of the mass and delineate its borders.3-5
Mediastinal teratomas can have significant clinical implications, including compression of intrathoracic organs, which can result in nonimmune fetal hydrops (NIFH), heart failure, pulmonary hypoplasia, and polyhydramnios.5-8
Several case reports in the literature describe fetal mediastinal teratomas, with different management strategies depending on factors such as gestational age, tumor size and growth rate, and the presence of NIFH. During pregnancy, interventional options include amnioreduction in cases of significant polyhydramnios, aspiration of the cystic components of the tumor, or in utero surgical resection.4),(7),(9 Some authors recommend in utero resection if fetal hydrops develops before 30 weeks of gestation.3),(9 At delivery, ex utero intrapartum therapy (EXIT) may be used to ensure ventilation if airway compression is strongly suspected.3),(5),(9),(10
This report described a case of mediastinal teratoma first diagnosed in the second trimester of pregnancy, highlighting the imaging features of the tumor and the chosen surveillance and treatment plan.
Clinical case
A 35-year-old primigravida with no relevant pathologic or genetic history was referred to the Center for Fetal Medicine and Surgery at 23 weeks’ gestation for evaluation of a fetal thoracic mass. Initial evaluation revealed a cystic lesion in the thymic region measuring 25 x 17 mm, and amniocentesis was performed.
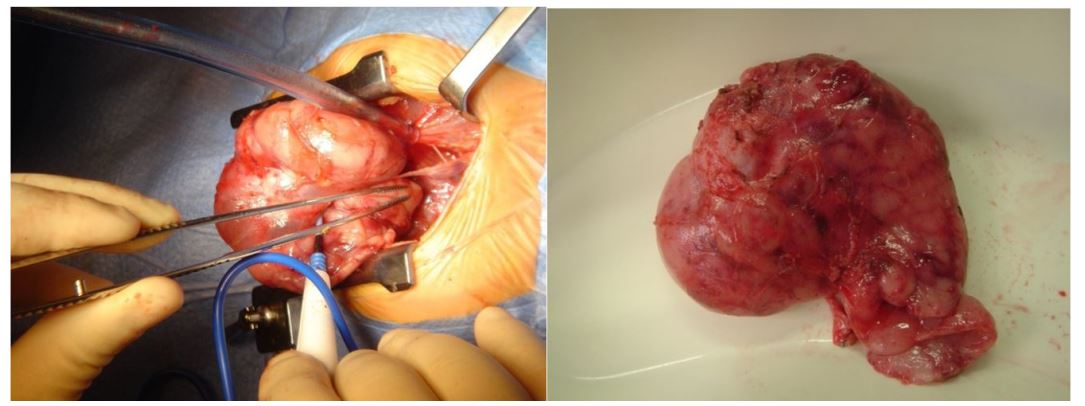
At 25 weeks, a detailed US revealed a heterogeneous mass in the anterior mediastinum measuring 30.2 x 24.6 x 28 mm with cystic and solid components and poor vascularization (Figure 1). Although the mass caused displacement of the mediastinum, there was no evidence of hemodynamic compromise. These findings were consistent with a diagnosis of mediastinal teratoma. Fetal biometry and other anatomic assessments were within normal limits.
Genetic analysis of the amniotic fluid revealed a duplication in the 22q11.21 region that, to the best of the authors’ knowledge, was unrelated to the malformation identified. After genetic counseling and a detailed discussion of the risks, the couple decided to continue the pregnancy.
Management decisions in this case were made by a multidisciplinary team composed of obstetricians specializing in fetal diagnosis and therapy, neonatologists, pediatric cardiologists and surgeons, radiologists, and geneticists. A monitoring plan was established with biweekly US scans.
Fetal MRI at 29 weeks confirmed the suspected diagnosis of teratoma (Figure 2). Mild pleural effusion and ascites were noted, consistent with early signs of fetal hydrops.
At the 31-week US, the lesion had increased in size to 59 x 40 x 36 mm and showed cystic, solid, and calcified components. Mild pleural effusion persisted, and additional findings included subcutaneous edema and polyhydramnios (Figure 3). Cervical examination revealed a shortened cervix measuring 19 mm.
Given these findings, the patient was admitted for close monitoring and received antenatal corticosteroid therapy to promote fetal lung maturation (two doses of 12 mg betamethasone administered 24 hours apart). After stabilization, she was discharged five days later for continued outpatient monitoring.
At 33 weeks’ gestation, the lesion remained stable in size and signs of fetal hydrops resolved, with no evidence of effusion or polyhydramnios. Doppler parameters were normal. Fetal echocardiography showed no structural or functional abnormalities.
No additional findings were noted on fetal scans from 33 to 39 weeks. At 39 weeks, the patient experienced spontaneous rupture of membranes and a female infant weighing 2535 g was born by vacuum-assisted vaginal delivery. Apgar scores were nine at five minutes and 10 at 10 minutes, with no signs of respiratory distress.
On day 7, a computed tomography (CT) scan of the chest showed a well-defined tumor measuring 60 x 54 x 32 mm, heterogeneous and with areas of calcification (Figure 4). It was closely associated with the mediastinal vessels and caused a mass effect in the thorax, although no pleural effusion was observed.
At one month of age, the infant underwent elective surgery. The mediastinal mass was completely removed via midline sternotomy without intraoperative or immediate postoperative complications (Figure 5A).
Histopathologic examination revealed a 60 x 42 x 18 mm tumor (Figure 5B), 90% cystic, containing elements from all three germ layers: endoderm (respiratory epithelium, seromucous glands, and pancreatic tissue), ectoderm (neuroglial tissue), and mesoderm (adipose tissue and cartilage). The final diagnosis was mature mediastinal teratoma (adult type).
At the sixth-month follow-up, the infant was in good health, with no evidence of tumor recurrence or delayed postoperative complications.
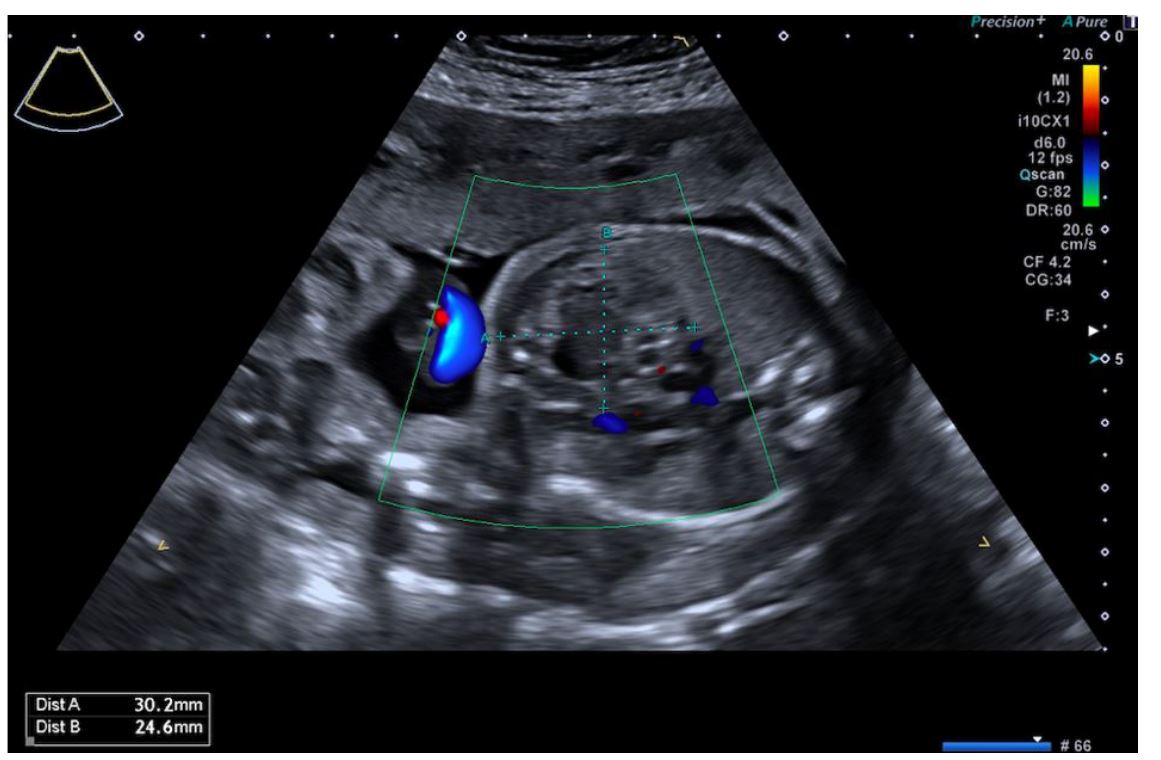
Figure 1 Ultrasound at 25 weeks showing a heterogeneous mass located anteriorly and in the midline of the thorax measuring 30.2 × 24.6 × 28 mm with cystic and solid components and poor vascularization.
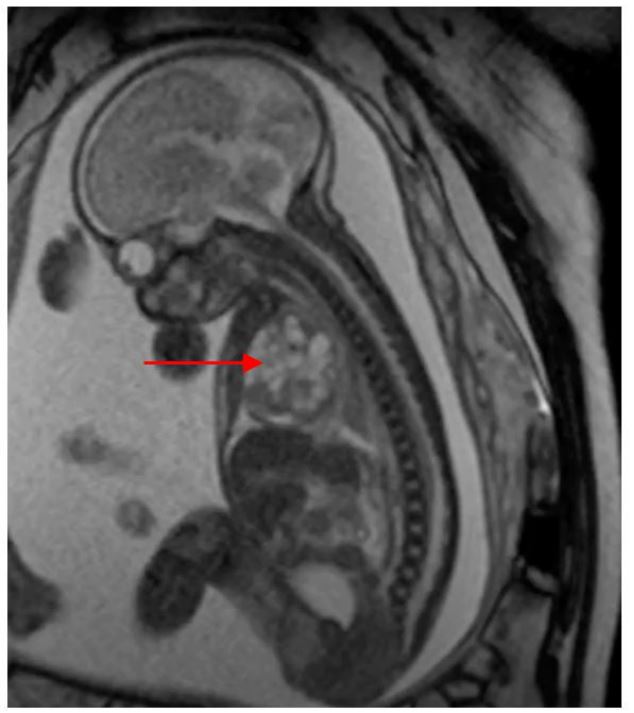
Figure 2 MRI at 29 weeks showing a predominantly cystic mass in the right hemithorax. The red arrow indicates the mediastinal teratoma.
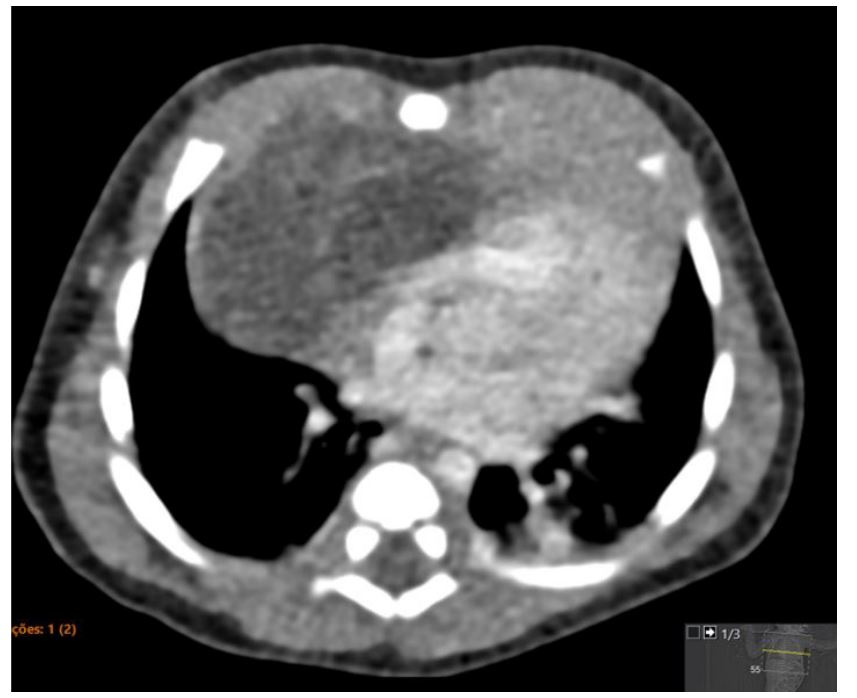
Figure 3 Ultrasound at 31 weeks showing a heterogeneous thoracic lesion with associated pleural effusion.

Figure 4 Postnatal CT scan showing a hypodense cystic mass with thin septa with contrast enhancement.
Discussion/conclusions
Advances in prenatal US, complemented by MRI, allow detailed characterization of many thoracic lesions in utero. Teratomas are among the most common congenital tumors, with prognosis depending on factors such as size, location, and development of NIFH. The differential diagnosis can be challenging and includes congenital cystic adenomatoid malformation, pulmonary sequestration, diaphragmatic hernia, and thymic cysts.2),(3 Certain sonographic features are characteristic of teratomas, including heterogeneous composition with cystic and solid components and hyperechoic foci with acoustic shadowing. Mediastinal teratomas are typically located between the sternum and the heart, which distinguishes them from most lung masses, which are usually seen lateral to the heart.11
Complications may arise from the compressive effect of the tumor on vital structures, potentially leading to NIFH and polyhydramnios in the prenatal period. These complications can cause varying degrees of lung and heart hypoplasia, which can significantly affect postnatal outcomes.7),(8),(11),(12
Airway compression should be carefully assessed to predict potential respiratory distress and ventilatory difficulties at birth.
Several prenatal and perinatal interventional strategies have been described in the literature, including in utero resection, cystic fluid aspiration, and the EXIT procedure.
In this case, an expectant management strategy including serial US scans, echocardiography, and fetal MRI was adopted. This approach was implemented through close collaboration among experts in fetal diagnosis and therapy, pediatric surgeons and cardiologists, geneticists, and radiologists. At 29 weeks’ gestation, the fetus presented with hydrops characterized by mild to moderate pleural effusion, subcutaneous edema, and polyhydramnios. Two weeks later, at 32 weeks’ gestation, the pleural effusion had resolved, subcutaneous edema was no longer observed, and amniotic fluid levels had normalized.
It is hypothesized that the improvement in fetal condition may have been influenced by the administration of corticosteroids for lung maturation. The use of corticosteroids has been associated with resolution or improvement of hydrops and a reduction in mortality in cases of congenital pulmonary airway malformations.14 Another possible explanation for the resolution of NIFH is arrest of teratoma growth.
The literature search conducted identified six case reports of fetuses with mediastinal teratomas who developed NIFH and survived.5),(7-10) In this case, no evidence of cardiac compression or airway obstruction was seen on serial examinations, supporting the continuation of expectant management.
A conservative approach combined with close multidisciplinary surveillance allowed this pregnancy to reach full term without complications.
In conclusion, prenatal diagnosis and close monitoring of mediastinal teratomas are essential for appropriate counseling and individualized treatment plans. Management strategies should be tailored on a case-by-case basis, guided by the couple's decision to continue the pregnancy, and may range from expectant management to interventions such as amnioreduction, in utero resection, aspiration of cystic components of the tumor, EXIT, or postnatal tumor resection. Whenever feasible, perinatal care should be provided by an experienced multidisciplinary team in centers with advanced neonatal and pediatric surgical expertise, as this is critical to a successful outcome.
Authorship
Carolina Carvalho - Writing - original draft; Conceptualization; Investigation; Resources; Visualization
Leonor Ferreira - Writing - review & editing; Resources
Paula Caetano - Writing - review & editing; Resources
Rita Cabrita Carneiro - Writing - review & editing; Resources
Rui Alves - Writing - review & editing; Resources
Ana Bernardo - Writing - review & editing; Conceptualization; Resources; Investigation; Visualization; Supervision
Álvaro Cohen - Writing - review & editing; Resources; Supervision