Introduction
Breastfeeding is unequivocally the best nourishment for the newborn, presenting multiple advantages for the health of both the child and the mother. The benefits of breast milk for the infant are often the primary motivation for the practice of breastfeeding, thus it is of utmost importance to acquire and share knowledge about these benefits. It is expected that increased literacy will reflect in greater adherence to breastfeeding. Breast milk is a complete and natural food, whose nutritional, anti-infectious, cognitive, and immunological advantages stem from its unique composition. Its constituents confer significant anti-infectious properties, aiding in the prevention of acute otitis media, bronchiolitis, acute gastroenteritis, respiratory infections and urinary tract infections, and play a key role in neurodevelopment and consequently in cognitive ability.1-3 The lactose and oligosaccharides present in breast milk are of great importance as prebiotic agents, promoting the growth of beneficial intestinal flora, including bacteria of the genera Bifidobacterium and Bacteroides.4 The reduced colonization by these agents in infants has been associated with increased prevalence of metabolic disorders, such as diabetes mellitus and obesity, and atopic skin diseases, such as dermatitis and eczema, hence the proliferation of these intestinal flora microorganisms through breastfeeding is advantageous for the prevention of these pathologies.5,6
In addition to the benefits for the baby's health, the mother also benefits from the breastfeeding process, with immediate results after delivery, including a reduced risk of postpartum hemorrhage and more rapid uterine involution induced by oxytocin, which is promoted by breastfeeding.7 Not only adherence, but also breastfeeding duration appears to correlate with maternal health benefits.8 In the postpartum period, breastfeeding has been shown to aid in the loss of weight gained during pregnancy.9 Furthermore, in the long term, mothers who breastfeed have a lower risk of developing breast and ovarian cancer, diabetes mellitus, and hypertension.10-11 In summary, greater adherence to breastfeeding and longer duration of breastfeeding have very positive consequences for maternal and child health, and its promotion is one of the objectives of various institutional and community actions in the health sector.
It is estimated that in Portugal the success of this good practice has been improving, thanks to the impact of various initiatives and awareness campaigns promoting breastfeeding, which are in line with those of the Organization for Economic Co-operation and Development (OECD).12 A study comparing the results of the National Health Surveys from 1995/1996 to 2014, revealed that the percentage of women residing in mainland Portugal who exclusively breastfed up to three months increased significantly from 34.6% to 60.6%.12 Another study conducted in two hospitals in Lisbon demonstrated that there was a significant improvement of exclusive breastfeeding rates at three months from 1999 to 2019, with an exclusive breastfeeding rate of 58% in 2019 compared to 41% in 1999.13 Both studies did not identify a significant improvement in the prevalence of exclusive breastfeeding up to six months. Thus, despite the efforts made in this area, there is still a long way to go regarding the promotion of breastfeeding in Portugal.
It is known that community interventions aimed at promoting breastfeeding and increasing literacy on this topic can enhance the rates of adherence, exclusivity, and duration of breastfeeding.8 Family Physicians, due to their close and lasting relationship with patients, are in a privileged position to encourage the practice of breastfeeding and its maintenance over time, with the aim of promoting the health of the mother-child dyad.
In order to improve health literacy regarding the importance and process of breastfeeding, and consequently, increasing its practice, the authors conducted a community intervention in a Primary Health Care setting. Its methods and results are further discussed in this article.
Methods
Community Intervention
The authors conducted a training session on breastfeeding, to which all pregnant women registered at USF Rainha D. Amélia, and their partners were invited. During the session, the following topics were covered: benefits of breast milk for the infant, benefits of breast milk for the mother, legal framework, milk extraction techniques, milk storage and preservation, prevention and management of breastfeeding complications.
On the day of the session, informed consent was obtained from the participants and an evaluation questionnaire on the topic of breastfeeding, developed by the authors and written in Portuguese, was implemented (Appendix 1 and 2). The questionnaire was repeated immediately after the training session to assess the participants' knowledge progression, and one month after the presentation to evaluate knowledge retention over time.
With this intervention, the authors aimed to promote the acquisition of knowledge about breastfeeding, targeting all of the following goals:
Achieve at least 75% correct items on the questionnaire after the intervention.
Attain an increase in the number of correct answers in at least 50% of the participants after the intervention.
Achieve an improvement of at least 25% in the participants' knowledge compared to the initial questionnaire.
Obtain a maximum knowledge decline of 25% on the re-evaluation questionnaire administered one month after the intervention.
Additionally, the authors aimed to evaluate the impact of different variables (gender, age, education level, number of children and previous participation in a breastfeeding course) on the baseline knowledge levels of the participants and the evolution of this knowledge after the intervention.
Statistical Analysis
Data analysis was performed using SPSS® version 26.0. Means (M) and standard deviations (SD) were used to describe continuous variables after confirming the symmetry of distributions. Absolute (n) and relative (%) frequencies were used for categorical variables. The comparison of proportions of correct responses before and after the breastfeeding session was conducted using McNemar's paired proportions test. To evaluate the combined effect of the session and other variables of interest on the knowledge progression demonstrated after the session, the sum of correct responses was calculated, creating a total score ranging from 0 to 10 points. Repeated Measures ANOVA was used to assess the overall effect of the session on the total score increase and subsequently the combined effect with variables such as age, sex, education level, number of children and participation in a previous breastfeeding course. Eta squared (η²) was the effect size considered, with cut-off points of 0.01 (small effect), 0.06 (moderate effect), and 0.14 (large effect). The variables age (≤ 30 y.o. vs. > 30 y.o.), education level (higher education vs. no higher education), and number of children (first child vs. > second child) were recoded to facilitate these analyses. Fisher’s exact test was used to assess the association between variables (level of education and prior history of breastfeeding). The assumptions of normality (Shapiro-Wilk test, p > 0.05) and homogeneity of variances (Levene's test, p > 0.05) were evaluated and confirmed. To assess the joint effect of all independent variables studied, as well as the confounding effect of the score obtained before the session, a multiple linear regression was constructed. The effect size was evaluated with the unstandardized coefficients estimated by the least squares method (β). The corresponding 95% confidence interval was also calculated. Model quality was assessed with the F-test and R². In the assessment of linear regression assumptions, the normality of residuals distribution (Shapiro-Wilk test, p > 0.05), absence of residuals exceeding an absolute value of 3 (ri ≤ |3|) and homoscedasticity of variances, evaluated by the standardized residuals vs. predicted values plot, which showed random dispersion, were confirmed. Statistical significance was assessed with a p-value < 0.05.
Results
In this study, 33 participants were included with the majority being female (78.8%, n = 26), aged between 18 and 40 years old (y.o.), with 63.6% (n = 21) above 30 y.o. and a mean age of 31.6 y.o. Of these participants, 63.6% (n = 21) had completed higher education, and only 15.2% (n = 5) had previously attended a breastfeeding course or training.
Regarding the number of children and history of previous breastfeeding, about 42.4% of participants (n = 14) had one or more children and 38.5% of women (n = 10) had breastfed in the past. The remaining descriptive analysis of the sample is represented in Table 1.
In the administration of the first questionnaire prior to the informative session the proportion of correct answers was 67.3%, corresponding to a mean (M) of 6.73 correct questions per questionnaire, with a standard deviation (SD) of 1.74 (Figure 1). Repeated Measures ANOVA showed that the average score on the questionnaire after the session was significantly higher (p < 0.001), with a proportion of correct answers of 91.5% (M = 9.15; SD = 0.83).
According to this analysis, we found that there was an improvement in knowledge for 87.9% of the participants (n = 29), with only two participants (6.1%) registering a decrease in correct answers on the questionnaire after the intervention. The proportions of correct answers before and after the health education session are represented in Table 2. It was noted that there was a positive progression between the questionnaire administered at the beginning and at the end of the session for all questions except for question seven, for which there was an equal amount of incorrect answers before and after the session. Despite this result, this positive progression was only statistically significant for questions four (p < 0.001), five (p = 0.001), six (p = 0.004), and eight (p = 0.001). It is also noteworthy that questions three, four and nine were those with the lowest approval rates on the initial questionnaire.
Table 1 Characterization of the Study Sample
| Variables | n | % |
| Gender | ||
| Women | 26 | 78.8% |
| Men | 7 | 21.2% |
| Age | ||
| ≤ 30 y.o. | 12 | 36.4% |
| > 30 y.o. | 21 | 63.6% |
| Education Level | ||
| Basic (1-9) | 2 | 6.1% |
| Secondary (10-12) | 10 | 30.3% |
| Higher (>12) | 21 | 63.6% |
| Number of children | ||
| One (this is the first child) | 19 | 57.6% |
| Two | 12 | 36.4% |
| Three or more | 2 | 6.1% |
| Previous breastfeeding | ||
| Not applicable (male gender) | 7 | 21.2% |
| No history of breastfeeding - Previously used formula | 2 | 6.1% |
| No history of breastfeeding - First child | 14 | 42.4% |
| Has previously breastfed | 10 | 30.3% |
| Previous breastfeeding course | ||
| No | 28 | 84.8% |
| Yes | 5 | 15.2% |
Disclaimer: Due to rounding, some totals may not correspond with the sum of the separate figures.
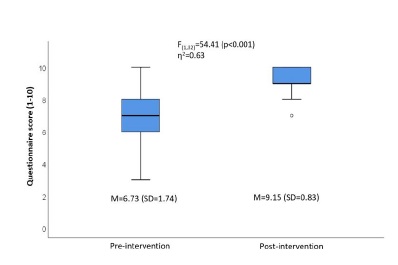
Figure 1 Comparison between pre-intervention and post-intervention questionnaire results, using repeated measures ANOVA
Table 2 Analysis of number and proportion of correct answers, before and after the intervention
| Question | Before the Intervention | After the Intervention | McNemar Test |
| 1 | 27 (81,8%) | 30 (90,9%) | p = 0,453 |
| 2 | 27 (81,8%) | 31 (93,9%) | p = 0,289 |
| 3 | 17 (51,5%) | 22 (66,7%) | p = 0,302 |
| 4 | 6 (18,2%) | 32 (97,0%) | p < 0,001 |
| 5 | 22 (66,7%) | 33 (100,0%) | p = 0,001 |
| 6 | 24 (72,7%) | 33 (100,0%) | p = 0,004 |
| 7 | 32 (97,0%) | 32 (97,0%) | p > 0,990 |
| 8 | 20 (60,6%) | 31 (93,9%) | p = 0,001 |
| 9 | 17 (51,5%) | 25 (75,8%) | p = 0,077 |
| 10 | 30 (90,9%) | 33 (100,0%) | p = 0,250 |
Additionally, an analysis was conducted regarding the interaction effect of the studied variables (age, gender, education level, number of children and previous participation in a breastfeeding course) on the participants’ baseline knowledge in the pre-intervention questionnaire and on the progression of their knowledge after the training session.
Concerning the participants’ baseline knowledge, i.e., knowledge prior to the intervention, it was found that the education level was the only statistically significant predictor of higher knowledge in the pre-intervention questionnaire (p = 0.023). This analysis indicates that participants who had completed higher education obtained a greater number of correct answers on the pre-intervention questionnaire.
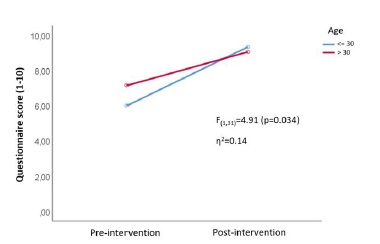
Regarding the effect of each of the studied variables on the progression of participants’ knowledge, it was found that gender, number of children and previous participation in a breastfeeding course did not show a statistically significant impact on knowledge progression. However, there was a significant interaction with age (p = 0.034) and education level (p = 0.034). Participants under 30 years of age had lower initial knowledge (M = 6.00; SD = 1.86) but achieved higher scores after the session (M = 9.33; SD = 0.78). Participants without higher education obtained lower initial scores (M = 5.83; SD = 1.85), but after the training, the scores were similar regardless of education level. These interactions can be visualized in Figures 2 and 3.
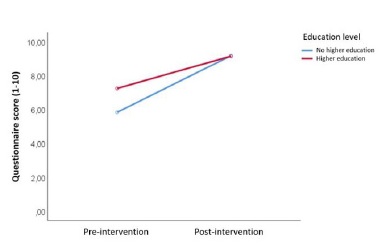
Figure 3 Effect of education level on the progression of total score before and after the intervention
To test the combined effect of different variables on the score variance obtained between questionnaires, a linear model was implemented, adjusted for the confounding effect of the pre-session score. The variable of previous participation in a breastfeeding course was the only statistically significant predictor, suggesting that these participants, on average, answered one more question correctly (β = 1.02; p = 0.023) than participants who had not attended any breastfeeding course, as shown in Table 3.
Table 3 Joint effect on score progression between questionnaires, adjusted for confounding factors (linear regression)
| Variable | β | SE | valor p | IC 95% |
| Score prior to the intervention | -1,00 | 0,09 | p < 0,001 | -1,19; -0,81 |
| Age > 30 y.o. | -0,10 | 0,33 | p = 0,761 | -0,79; 0,58 |
| Male gender | 0,15 | 0,35 | p = 0,675 | -0,58; 0,88 |
| Higher education | -0,27 | 0,33 | p = 0,427 | -0,96; 0,42 |
| One or more children | -0,56 | 0,31 | p = 0,082 | -1,20; 0,08 |
| History of breastfeeding course | 1,02 | 0,42 | p = 0,023 | 0,15; 1,88 |
Finally, the analysis of the proportion of correct answers in the same questionnaire administered one month after the intervention revealed a significant follow-up loss (of the initial 33 participants, responses were obtained from only 15 individuals). An approval rate of 87.3% was obtained. When compared to the approval rate of the questionnaire administered immediately after the intervention, there was a decrease of 4.2 percentage points between the two time points, corresponding to a knowledge decline of approximately 4.6%.
Discussion
This community intervention, aimed at increasing participants' literacy regarding breastfeeding, proved to be effective, considering the targets established by the authors. In the pre-intervention questionnaire, a correct response rate of 67.3% was observed, and in the post-intervention questionnaire this value increased to 91.5%, exceeding the target of 75% correct answers in the pre-intervention questionnaire set by the authors. These data allow us to infer that there was an increase of 24.2 percentage points between the questionnaires, which corresponds to a 36% improvement in knowledge compared to the initial knowledge, surpassing the intended target.
Regarding the participants' progression between the questionnaires administered before and after the session, 87.9% of participants improved the number of correct answers. This value exceeds the researchers' objective of achieving a knowledge progression in at least 50% of the participants.
Additionally, the intervention resulted in only a 4.6% knowledge decline approximately one month after the intervention, which is well below the threshold established by the authors. However, this data analysis should consider the significant follow-up loss observed at this project phase.
Concerning the individualized analysis of the questions, the results showed that the question with the most significant progression, question four, had the lowest approval rate in the initial questionnaire (18.2%). However, after the training session, the approval rate for this question was 97%, which reflects not only the effectiveness of the training session but also the relevance of addressing the topic of milk storage in breastfeeding consultations and courses.
After analyzing the impact of different variables on participants' knowledge levels, it was found that higher education was statistically significantly associated with greater knowledge prior to the intervention. Regarding the variable of age, it was also documented that younger participants had less knowledge about breastfeeding before the training session, although this difference was not statistically significant (presumably due to the small sample size). This trend aligns with what various authors have documented regarding the impact of the mother's age and education level on her literacy and decision to breastfeed. In a study conducted in India among adolescents and young adults, Kumar et al.14 found that older participants with more than 10 years of schooling had greater knowledge regarding breastfeeding.
Breastfeeding literacy is described as one of the factors positively influencing the decision to breastfeed long-term, as verified by Dyson et al.15 Thus, we can infer that education and age, through their positive influence on acquiring knowledge about breastfeeding, also contribute positively to improving breastfeeding adherence. Multiple researchers have also studied the association between these variables and breastfeeding adherence. Although in this group the authors did not find a statistically significant association between education level and previous breastfeeding practices, other studies have confirmed this connection. A study conducted in Indonesia concluded that mothers' education positively influenced exclusive breastfeeding practices.16 Additionally, in an American study, Jones et al.17 found that mothers over 30 years of age were twice as likely to maintain exclusive breastfeeding for up to six months compared to mothers under 20 years of age.
The authors also found that age and education had a statistically significant impact on participants' knowledge improvement after the intervention. However, they note that after conducting an analysis adjusted for different confounders, the only variable that showed a statistically significant impact on knowledge progression, and thus the only predictor of this evolution, was previous attendance at a breastfeeding course. This apparent inconsistency seems to be explained, besides the small sample size, by the fact that older participants with higher education are more likely to have previously attended one of these courses compared to participants aged 30 or younger without higher education. It is expected that participants who had previously attended a breastfeeding course could recall previously forgotten concepts, making it easier to understand and memorize them after this knowledge update during the training session.
The results of this investigation also support the effectiveness of a community intervention on breastfeeding, conducted by healthcare professionals, in increasing participants' knowledge levels. Similar conclusions have been reported in various systematic reviews, showing a positive impact of community interventions and counseling by healthcare professionals on breastfeeding adherence.18,19
Regarding other factors influencing the decision to initiate breastfeeding, different variables are described in the literature, including the right to breastfeeding leave, the percentage of salary subsidy, the number of weekly working hours, and family support.20 A systematic review conducted by Ogbo et al. concluded that partners' support plays an essential role in the mother's decision to initiate and continue breastfeeding.21 Although there is significant heterogeneity in the type of support provided by partners to pregnant and postpartum women, the positive impact of this support was observed in the initiation and duration of exclusive breastfeeding, particularly when this support consisted of verbal encouragement. Other effective forms of support included assistance in preventing and resolving breastfeeding-related complications, as well as help with household chores and childcare.21 These findings validate the intervention carried out, as the authors included not only pregnant women but also their partners. This decision was based on the premise that increasing knowledge about breastfeeding (specifically in milk extraction and storage techniques, preventive measures and complication resolution strategies) would better equip partners to support women during breastfeeding.
However, the study has several limitations. The small sample size, resulting from the limited number of pregnant women registered at USF Rainha D. Amélia and the potential incompatibility of the session time with work schedules, restricted the analysis capacity and the statistical value of the results.
Regarding sample selection, there may have been participation bias, as individuals who accepted to participate in this intervention may have different characteristics from those who declined, possibly having a greater concern for their health and their baby's health, and potentially overestimating the results obtained after the training session.
Another limitation encountered by the researchers was the absence of a validated questionnaire for the Portuguese population regarding breastfeeding literacy, which could introduce a measurement bias in the results.
Finally, during the administration of the last questionnaire, approximately one month after the intervention, there was a significant follow-up loss of participants, which may render the analyzed results unrepresentative of the original sample. The authors believe that administering the questionnaires remotely (via telephone and email) may have contributed to the reduced participation rate. This could have been improved by conducting an additional support session for addressing queries, with the questionnaires being repeated in person.
Conclusion
In accordance with the literature, this community intervention conducted by qualified healthcare professionals improved the literacy regarding breastfeeding among pregnant women and their partners. Despite a significant loss in follow-up, the knowledge decline one month after the session was slight, demonstrating the importance and impact of such interventions. The longevity of these informative sessions’ impact was also demonstrated by the fact that previous attendance of a breastfeeding course was the only predictor of greater knowledge progression.
This study also provided a valuable opportunity to examine the impact of age, education, parental background and other variables on breastfeeding knowledge, facilitating data collection and encouraging researchers to explore these determinants. However, further studies on this topic are necessary to confirm the impact of these variables on breastfeeding literacy. Moreover, additional research is needed to corroborate the direct relationship between literacy level and adherence, duration and exclusivity of breastfeeding.
Authorship
Sofia Padilha - Conceptualization; Methodology; Investigation; Data curation; Formal analysis; Writing - original draft
Pedro Arantes - Conceptualization; Methodology; Investigation; Data curation; Formal analysis; Writing - original draft
Teresa Sarmento de Beires - Conceptualization; Methodology; Investigation; Data curation; Formal analysis; Writing - original draft
Joana Ribeiro - Conceptualization; Supervision; Writing - review and editing
Andreia Eiras - Conceptualization; Supervision; Writing - review and editing