Imaging Cases
Purpuric rash in an adolescent
Exantema purpúrico num adolescente
1 Department of Pediatrics, Hospital José Joaquim Fernandes, Unidade Local de Saúde do Baixo Alentejo. 7801-849 Beja, Portugal. joanalebre@gmail.com; ana.margalha.miranda@gmail.com; sonia.garces@ulsba.min-saude.pt
Abstract
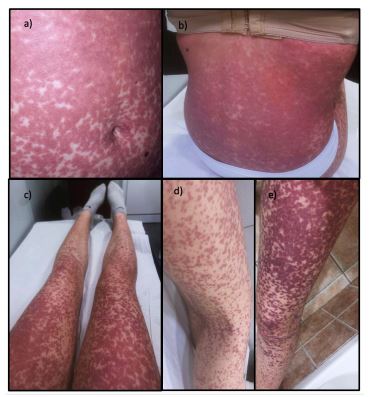
A previously healthy 17-year-old girl presented to the emergency department with a 14-day history of fever, sore throat, and a generalized reddish-purple pruritic rash. The rash, initially erythematous and maculopapular, worsened and became coalescent and purpuric. She had been treated with azithromycin for three days starting on the third day of illness. Physical examination revealed a good general condition, pharyngeal erythema with exudate, and a purpuric rash covering the body, including the face, palms, and soles, without other systemic signs. Serological tests confirmed a diagnosis of acute infectious mononucleosis. The patient was managed conservatively and had fully recovery at re-evaluation, 50 days after symptom onset. Acute infectious mononucleosis typically presents with fever, cervical lymphadenopathy, and tonsillitis/pharyngitis, with spontaneous exanthema occurring in 3-15% of cases. This case highlights the importance of considering acute infectious mononucleosis in adolescents presenting with purpuric exanthema and the potential for antibiotic-associated rash including azithromycin, emphasizing the need for thorough clinical and serological evaluation.
Keywords: azithromycin; infectious mononucleosis; purpuric rash
Resumo
Uma adolescente de 17 anos, previamente saudável, apresentou-se no serviço de urgência com uma história de 14 dias de febre, odinofagia e erupção cutânea pruriginosa generalizada de cor púrpura-avermelhada. A erupção cutânea, inicialmente eritematosa e maculopapular, agravou-se e tornou-se coalescente e purpúrica. A doente foi medicada com azitromicina durante três dias a partir do terceiro dia de doença. O exame físico revelou um bom estado geral, eritema faríngeo com exsudado e um exantema purpúrico generalizado, incluindo a face, as palmas das mãos e as plantas dos pés, sem outros sinais sistémicos. Os testes serológicos confirmaram o diagnóstico de mononucleose infecciosa aguda. A doente recebeu terapêutica de suporte e recuperou totalmente 50 dias após o início dos sintomas. A mononucleose infecciosa aguda é tipicamente caracterizada por febre, linfadenopatia cervical e amigdalite/faringite, com exantema espontâneo a ocorrer em 3-15% dos casos. Este caso realça a importância de considerar a mononucleose infecciosa aguda em adolescentes com exantema purpúrico e o potencial de exantema associado a antibióticos, incluindo a azitromicina, sublinhando a necessidade de uma avaliação clínica e serológica exaustivas.
Palavras-chave: azitromicina; exantema purpúrico; mononucleose infecciosa
A 17-year-old girl, previously healthy, presented to the emergency department with a generalized reddish-purple pruritic rash. She gave a history of fever, sore throat and malaise starting 14 days before. She was medicated on the third day of disease with azithromycin for three days. Three days after completing treatment, she developed a rash initially erythematous and maculopapular, widespread all over the body. Over the next days, the lesions became coalescent and purpuric. Fever resolved on the 11th day of the illness. Physical examination showed good general condition, pharyngeal erythema and exudate, and a scattered purpuric exanthema over the entire body, including face, palms and soles (Figure 1), without any other complaints such as mucous-membrane involvement, arthralgias, hepatomegaly, facial or peripheral oedema.
What is your diagnosis?
Diagnosis
Acute infectious mononucleosis (AIM) with a purpuric exanthema associated with azithromycin intake, based on seroconversion of Epstein-Barr virus-specific IgM and IgG antibodies (on the 14th day of illness, the patient had: positive EBV VCA IgM, positive EBV VCA IgG, negative EBV EBNA IgG; at 50 days after symptom onset: negative EBV VCA IgM, positive EBV VCA IgG, positive EBV EBNA IgG).
Patient’s management
The patient was treated with supportive care and recovered from all symptoms 50 days after the onset of disease, with no visible skin lesions.
Discussion
AIM is an acute clinical manifestation of EBV infection, and typically presents with a triad of fever, cervical lymphadenopathy, and tonsillitis/pharyngitis.1 A spontaneous exanthema can occur in 3-15% of the affected patients.2 The characteristic exanthema is maculopapular (in some patients, an urticarial or petechial rash may also be seen), involving mainly the trunk and sparing the extremities.2
In patients with AIM, a rash has been described following the administration of ampicillin or amoxicillin in up to 33% of cases, and lately, it has also been described occasionally with other antibiotics, such as azithromycin.3,4 The mechanism responsible for this rash is not well understood, but it may represent a transient virus-mediated immunomodulation, resulting in the development of a reversible, delayed-type hypersensitivity reaction to the antibiotic.4,5
The characteristics of AIM in children that will develop an antibiotic-associated rash are not known, but an older age may be an independent risk factor.6
Authorship
Joana Melo - Writing - original draft; Writing - review & editing
Ana Margalha Miranda - Writing - original draft; Writing - review & editing
Sónia Pereira Fernandes Garcês - Writing - original draft; Writing - review & editing
References
1. Luzuriaga K, Sullivan JL. Infectious mononucleosis. N Engl J Med. 2010;362:1993.
[ Links ]
2. Chovel-Sella A, Ben Tov A, Lahav E, Mor O, Rudich H, Paret G, Reif S. Incidence of rash after amoxicillin treatment in children with infectious mononucleosis. Pediatrics. 2013 May;131(5):e1424-7. doi: https://doi.org/10.1542/peds.2012-1575.
[ Links ]
3. Thompson DF, Ramos CL. Antibiotic-Induced Rash in Patients With Infectious Mononucleosis. Ann Pharmacother 2017; 51:154.
[ Links ]
4. Banerjee I, Mondal S, Sen S, Tripathi SK, Banerjee G. Azithromycin-induced rash in a patient of infectious mononucleosis - a case report with review of literature. J Clin Diagn Res. 2014 Aug;8(8):HD01-2. doi: https://doi.org/10.7860/JCDR/2014/9865.4729.
[ Links ]
5. Di Lernia V, Mansouri Y. Epstein-Barr virus and skin manifestations in childhood. Int J Dermatol. 2013;52(10):1177-84.
[ Links ]
6. Zhang R, Mao Z, Xu C, Wang W, Kwong JS, Xu M, et al. Association between Antibiotic Exposure and the Risk of Rash in Children with Infectious Mononucleosis: a Multicenter, Retrospective Cohort Study. Antimicrob Agents Chemother. 2023 Jun 15;67(6):e0024923. doi: https://doi.org/10.1128/aac.00249-23.
[ Links ]