Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Medicina Interna
versão impressa ISSN 0872-671X
Medicina Interna vol.24 no.2 Lisboa jun. 2017
ARTIGOS ORIGINAIS / ORIGINAL ARTICLES
Predictores de Prescrição Inadequada de Inibidores da Bomba de Protões num Serviço de Medicina Interna
Predictors of Inappropriate Proton Pump Inhibitor Prescription in an Internal Medicine Department
Luís Ramos dos Santos, Sofia Nóbrega, Dina Santos, Manuela Lélis, Maria da Luz Brazão
1Serviço de Medicina Interna, Hospital Central do Funchal,
SESARAM EPE, Funchal Portugal
RESUMO
Introdução:Os inibidores da bomba de protões (IBPs) são utilizados no tratamento da patologia gastrointestinal e prevenção da hemorragia digestiva alta, frequentemente de forma inadequada nos doentes hospitalizados.
Métodos:Realizou-se um estudo transversal entre 15 de Março e 15 de Maio de 2015 para avaliar o padrão de prescrição de IBPs num Serviço de Medicina Interna, relativamente às indicações e aos custos.
Resultados: Foram incluídas 585 admissões, idade média de 75 anos. Dos casos, 163 já eram medicados com IBP pré-admissão, metade sem indicação. Dos episódios, 372 receberam um IBP na admissão/durante o internamento, mas apenas 63 casos tinham indicação para tal, pelo que 83% tinham sido medicados de forma inapropriada. Os predictores de prescrição inadequada de IBP foram o sexo feminino, idade = 75 anos e estar medicado com IBP pré-admissão.
Conclusões: Custos totais, directamente relacionados aos IBPs, ascenderam aos 1079,96, em média 2,72 por episódio. A terapêutica com IBPs deve ser revista para reduzir prescrições inadequadas e custos.
Palavras-chave:Departamentos Hospitalares; Inibidores da Bomba de Protões/uso terapêutico; Medicina Interna; Prescrição Inapropriada.
ABSTRACT
Introduction:Proton pump inhibitors (PPIs) are used in the treatment of gastrointestinal pathology and prevention of upper gastrointestinal bleeding. They are frequently misused in hospitalized patients.
Methods:We conducted an observational cross-sectional study between 15th March and 15th May 2015 to evaluate the prescription pattern of PPIs in an Internal Medicine ward regarding indications and costs.
Results:Five hundred and eighty five admissions were included with an average age of 75 years. One hundred and sixty three cases were medicated with a PPI prior to admission, half of them without indication. Three hundred seventy-two cases were prescribed a PPI on admission/during hospital stay but only 63 cases had a proper indication meaning that 83% were inadequately medicated. Predictors of inadequate PPI prescription were female sex, age = 75 years and being medicated with a PPI prior to admission.
Conclusion: Total costs, directly related to PPIs were set at 1079.96, on average 2.72 per episode. Therapy with PPIs should be reviewed to decrease inadequate prescriptions and costs.
Keywords:Hospital Departments; Inappropriate Prescribing; Internal Medicine; Proton Pump Inhibitors/therapeutic uso.
Introduction
Proton pump inhibitors (PPIs) are widely used for several primary gastrointestinal disorders (dyspepsia, gastroesophageal reflux disease (GERD), peptic ulcer disease, Helicobacter pylori eradication, others)1-6as well as in prevention of upper gastrointestinal bleeding (UGIB) such as in the context of antiplatelet therapy or non-steroidal anti-inflammatory drugs (NSAID) therapy.7-10 Its widespread use reflects PPIs overall efficacy and safety. However, some of the risks linked to PPI use include higher rates of enteric infections including Clostridium difficile, community-acquired pneumonia, hip fractures, drug interactions (clopidogre, although inconsistent through PPIs) and several nutritional deficiencies.11-15 Large scale unmonitored use of PPIs may enhance these iatrogenic risks.
Internal Medicine (IM) patients are some of the most prone to receiving a PPI prescription, either from their general practitioners, when hospitalized in IM wards or at the time of hospital discharge.12-19Appropriate prescription of PPI on hospital admission is generally limited to patients with UGIB, peptic ulcer or erosive esophagitis and in a subset of Intensive Care Unit (ICU) patients.1 It is then arguable that many patients admitted to IM wards are inappropriately prescribed a PPI, leading to iatrogenic and economic consequences.1,20,21 PPI prescription itself is not the only problem as a reasonable number of patients are inappropriately prescribed intravenous forms, usually reserved for active UGIB.22-24
The purpose of this research was to evaluate prescription patterns of PPIs in an Internal Medicine department regarding its indications, predictors of misuse and briefly describe the costs involved.
METHODS
An observational cross-sectional study was conducted from 15th March 2015 to 15th May 2015 in the Internal Medicine (IM) department at Hospital Central do Funchal, SESARAM EPE, Funchal, Portugal, a tertiary hospital with 134 IM beds. Consecutive admissions to the general ward and intermediate care unit were enrolled. Exclusion only happened when there was discrepancy between patient file number and patient name. Demographic data was obtained (sex, age). Motive of admission was noted and categorized in six groups according to higher prevalence in the sample (lower respiratory tract infections (LRTIs), urinary tract infections (UTIs), heart failure (HF), ischemic stroke (IS), cerebral hemorrhage (CH) and others) as seen on Table 1. Relevant ambulatory medications were also enquired (antiplatelet therapy, anticoagulants, NSAID, corticosteroids). Daily therapeutic online sheets were consulted for prescription data extraction (date of initiation, date of suspension, administration route, date of change of administration route, and type of PPI). For information regarding the use of PPI prior to admission and the motive for such use, each patient file was reviewed in search of diagnosed entities and endoscopic data in the year prior to ward admission. We considered a positive history if the PPI was prescribed within the last year before admission date. Data regarding ambulatory prescription at time of discharge were obtained from discharge note and reason for prescription was evaluated. If a patient was admitted more than once during the research period they were enrolled as a separate episode. Our aim was to assess physician prescription behavior with each new episode. Moreover, patient distribution per attending physician on admission is random, hence a readmission could be delivered to a different physician, yielding a different prescription outcome. Department director was informed of study but not the remaining physicians in order to assess PPI prescription knowledge at baseline. A follow-up study after presentation of results and literature review is scheduled to assess intervention impact.
Valid criteria for preventive PPI usage in inpatient setting and at discharge time are guidelines updated at time of this study, which are described elsewhere.1-10 Main outcome was appropriateness of PPI usage among IM inpatients according to current evidence. Some considerations should be taken into account regarding criteria used: Intravenous (IV) PPIs are not indicated for UGIB prophylaxis. In all cases, oral or enteric formulas should be used. IV formulas are reserved for peptic ulcer disease in the context of endoscopic procedures or after an endoscopic procedure that confirms a bleeding ulcer or a non-varicose lesion with a high risk for bleeding recurrence.18 In the case of GERD, PPIs are only recommended for: recurring or severe symptomatic GERD as maintenance therapy or induction and maintenance therapy of erosive esophagitis and finally for maintenance therapy for Barretts esophagus. Duration of therapy should be individualized in all cases.17 In the case of peptic disease, PPIs are recommend for induction and maintenance therapy for high risk gastric ulcers (hemorrhage, perforation, refractory, recurrent, giant and fibrotic) as well as duodenal ulcers.17 In this study, chronic corticosteroid therapy refers to a therapy duration superior to three weeks.10
Finally, a simple economic analysis was performed in order to obtain the total amount spent on inappropriate use. Medical records were reviewed by authors (LRS and SN). The study was conducted in adherence with the Declaration of Helsinki and approved by the institutions Ethical Committee. Statistical analysis was performed using SPSS software, version 19. Descriptive analysis was initially performed. Chisquare and Fischers exact test were used for analysis of categorical variables while continuous variables were evaluated using students t-test. Logistic regression was conducted with statistically significant variables from univariate analysis as well as some non-significant but considered relevant for the study; odds ratio (OR) and respective 95% confidence intervals (CI) were calculated. Significance was defined as p < 0.05.
Results
Five hundred and eighty five admissions were entered during the research time. Fig 1 clarifies the process of final sample studied. Three hundred seventy-two admissions were female patients (59.5%). Patient mean age was 75 years (SD 14.62) with a range between 18-100 years. Top three admission motives were LRTIs, UTIs and HF with 45.8, 12.0 and 10.9%, respectively. 54.6 % of patients had at least 4 or more comorbidities on admission with this value rising to 59.5% at discharge. Table 1 summarizes patient demographics.
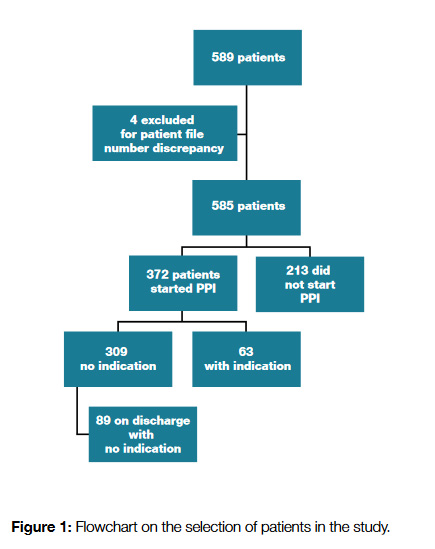
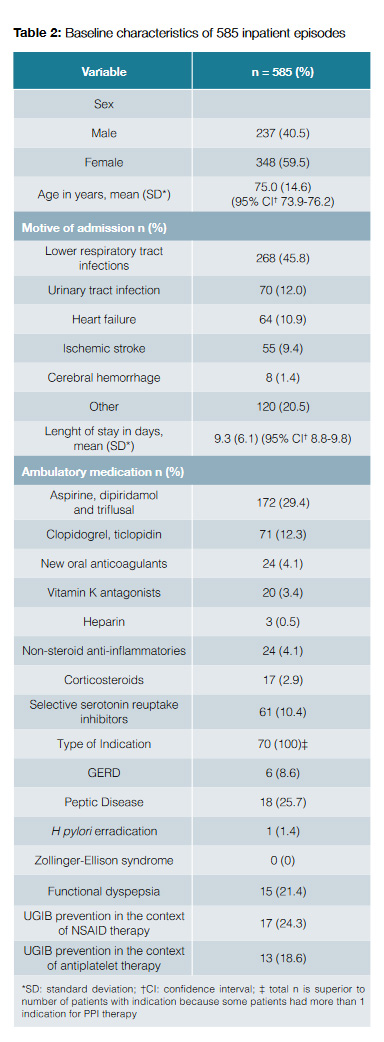
Five hundred fifty nine (95.6%) of patients were admitted to the general IM ward while 26 (4.4%) received treatment in the intermediate care unit. One hundred and sixty-three (27.9%) cases were medicated with a PPI before admission, however, based on the criteria elaborated for this study, only 78 patients (13.3%) had a proper motive for PPI use before admission. Of note, in 372 (63.6%) episodes, patients were prescribed a PPI on admission or during inpatient stay. When reviewing medical record and daily therapeutic sheets just 63 cases had a proper indication for inpatient PPI prescription (each patient could have more than 1 indication) which means that 309 episodes (83.1%) were inappropriately medicated.
Table 1 shows univariate analysis for PPI prescription on admission, comparing patients who did not receive a PPI versus patients who received an inadequate prescription (n = 522). Female sex, increasing age group and prior PPI use showed statistically significant differences in this study, highlighting these variables as factors for inadequate prescription.
Route administration was also evaluated. Two hundred and twenty five (38.5%) cases were given IV pantoprazole at a 40 mg dose, of which 221 (98.2%) without a proper indication, while 148 (25.3%) were prescribed oral esomeprazole at a 40 mg dose, 121 (82.3%) of which without indication. There was a total of 6 UGIB (1%), each corresponding to a different patient with different admission diagnosis. Just one of those patients had a medical record compatible with UGIB prevention (peptic disease), however this patient was not under PPI before admission. Mean inpatient time was 9.3 days (SD 6.01) ranging from 1-69 days.
After multivariate analysis through logistic regression (X2(6)= 47.667, p < 0.00, with the model explaining 11.8% (NagelkerkeR2) of the variance and correctly classifying 64.2% of cases), inappropriate inpatient prescription of PPIs was predicted by female sex (OR: 0.64 95% CI: 0.44-0.94, p = 0.021), age 66-74 years (OR: 1.87 95% CI: 1.03-3.38, p = 0.039), age = 75 (OR: 2.22 95% CI 1.35-3.66,p = 0.002) and use of PPI prior to admission (OR: 3.45 95% CI: 2.07-5.74, p = 0.000) (Table 3).
Of the 309 episodes inadequately prescribed on admission, 89 (29%) received an inappropriate PPI prescription on discharge. Just 70 (23%) cases had a correct indication for taking this medication. Univariate analysis (Table 1), compares patients who did not receive a PPI prescription on discharge versus patients who received and inadequate prescription, regardless of PPI use during inpatient stay (n = 278). Prior PPI use, increasing number of age and comorbidities were statistically associated with PPI prescription for ambulatory care at time of discharge. Due to inpatient treatment or diagnosis, two patients gathered indication for initiating de novo PPI (one after nosocomial UGI bleed, for maintenance therapy, and the other because of the combination of chronic corticosteroid treatment for systemic lupus erythematous, antiplatelet treatment and age above 60 years). On multivariate analysis, through logistic regression (?2(5) = 31.549, p < 0.00, with the model explaining 15.0% (NagelkerkeR2) of the variance and correctly classifying 69.8% of cases) (Table 3) predictors of inappropriate PPI prescription at the time of discharge included patients 75-years-old or older (OR: 5.45 95% CI 1.58- 18.79, p = 0.001), having between 4 and 6 comorbidities (OR: 2.05 95% CI 1.11-3.78, p = 0.022) and between 7-9 comorbidities (OR: 4.87 95% CI 1.73-13.69, p = 0.001). These value are described in Table 3.
Total costs relating solely to inappropriate PPI use ascended to 1079.96, mean per patient during stay of 2.12 (SD 2.97) in the two-month period, roughly 6479.76 for 12 months, see Table 4.
Discussion
Number of inappropriate prescriptions may be highly represented in this patient population because active or subacute UGIBs as well as endoscopic procedures are usually admitted to the Gastroenterology ward not the IM ward. It is likely that prescriptions would be more accurate in the setting of a Gastroenterology ward as previously reported23 both by improved knowledge of proper indications as well as increased volume of endoscopic procedures and UGIB diagnoses that require PPI initiation.
It was surprising to notice the number of IV prescriptions, normally used for active UGIB. In our understanding this may be due to the overall population in the study, which includes patients with decreased oral intake because of old age and comorbidities such as previous stroke. It may be argued that these patients are less autonomous in the handling of their inpatient medication if their motor skills are decreased or if they have dysphagia. However, it is important to note that not infrequently there were other prescriptions (antihypertensive, antidepressants, etc.) by oral intake in the same therapeutic sheets of PPI IV prescriptions, raising the question of true lack of oral intake. These IV PPI prescriptions were naturally deemed inappropriate. The problematic of inappropriate IV PPI prescription has been described before with Craig et al reporting up to 75% of inadequate IV prescriptions, with proper indications for IV PPI being endoscopic evidence of recent UGIB, patient nil by mouth with a valid indication for oral PPI therapy and stress ulcer prophylaxis in a critical care setting.23 Another study found that 71% of IV prescriptions had no clear indication. Correct use was higher among medical ICU physicians (67%), followed by medicine wards (29%) while the surgery wards (16%) had the most incorrect prescriptions rates.15
Several factors were identified as predictors of inappropriate inpatient prescription of a PPI namely female sex, increasing age and use of PPI prior to admission (Table 3). Female sex has been identified as a predictive factor for IV PPI prescription elsewhere.23 In this study we show that it increases the likelihood of oral PPI as well (OR: 0.64 95% CI: 0.44-0.94, p = 0.021). It is unclear to us why there is a trend for more prescriptions in the female sex, although it could be argued that female patients consult more than men and thus have more diagnosed conditions compared to male patients.25
Age was significantly associated with inappropriate prescriptions and the effect was superior with advancing age: age 66-74 years (OR: 1.87 95% CI: 1.03-3.38, p = 0.039), age = 75 (OR:95% CI 1.35-3.66, p = 0.002). Older age is usually linked to other significant comorbidities and polypharmacy. PPI may then be viewed by physicians as a way for gastric protection. We found that the simple fact of being medicated with a PPI prior to admission was independently associated with an inpatient PPI prescription after multivariate analysis (OR: 3.45 95% CI: 2.07-5.74, p= 0.000). Similar results have been described in a study of 213 patients on non-critical inpatient setting, where 84% of the patients admitted were prescribed a PPI despite only 33% of them being medicated prior to admission.26 This raises the question of the depth of knowledge from physicians at the time of making the therapeutic sheets, at least in what PPIs are concerned. While guidelines help establish stress ulcer prophylaxis (SUP) on the ICU setting (ASHP – American Society of Health-System Pharmacists), without promotion of PPIs over other options, there are no guidelines when it comes to the non-critical care setting, except for gastrointestinal diagnosis in need of treatment.1 Despite lack of evidence in this field, several studies have demonstrated overuse of PPIs. Another reason may come from fear of UGIB during inpatient stay.1,27
On the other hand, lack of complete clinical data in the patients files due to poor registration patterns, patient frailty, cognitive impairment or inability to verbalize symptoms or prior diagnosis, may obscure proper reasons for PPI use, thus mislabeling as inappropriate actually appropriate PPI prescriptions. It is still important to emphasize the need to review the indication for each medication prior to its institution during hospital stay and at the time of discharge. Talking to relatives or next of kin may aid in this process as well as raising awareness of physicians to proper registration of diagnosis in the patients files.
We evaluated the financial impact of inappropriate PPI prescriptions. Total costs relating solely to inappropriate PPI use ascended to 1079.96 in the three month period. Mean price per patient per hospital stay was 2.12. These costs are based on pricing per pill of oral esomeprazole or IV pantoprazole ampoule alone. Consumables such as catheters and syringes were not accounted for as well as human resources and possible iatrogenic effects of PPI administration. Thus, there are potential savings to be made with PPI as far as the inpatient setting is concerned. A better description of costs involved can be seen on Table 4.
We also evaluated the pattern of PPI prescription at the time of discharge. A 2006 study with 1769 patients reported a 22% of inappropriate PPI prescription for inpatient SUP with 54% of these patients leaving the hospital under PPI continuation.28 In our study approximately 29% (89 of 309) left the hospital under inappropriate PPI continuation, with just 51 cases (16.5%) of the having appropriate reason for PPI continuation. Predictive factors of inappropriate discharge prescription are age = 75 and increasing number of comorbidities as seen on Table 3. Despite being statistically significant on univariate analysis, we did not include prior to admission PPI use in the multivariate analysis for discharge prescription, for risk of confounding due to inadverted resuming on of routine medication listed before admission. Patient characteristics such as frailty and other polypharmacy in these groups may account for the increased number of prescriptions. Also with increasing comorbidities, it is more likely to exist some sort of past record of GI diagnosis. In these cases physicians may fear risking recurrence of UGIB in the long haul. This may be viewed as lack of proper review of discharge medication namely the need to maintaining certain medications despite appropriate indication. Discharge time should be a privileged time for an ambulatory therapeutic review and overlooking it may have iatrogenic effects as well as an economic impact. In this study we did not propose to evaluate the economic impact of inappropriate ambulatory PPI prescription but some studies have done so elsewhere.26,29,30 A 4-year long study described a rate of 69% of inappropriate discharge PPIs with a related cost during the first 30 days of up to US$3 million.1,26 Another study showed that 24.4% of patients were inadequately discharged with acid suppressant therapy with the total cost for unnecessary therapy within the study period being $13973 (US$4.20 per patient each day).26,29 Another 2010 study conducted in an ambulatory community reported that among 946 patients only 35% had an appropriately documented gastrointestinal reason for PPI prescription, but 10% were prescribed empirically for extraesophageal symptoms, 18% for gastroprotection and in 36% no reason was found for the prescription. Not surprisingly, when all groups were considered, 49% of patients were continued on PPIs without documentation of clinical symptoms reassessment.30
Unfortunately, discharge with an inappropriate PPI prescription will likely be continued for too long. In a retrospective analysis where 34% of patients were inappropriately discharged with acid suppressant therapy (AST) (84% of which with a PPI), 80% and 50% of patients were still under AST at 3 and 6 months, respectively, despite having been evaluated by their primary care physician.31
An information bias could have been introduced in the study since the authors patients were also enrolled. However, after review of the results such bias is residual at best considering the proportion of inappropriate prescriptions, meaning that prior updated knowledge of guidelines from the authors side did not interfere with the results.
In this study we did not evaluate whether or not the implementation of formal guidelines for inpatient prevention of upper gastrointestinal bleeding had any impact on the quality of prescriptions. This has been addressed before by Yachimski et al, where the prescription patterns were evaluated before and after implementation of guidelines for physicians. The introduction of standardized guidelines resulted in an improvement of inpatient and discharge prescriptions.17 After release of this studys results, a follow-up interventional study is schedule to begin to assess impact on prescriptions. In an era where internists have to account for a myriad of polypharmacy it is no wonder that strategies like these improve quality of prescriptions. Such approach could potentially be amplified to other groups of drugs that are misused during inpatient stay.
Conclusion
PPIs remain one of the widest used acid suppressant therapies. This study reinforced that inpatient prescription of PPIs is erratic both in need and in route of administration. Continuous reinforcement of proper indications for its prescription in the hospitalized patient may reduce iatrogenic effects and promote cost savings, a statement due for confirmation in a follow-up interventional study. Clear guidelines for prevention of iatrogenic upper gastrointestinal bleeding in the hospitalized non-ICU patient are still lacking but they may result in a more consensual prescription pattern.
References
1. Heidelbaugh JJ, Kim AH,Chang R, andWalker PC. Overutilization of proton-pump inhibitors: what the clinician needs to know. Therap Adv Gastroenterol.2012; 5: 219-32. [ Links ]
2. Kahrilas PJ, Shaheen NJ, Vaezi MF. American Gastroenterological Association
Institute technical review on the management of gastro-oesophageal reflux disease.Gastroenterology. 2008;135:1392-413. [ Links ]
3. Freston JW. Review article: role of proton pump inhibitors in non-H. Pylori-relatedulcers. Aliment Pharmacol Ther. 2001;15(Suppl 2):2-5. [ Links ]
4. Malfertheiner P, Megraud F, OÂ;Morain C, Bazzoli F, El-Omar E, Graham D,et al. Current concepts in the management of Helicobacter pylori infection: the Maastricht III Consensus Report. Gut. 2007;56:772-81. [ Links ]
5. Wilcox CM, Hirschowitz BI. Treatment strategies for Zollinger-Ellison syndrome.Expert Opin Pharmacother. 2009;10:1145-57. [ Links ]
6.Wang WH, Huang JQ, Zheng GF, Xia HH, Wong WM, Liu XG, et al. Effects of proton-pump inhibitors on functional dyspepsia: a meta-analysis of randomized placebo-controlled trials. Clin Gastroenterol Hepatol. 2007;5:178-85. [ Links ]
7.Abraham NS, Hlatky M, Antman EM, Bhatt DL, Bjorkman DJ, Clark CB, et al. EXPERT CONSENSUS DOCUMENT ACCF / ACG / AHA 2010 Expert Consensus Document on the Concomitant Use of Proton Pump Inhibitors and Thienopyridines: A Focused Update of the ACCF / ACG / AHA 2008 Expert Consensus Document on Reducing the Gastrointestinal Risks. J Am Coll Cardiol. 2010;56:2051–66. [ Links ]
8.Moukarbel GV,Bhatt DL. Antiplatelet therapy and proton pump inhibition: clinician update. Circulation. 2012;125:375-80 [ Links ]
9.Lanza FL, Chan FK, Quigley EM. Guidelines for Prevention of NSAID-related ulcer complications. Am Gastroenterol. 2009;104:728–38. [ Links ]
10.Retornaz F, Boullu-Ciocca S, Farcet A, Oliver C. Arret de la corticotherapie chez la personne agee. Geriatr Psychol Neuropsychiatr Vieil. 2013;11:361-6. [ Links ]
11.Haroon M, Yasin F, Gardezi SK, Adeeb F, Walker F. Inappropriate use of proton pump inhibitors among medical inpatients: a questionnaire-based observational study. JRSM Short Rep. 2013;4:36. [ Links ]
12.Hughes JD, Tanpurekul W, Keen NC, Ee HC. Reducing the cost of proton pump inhibitors by adopting best practice. Qual Prim Care. 2009;17:15–21. [ Links ]
13.Ahrens D, Chenot JF, Behrens G, Grimmsmann T, Kochen MM. Appropriateness of treatment recommendations for PPI in hospital discharge letters. Eur J Clin Pharmacol. 2010; 66:1265–71. [ Links ]
14.Ahrens D, Behrens G, Himmel W, Kochen MM, Chenot JF. Appropriateness of proton pump inhibitor recommendations at hospital discharge and continuation in primary care. Int J Clin Pract. 2012;66:767-73. [ Links ]
15.Eurich, DT, Sadowski, CA, Simpson, SH, Marrie, TJ, Majumdar SR. Recurrent community-acquired pneumonia in patients starting acid-suppressing drugs. Am J Med. 2010; 123:47-53. [ Links ]
16.Oh AL, Tan AG, Phan HS, Lee BC, Jumaat N, Chew SP, et al. Indication of acid suppression therapy and predictors for the prophylactic use of proton pump inhibitors vs. histamine-2 receptor antagonists in a Malaysian tertiary hospital. Pharm Pract. 2015;13:633. [ Links ]
17. Yachimski PS, Farrell EA, Hunt DP, Redi AE. Proton pump inhibitors for prophylaxis of nosocomial upper gastrointestinal tract bleeding. effect of standardized guidelines on prescribing practice. Arch Intern Med.2010;170:779-83. [ Links ]
18.Akram F, Huang Y, Huggan PJ, Merchant RA. Proton pump inhibitors: Are we still prescribing them without valide indicatons? Australas Med J. 2014;7:465-70. [ Links ]
19.Eid SM,Boueiz A, Paranji S,Mativo C,Landis R,Abougergi MS. Patterns and predictors of proton pump inhibitor overuse among academic and non-academic hospitalists. Intern Med. 2010;49:2561-8. [ Links ]
20.Barletta JF, Sclar DA. Use of Proton pump inhibitors for the provision of stress ulcer prophylaxis: clinical and economic consequences. PharmacoEconomics. 2014; 32:5–13. [ Links ]
21.Ladd, AM, Panagopoulos, G, Cohen, J, Mar, N, Graham R. Potential costs of inappropriate use of proton pump inhibitors. Am J Med Sci. 2014;347:446-51. [ Links ]
22. Afif W, Alsulaiman R, Martel M, Barkun AN. Predictors of inappropriate utilization of intravenous proton pump inhibitors. Aliment Pharmacol Ther. 2007;25:609-15. [ Links ]
23.Craig DG, Thimappa R, Anand V, Sebastian S. Inappropriate utilization of intravenous proton pump inhibitors in hospital practice a prospective study of the extent of the problem and predictive factors. QJM. 2010;103:327-35. [ Links ]
24.Hoover JG, Schumaker AL, Franklin KJ. Use of intravenous proton-pump inhibitors in a teaching hospital practice. Dig Dis Sci. 2009;54:1947-52. [ Links ]
25.Bertakis KD,Azari R,Helms LJ,Callahan EJ,Robbins JA. Gender differences in the utilization of health care services. J Fam Pract. 2000;49:147-52. [ Links ]
26.Pham CQ, Regal RE, Bostwick TR, Knauf KS. Acid suppressive therapy use on an inpatient internal medicine service. Ann Pharmacother. 2006;40: 1261–6. [ Links ]
27. Hussain S, Stefan M, Visintainer P, Rothberg M. Why do physicians prescribe stress ulcer prophylaxis to general medicine patients? South Med J. 2010;103: 1103–10. [ Links ]
28.Heidelbaugh, JJ, Inadomi JM. Magnitude and economic impact of inappropriate use of stress ulcer prophylaxis in non-ICU hospitalized patients. Am J Gastroenterol. 2006;101:2200–05. [ Links ]
29.Wohlt PD, Hansen LA, Fish JT. Inappropriate continuation of stress ulcer prophylactic therapy after discharge. Ann Pharmacother. 2007;41:1611–6. [ Links ]
30. Heidelbaugh JJ, Goldberg KL, Inadomi JM. Magnitude and economic effect of overuse of antisecretory therapy in the ambulatory care setting. Am J Manag Care.2010;16: e228-34. [ Links ]
31. Zink DA, Pohlman M, Barnes M, Cannon ME. Long-term use of acid suppression started inappropriately during Hospitalization. Aliment Pharmacol Ther. 2005;21: 1203–9. [ Links ]
Correspondência: Luís Ramos dos Santos ramos_santos88@hotmail.com
Serviço de Medicina Interna, Hospital Central do Funchal, SESARAM EPE,
Estrada dos Marmeleiros, 9050-495 - Funchal
Conflicts of interest: The authors have no conflicts of interest to declare.
Financing Support: This work has not received any contribution, grant or scholarship.
Confidentiality of data: The authors declare that they have followed the protocols of their work center on the publication of data from patients.
Protection of human and animal subjects: The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Protecção de Seres Humanos e Animais: Os autores declaram que não foram realizadas experiências em seres humanos ou animais.
Direito à Privacidade e Consentimento Informado: Os autores declaram que nenhum dado que permita a identificação do doente aparece neste artigo.
Conflitos de Interesse: Os autores declaram a inexistência de conflitos de interesse na realização do presente trabalho.
Fontes de Financiamento: Não existiram fontes externas de financiamento para a realização deste artigo.
Recebido: 06/01/2017
Aceite: 08/02/2017














