Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Medicina Interna
versão impressa ISSN 0872-671X
Medicina Interna vol.27 no.3 Lisboa jul. 2020
https://doi.org/10.24950/O/69/20/3/2020
ARTIGOS ORIGINAIS / ORIGINAL ARTICLES
Troponin Elevation and Myocardial Injury in Patients Admitted to an Internal Medicine Department: Diagnostic and Prognostic Significance
Troponina Elevada e Lesão Miocárdica em Doentes Internados em Medicina Interna: Significado Diagnóstico e Prognóstico
Mafalda Carrington1  https://orcid.org/0000-0002-4491-5312
https://orcid.org/0000-0002-4491-5312
Margarida Jacinto2  https://orcid.org/0000-0003-1327-5890
https://orcid.org/0000-0003-1327-5890
Ana Sousa2  https://orcid.org/0000-0002-5182-6019
https://orcid.org/0000-0002-5182-6019
Joana Sant’Anna2  https://orcid.org/0000-0003-1815-5011
https://orcid.org/0000-0003-1815-5011
José Muñoz3  https://orcid.org/0000-0001-8766-1933
https://orcid.org/0000-0001-8766-1933
Tiago Tribolet de Abreu2  https://orcid.org/0000-0001-9013-1095
https://orcid.org/0000-0001-9013-1095
1Serviço de Cardiologia, Hospital do Espírito Santo de Évora, Évora, Portugal
2Serviço de Medicina Interna, Hospital do Espírito Santo de Évora, Évora, Portugal
3Serviço de Patologia Clínica, Hospital do Espírito Santo de Évora, Évora, Portugal
Abstract:
Introduction: An elevated troponin is often found in patients admitted to the hospital. The meaning and the classifications of patients with this elevation (myocardial injury, either acute or chronic, versus acute myocardial infarction, either type 1 or type 2) remains unclear. The aim of our study was to assess the meaning and to classify the patients admitted to an internal medicine department with an elevated troponin level.
Material and Methods: A clinical retrospective analysis of hospitalized patients admitted to an internal medicine department was conducted over a 2-year period. We identified patients with at least 2 troponin I measurements, and at least 1 above 0.1 ng/mL. Population was characterized according to demographics, cardiovascular risk factors, clinical presentation, treatment and prognosis. Troponin elevation was interpreted according to the fourth universal definition of myocardial infarction.
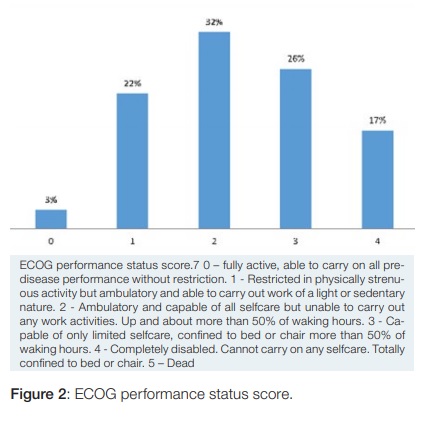
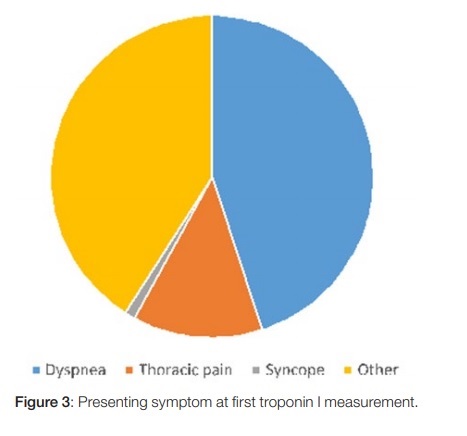
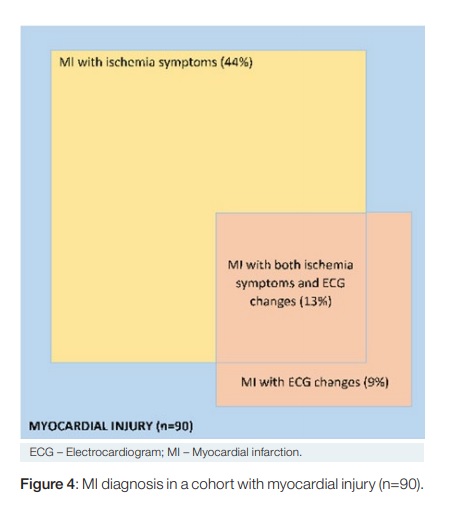
Results: A total of 90 patients were enrolled, with a mean age of 83 years ((± 8.1), 52% were male. Sixty patients (66%) had myocardial infarction criteria, and the remaining 30 patients (33%) were classified as acute myocardial injury, without infarction. We found no clinical difference between these patients, except for age, which was higher in myocardial infarction patients (84 ± 7 vs 81 ± 10 years, p = 0.039). Patients had a high disability score (43% had an ECOG 3 or 4), hypertension (89%), heart failure (51%), type 2 diabetes (50%), chronic kidney failure(35%), atrial fibrilation or flutter (35%) and had had a previous myocardial infarction (33%). Clinical presentation included dyspnea (44%) and chest pain (13%). On discharge, patients were prescribed a statin (64%) and antiplatelets (58%). In-hospital mortality was 17%, while 30 days and 1 year mortality were 27% and 51% respectively.
Conclusion: In this study, in a real-world cohort of patients admitted to an Internal Medicine department over a 2-year period, troponin levels were analyzed in 9%, and acute myocardial injury was found in one third of those patients. These patients had criteria for acute myocardial infarction in 66% and of acute myocardial injury without infarction in 33%. Age was higher in myocardial infarction patients, whilst there were no differences in other clinical, management or prognostic features. Patients were elderly and fragile, with a higher prevalence of several comorbidities, when compared with studies based on Cardiology departments. Mortality was high, with half the patients dying within a year, even with the prescription of statins in 64% and antiplatelets in 60%.
Keywords: Myocardial Infarction / diagnosis; Troponin; Troponin I.
Resumo:
Introdução: A elevação de troponina é frequente nos doentes internados. O seu significado e classificação (lesão miocárdica crónica versus aguda versus enfarte agudo de miocárdio (EAM), quer tipo 1, quer tipo 2) não se encontram esclarecidos. O objectivo deste estudo foi avaliar o significado e classificar as elevações de troponina em doentes internados numa enfermaria de Medicina Interna
Material e Métodos: Estudo retrospectivo de doentes internados, num período de dois anos, numa enfermaria de Medicina Interna, a quem foram pedidos, pelo menos, 2 doseamentos de troponina I, ao critério do médico assistente, e que tiveram pelo menos um valor acima do limite de referência de 0,1 ng/ mL. A população foi caracterizada quanto à demografia, factores de risco cardiovascular, antecedentes clínicos, achados clínicos e laboratoriais, terapêutica efectuada e prognóstico. Foi interpretada a elevação de troponina de acordo com a quarta definição de EAM.
Resultados: Foram incluídos 90 doentes, com idade média de 83 anos (± 8,1), sendo 52% do sexo masculino. Cumpriram critérios de EAM 60 doentes (66%), sendo que os restantes 30 doentes (33%) eram classificáveis como lesão miocárdica aguda, sem EAM. Não encontrámos diferenças clínicas, no tratamento e prognóstico entre estes dois grupos de doentes, à excepção da idade (84 ± 7 vs 81 ± 10 anos, respectivamente, p = 0,039). Os doentes tinham um performance status baixo (43% ECOG 3 ou 4), hipertensão arterial (89%), insuficiência cardíaca (51%), diabetes mellitus tipo 2 (50%), insuficiência renal crónica (35%), fibrilhação auricular ou flutter (35%) e enfarte agudo de miocárdio prévio (33%). A apresentação clínica incluiu dispneia em 44% e dor torácica em 13%. À data da alta, 64% dos doentes foram medicados com estatina e 58% com pelo menos um anti-agregante plaquetário. A morte ocorreu durante o internamento em 17%, sendo que a mortalidade a 30 dias foi de 27% e a um ano de 51%.
Conclusão: Neste estudo, verificámos que, dos doentes com elevação de troponina compatível com lesão miocárdica internados numa enfermaria de Medicina Interna, 66% cumpriam os critérios de definição de EAM, enquanto os restantes 33% tinham lesão miocárdica aguda, sem EAM. À excepção da idade (mais elevada nos doentes com EAM) não houve diferença significativa nas características clínicas, abordagem ou prognóstico entre os dois grupos. Os doentes eram idosos e frágeis, com múltiplas comorbilidades, tendo a morte ocorrido durante o internamento em 17%, aos 30 dias em 27% e ao 1 ano em 51%, apesar de prescrição de estatina em 64% e de antiagregação em 60%.
Palavras-chave: Infarto do Miocárdio/diagnóstico; Troponina; Troponina I.
Introduction
The Fourth Universal Definition of Myocardial Infarction1 clearly defined myocardial injury as being present when blood levels of cardiac troponin (cTn) are increased above the 99th percentile upper reference limit (URL). This injury may be acute, as evidenced by a newly detected dynamic rising and/or falling pattern of cTn, or chronic, in the setting of persistently elevated cTn levels. Acute myocardial injury in the setting of acute myocardial ischemia should be labelled as MI, and MI can be further classified into 5 types.
Since the publication of the first Universal Definition of of Myocardial Infarction in 2007, a particular interest on type 2 myocardial infarction (MI) has arisen.2 Evidence-based treatment recommendations for type 2 MI are lacking,3 and, in clinical practice, treatment strategies are frequently limited because of higher co-morbidity in this population. The prognosis of type 2 MI is also controversial.3 Consequently, there is still no clarification nor robust clinical evidence on type 2 MI epidemiology, diagnostic criteria, provoking conditions, management and prognosis,3 especially in the non-cardiology setting.4 Furthermore, the clinical relevance of distinguishing between type 2 MI fulfilling the Universal Definition criteria and myocardial injury without definite MI is not yet established.5
The aim of this study was to assess patients admitted to an internal medicine department with an elevated troponin level, and to investigate the characteristics, clinical causing conditions, management and outcomes of type 2 MI and myocardial injury without definite MI.
Material and Methods
The present study analyzed all patients admitted to a general Internal Medicine department in a 322-bed hospital, serving as a local hospital for a catchment area of 150 000 residents and as a secondary referral center for a region with 440 000 inhabitants. The hospital has both general and Coronary Intensive Care Units and the Cardiology department is equipped with a hemodynamic laboratory working 24/7.
We included for analysis all patients admitted to our General Internal Medicine department over a 2-year period from July 1, 2014 to June 30, 2016, who had at least 2 cardiac troponin I measurements, requested according to treating physician criteria, and presented at least 1 troponin I value above the upper reference limit of 0.1 ng/mL.6 We excluded patients with a single troponin I measurement, in which a rise and/or fall could not be perceived. Serum cardiac troponin I was measured using the Ortho-Clinical Diagnostics (Rochester, NY) Vitros Troponin I immunodiagnostic assay. The study was approved by the hospital´s Review Board with a waiver of informed consent.
We retrospectively collected detailed baseline and clinical data on the included patients. Computer and material medical records were reviewed for a history of cardiovascular risk factors, major adverse cardiac and cerebrovascular events, heart failure, peripheral arterial disease, chronic kidney disease (MDRD eGFR <60 mL/min/1.73 m²) and chronic respiratory problems. Similarly, medical record’s information was revised to determine how previous diseases impacted patient’s daily living abilities previously to index hospitalization, and ECOG performance status score7 was calculated accordingly for each patient. We searched for an electrocardiogram (ECG) performed at the moment of the first elevated troponin I, either printed or described in computer or material medical records by the treating physician. All ECG obtained were retrospectively reviewed and we also recorded symptoms that made the doctor take the first elevated troponin I measurement. Finally, mortality, hospital discharge destination, cardiovascular prescription medication and 30-day hospital re-admissions were analyzed. Mortality was analyzed by electronic access to primary care records. Cardiovascular medication prescribed was accessed using the national medical electronic prescription system.
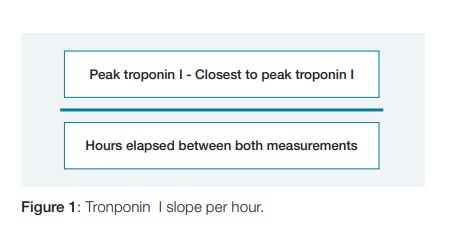
Relevant laboratory data was also registered. Since MI definition implies kinetics in serum troponin (rise or fall), we recorded a troponin I slope per hour. This was defined as the ratio between the difference between peak troponin I value and the closest obtained value to peak troponin I, and the time elapsed between both measurements in hours (Fig. 1).
Adjudication of the diagnosis of MI versus myocardial injury without definite MI was based on the Universal Definition of MI.1 MI was defined as a rise and/or fall of serum troponin above the 99% URL in the context of clinical evidence of ischemia, with at least 1 of the following: symptoms of ischemia; ECG changes with new significant ST-segment-T wave changes, new left branch block (LBBB), or development of pathological Q waves in the ECG; or imaging evidence of a new regional wall motion abnormality. Cases in which a rise and/or fall in serum troponin was observed in the absence of clinical evidence of ischemia (as defined above) were classified as myocardial injury without definite MI. Therefore, we created 2 groups – MI and myocardial injury without definite MI, and compared baseline characteristics, dis- charge treatment and mortality outcomes between both groups.
Finally, adjudication of myocardial injury etiology was based on specific clinical criteria that were previously published. Although the possible mechanisms of type 2 MI were recently recognized in the 4th Universal Definition of Myocardial Infarction,1 specific criteria were not yet defined and we used the parameters presented by other authors,13 if they were present within a span of 48-hours (from 24-hours before to 24-hours after) of the first elevated troponin I measurement:
· Anemia, defined as hemoglobin <8.9 g/dL for men and <8.1 g/dL for women.
· Shock, defined as systolic blood pressure (SBP) <90 mmHg together with signs of organ dysfunction - metabolic acidosis, arterial oxygen pressure <60 mmHg, oliguria or encephalo-pathy.
· Bradycardia requiring medical treatment or cardiac pacing.
· Respiratory failure with an arterial oxygen pressure <60 mmHg and clinical signs of acute respiratory failure lasting more than 20 minutes or a need for ventilation.
· Supraventricular tachycardia lasting ≥20 minutes, with a ventricular rate >150 beats/minutes.
· Ventricular tachycardia lasting ≥ 20 minutes.
· Severe hypertension, defined as:
a) SBP >160 mmHg and either signs of pulmonary edema or concomitant left ventricular hypertrophy,
b) SBP >180 mmHg or
c) Diastolic blood pressure >110mmHg.
Continuous variables were expressed as medians [interquartile range] and means ± standard deviation. Comparison between medians was performed using One-sample Wilcoxon Signed Rank Test (for variables with a non gaussian distribution) and comparison between means was performed using One-Sample T-Test (for variables with a gaussian distribution). Categorical variables were expressed as N (proportions) and in percentages and analyzes of these variables were performed using chi-squared test. Statistical analyses were performed using IBM SPSS Statistics 24.
Results
Among all patients admitted to our Internal Medicine department between July 2014 and June 2016, troponin I levels were determined (according to treating physician criteria) in 9%. Of these, we included for analysis 90 patients (corresponding to 35% of the patients with any troponin I measurement, and 3% of all patients), who met the inclusion criteria (at least 2 measurements of serum troponin I and at least 1 of them above the URL of 0.1ng/mL).
Demographics, past medical history, laboratory data, clinical characteristics, treatment and discharge data are shown in Tables 1 and 2. Our patients with myocardial injury were older (83 ± 8 years-old (yo)) than all the patients hospitalized in our Medicine department during the study period (75±15 years) (p < 0,001), and the majority were male in both groups (52%). The overall population had a poor performance status at baseline, with 26% of the patients scoring ECOG 3 and 17% being allocated a grade 4 (Fig. 2). We found a high prevalence of comorbidities among patients with myocardial injury, including hypertension in 81 (89%), heart failure in 46 (51%), chronic kidney disease in 32 (35%) and atrial fibrillation or flutter in 32 (35%). Evidence of prior history of coronary heart disease was present in some patients, as 30 (33%) had previous history of MI, of whom 20 (22%) had been studied with coronary angiography, of whom 4 (4%) had undergone CABG and 6 (7%) had been treated with percutaneous coronary intervention (PCI). Only 3 patients had cigarette smoking reported in our medical records.
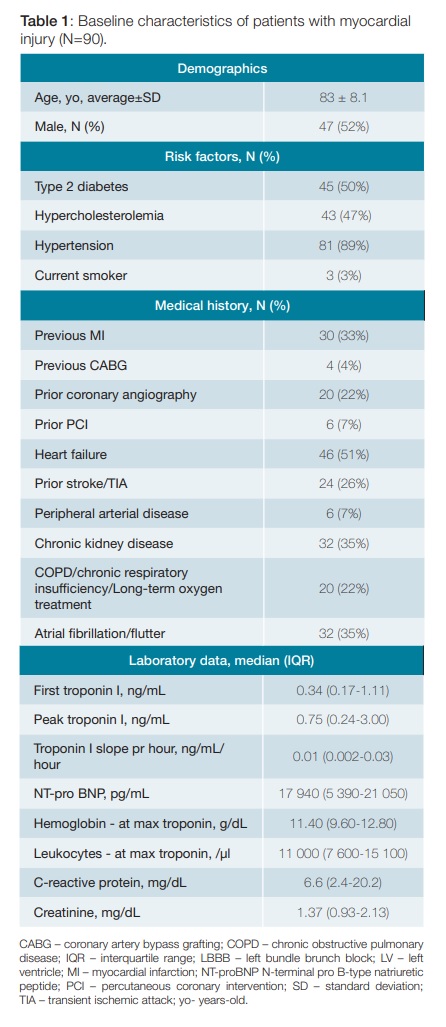
The most common manifestation in our patients was dyspnea (44%), and only 13% had chest pain (Fig. 3). Median peak troponin I was 0.75 (0.24-3.00) ng/mL and the median slope of troponin I in all the patients included was 0.01 (0.002-0.03) ng/mL/hour (Table 1). Only 38 (42%) of the patients had an ECG reported at the moment of the first elevated troponin I, the remaining only having an ECG described at admission or later during index hospitalization.
A total of 60 patients (corresponding to 66% of all included patients with myocardial injury, 23% of the patients with any troponin I measurement, and 2% of all patients over the 2-year period) met the Universal Definition criteria for acute myocardial infarction, and only 12 (13%) of them presented with both ECG changes and ischemia symptoms. The remaining 30 patients(33%) were classified as myocardial injury without definite MI (Fig. 4).
Possible causative conditions for myocardial injury and type 2 MI are shown in Fig. 5. The most common cause in our group of patients was respiratory failure (34%), followed by severe hypertension (21%). Sixty-six percent had more than one cause and in 34% of the patients, none of the pre-specified possible causes of type 2 MI was identified. At the time of the peak troponin I level, 58% of the patients showed hemoglobin values below 12 g/dL, 48% had leukocytes above 11 000/µl, 49% had C-reactive protein (CRP) above 5 mg/dL and 42% had a creatinine value superior to 1.5 mg/dL. The biomarker NT-proBNP was assayed in 75 (83%) of the patients and the median first NT-proBNP measured during index hospitalization was 17.940 (5.390-21.050) pg/mL.
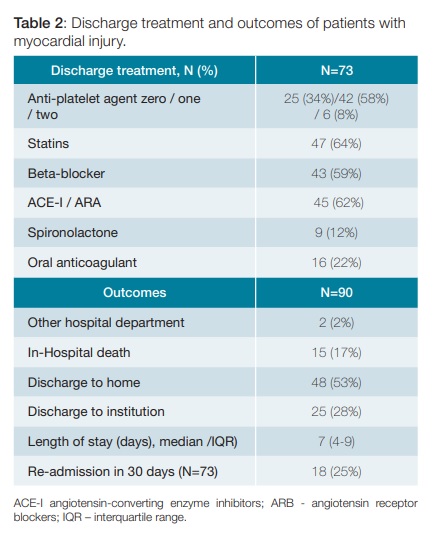
Seventeen percent (n = 15) of our patients with myocardial injury died during index hospitalization (Table 2), comparing to an in-hospital death incidence of 13% (n = 358) amongst all patients admitted to our Internal Medicine department. In those who survived, around 60% had one anti-platelet agent, a beta-blocker and/or an ACE-I prescribed at discharge and 64% received a statin. Only 8% of them were discharged while on two anti-platelet agents. Coro-nary angiography was performed in five patients, two had no significant lesions in the coronary arteries, two had a documented 3-vessel disease and only one had a culprit lesion which was treated with a drug-eluting stent. All-causes mortality rate at 30 days was 27%, and at 1 year it was 51%.
There were no differences in baseline characteristics, management and outcome between patients with MI (n = 60) and patients with myocardial injury without definite MI (n = 30), except for age (84±7 vs 81±10 yo, respectively, p = 0.039). Other variables considered were previous MI (35% vs 30%, p = 0.635), treatment at discharge with statin (76% vs 58%, p = 0.135) and/or 1 anti-platelet agent (67% vs 64%, p = 0.820), in-hospital (18% vs 13%, p = 0.549) or 1-year mortality (48% vs 54%, p = 0.655).
Discussion
This study showed that amongst all patients hospitalized in an Internal Medicine department, 90 patients had ongoing myocardial injury, and 60 (66%) met the MI criteria defined in the Third Universal Definition of MI. No significant differences in baseline characteristics, management or outcome were found between patients with MI and patients with myocardial injury without definite MI, except that patients in the former group were older. The most frequent possible causative conditions for myocardial injury were respiratory failure and severe hypertension and in 34% of them we could not identify any potential cause. Our patients with myocardial injury were old and frail, had multiple comorbidities and 17% experienced in-hospital death. Medication at discharge included more frequently statin therapy (64%) than previously described in other younger and healthier patients, and approximately the same proportion (60%) was treated with at least 1 anti-platelet agent.3,5,8 Despite frequent prescription of secondary prevention medication at discharge, we found disproportionally high 30-days (27%) and 1-year (51%) all-causes mortality rates.3-4,9,10
Similarly, other authors found no significant mortality differences between type 2 MI and myocardial injury without definite MI,5,8,12 and this finding made them question the relevance of distinguishing between both entities through the application of Universal Definition of MI’s criteria. One of the difficulties found while applying Universal Definition criteria in type 2 MI is related to the associated co-morbidities and clinical conditions that are frequently recognized to limit the appropriate recognition of ischemia symptoms and ECG-changes documentation.9,10 Accordingly, in our Internal Medicine department’s patients, presentation with chest pain was rarer than described in previous studies (13% versus >51%), and dyspnea was more frequent
(44% versus <19%).3-4,8-10 Only 38 (42%) of our patients had an ECG performed at first elevated troponin I measurement and we were unable to identify any diagnostic ECG change1 in 20 (22%) patients. Furthermore, median peak troponin I was 0.75 ng/mL (0.24-3.00), and this was not significantly different from values reported by other authors (p = 0.84 and p = 0.513), who also described higher levels of this biomarker in type 1 MI. All these aspects emphasize the limitations in the application of Universal Definition criteria in the case of type 2 MI, and reinforce difficulty in distinguishing it from acute myocardial injury. Contrarily, the latter can easily be defined based on troponin I elevation and variation, and these two were the main criteria used for inclusion of patients in our study. A very slow variation in troponin I levels (0.01 ng/mL per hour) was calculated and we cannot exclude that this slow variation was due to chronic, rather than acute myocardial injury. However, we did not intend to distinguish between these two entities, but to analyze hospitalized patients who had ongoing myocardial injury reportable to co-morbid conditions. There is increasing evidence that even slight variations in detectable concentrations of troponin is associated with an impaired outcome in specific clinical settings.14-16 We then hypothesize that studying troponin I slope per hour using high-sensitivity troponin I can shed light upon the importance of the kinetics of troponin in distinguishing between MI and myocardial injury, as well as between MI types.
Another possible approach to type 2 MI and myocardial injury classification and diagnosis relates to possible causative etiologies, which are clinical conditions that origin imbalances between myocardial oxygen supply and demand. Many authors have adjudicated the diagnosis of type 2 MI to the subjective opinion of physician panels, without applying strict parameters.3,9,12 In other studies, specific clinical criteria were proposed for the diagnosis of type 2 MI.2,5,10,13 We decided to study the frequency of these conditions, by applying specific clinical criteria in our patients with myocardial injury. The two most frequent possible causative conditions were respiratory failure (34%) and severe hypertension (21%). This data differed from that found in previous studies,4-5,9-10,13 in which severe anemia was identified as a leading cause; nevertheless, median hemoglobin concentrations in our patients were significantly lower than those found by some of the authors (p < 0.001).2,4,10
There is a lack of data on the frequency and baseline characteristics of patients with these conditions, and this is possibly due to the challenge in defining and differentiating between type 2 MI and myocardial injury. Most of the studies comparing type 1 and type 2 MI are designed in a retrospective way, as shown by a recently published meta-analysis,17 and some have reported very low incidences of type 2 MI. This is possibly due to a selection bias of the study population, as most of the patients studied were collected from Cardiology departments and/or after being diagnosed with a MI.3-4,9,10,13 We decided to specifically study patients from an Internal Medicine department, because this population is much more susceptible to develop myocardial injury and the so-called type 2 MI. As a result, we obtained a more ill3-5,8-13 population, with older patients who were previously more dependent in activities of daily living.9 We found a considerably higher prevalence of previous hypertension and diabetes mellitus in our patients (89% versus <81% and 50% versus <36%, respectively)4-5,8,10-12 and we had higher rates of prior stroke or transient ischemic attack (TIA)4,8,10,11 and COPD.3,9 More importantly, our patients with myocardial injury had about twice the prevalence of congestive heart failure (51% versus <26%).2-5,9,13 Therefore, we suggest that future research on myocardial injury and type 2 MI should be based on Internal Medicine departments rather than on Cardiology departments, as baseline characteristics of these patients are contrasting and relate to possible causative conditions for myocardial injury, potentially influencing the prognosis of these patients.
There are a number of limitations to this small observational study. First, clinical criteria such as ischemia symptoms and ECG changes were evaluated retrospectively; therefore, ascertainment bias may have affected the diagnosis of MI. Secondly, only five of our patients had a coronary angiography performed, so we could not definitely exclude type 1 MI. Finally, the reduced number of patients analyzed may not have allowed to accurately compare characteristics, management and outcomes between type 2 MI and myocardial injury without definite MI.
Conclusion
In this study, in a real-world cohort of patients admitted to an Internal Medicine department over a 2-year period, troponin levels were analyzed in 9%, and acute myocardial injury was found in one third of those patients. These patients had criteria for acute myocardial infarction in 66% and of acute myocardial injury without infarction in 33%.
Age was higher in myocardial infarction patients, whilst there were no differences in other clinical, management or prognostic features. Patients were elderly and fragile, with a higher prevalence of several comorbidities, when compared with studies based on Cardiology departments. Mortality was high, with half the patients dying within a year, even with the pre-scription of statins in 64% and antiplatelets in 60%.
We suggest that future research on myocardial injury and type 2 MI should be based on Internal Medicine departments rather than on Cardiology departments.
REFERENCES
1. Thygesen K, Alpert JS, Jaffe AS, Chaitman BR, Bax JJ, Morrow DA, et al. Fourth Universal definition of myocardial infarction. J Am Coll Cardiol. 2018;72:2231-64. doi: 10.1016/j.jacc.2018.08.1038. [ Links ]
2. Saaby L, Poulsen TS, Diederichsen ACP, Hosbond S, Larsen TB, Schmidt H, et al. Mortality Rate in Type 2 Myocardial Infarction: Observations from an Unselected Hospital Cohort. Am J Med. 2014;127:295-302. [ Links ]
3. López-Cuenca A, Gómez-Molina M, Flores-Blanco P, Sánchez-Martínez M, García-Narbon A, Heras-Gómez I, et al. Comparison between type-2 and type-1 myocardial infarction: clinical features, treatment strate- gies and outcomes. J Geriatr Cardiol. 2016;13:15-22. doi: 10.11909/j.issn.1671-5411.2016.01.014. [ Links ]
4. Baron T, Hambraeus K, Sundström K, Erlinge D, Jernberg T, Lindahl B. Type 2 myocardial infarction in clinical practice. Heart. 2015;101:101-6. doi: 10.1136/heartjnl-2014-306093. [ Links ]
5. Smilowitz NR, Weiss MC, Mauricio R, Mahajan AM, Dugan KE, Devanabanda A, et al. Pro-voking conditions and outcomes of type 2 myocardial infarction and myocardial necrosis. Int J Cardiol. 2016;218:196-201. doi: 10.1016/j.ijcard.2016.05.045. [ Links ]
6. Morrow DA, Cannon C, Jesse R, Newby LK, Ravkilde J, Storrow AB, et al. National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines: Clinical Characteristics and Utilization of Biochemical Markers in Acute Coronary Syndromes. J Clin Chem. 2007;53:552-74. [ Links ]
7. Oken M, Creech R, Tormey D, Horton J, Davis TE, McFadden ET, et al. Toxicity And Response Criteria Of The Eastern Cooperative Oncology Group. Am J Clin Oncol. 1982;5:649-55. [ Links ]
8. Shah A, McAllister DA, Mills R, Lee KK, Churchhouse A, Fleming KM, et al. Sensitive Tro-ponin Assay and the Classification of Myocardial Infarction. Am J Med. 2015;128:494-501. doi: 10.1016/j.amjmed.2014.10.056. [ Links ]
9. Stein G, Herscovici G, Korenfeld R, Matetzky S, Gottlieb S, Alon D, et al. Type-II Myocardial Infarction – Patient Characteristics, Management and Outcomes. PLoS One. 2014;9:e84285. doi: 10.1371/journal.pone.0084285.
10. Szymanski F, Karpinski G, Platek A, Majstrak F, Hrynkiewicz-Szymanska A, Kotkowski M, et al. Clinical characteristics, aetiology and occurrence of type 2 acute myocardial infarction. Kardiol Pol. 2014;72:339-44. doi: 10.5603/KP.a2013.0284. [ Links ]
11. Nestelberger T, Boeddinghaus J, Badertscher P, Twerenbold R, Wildi K, Breitenbücher D, et al. Effect os definition on incidence and prognosis of type 2 myocardial infarction. J Amn Coll Cardiol. 2017;70:1558-68. doi: 10.1016/j.jacc.2017.07.774. [ Links ]
12. Javed U, Aftab W, Ambrose J, Wessel RJ, Mouanoutoua M, Huang G, et al. Frequency of Elevated Troponin I and Diagnosis of Acute Myocardial Infarction. Am JCardiol. 2009;104:9-13. [ Links ]
13. Saaby L, Poulsen TS, Hosbond S, Larsen TB, Diederichsen AC, Hallas J, et al. Classification of Myocardial Infarction: Frequency and Features of Type 2 Myocardial Infarction. Am J Med. 2013;126:789-97. [ Links ]
14. Masson S, Anand I, Favero C, Barlera S,Vago T,Bertocchi F, et al. Serial measurements of cardiac troponin T using a highly sensitive assay in patients with chronic heart failure: data from two large randomized clinical trials. Circulation. 2012;125:280-8. [ Links ]
15. Pavasini R, dAscenzo F, Campo G,Biscaglia S,Ferri A,Contoli M, et al. Cardiac troponin elevation predicts all-cause mortality in patients with acute exacerbation of chronic obstructive pulmonary disease: systematic review and meta-analysis. Int J Cardiol. 2015;191:187-93. doi: 10.1016/j.ijcard.2015.05.006. [ Links ]
16. Peacock W, Marco T, Fonarow G, Diercks D, Wynne J, Apple FS, et al. Cardiac troponin and outcome in acute heart failure. NEJM. 2008;358:2117-26. [ Links ]
17. Gupta S, Vaidya S, Arora S, Bahekar A, Devarapally S. Type 2 versus type 1 myocardial infarction: a comparison of clinical characteristics and outcomes with a meta-analysis of observational studies. Cardiovasc Diagn Ther. 2017;7:348-58. doi: 10.21037/cdt.2017.03.21. [ Links ]
Responsabilidades Éticas
Conflitos de Interesse: Os autores declaram a inexistência de conflitos de interesse na realização do presente trabalho.
Fontes de Financiamento: Não existiram fontes externas de financiamento para a realização deste artigo.
Confidencialidade dos Dados: Os autores declaram ter seguido os protocolos da sua instituição acerca da publicação dos dados de doentes.
Proteção de Pessoas e Animais: Os autores declaram que os procedimentos seguidos estavam de acordo com os regulamentos estabelecidos pelos responsáveis da Comissão de Investigação Clínica e Ética e de acordo com a Declaração de Helsínquia da Associação Médica Mundial.
Proveniência e Revisão por Pares: Não comissionado; revisão externa por pares.
Ethical Disclosures
Conflicts of interest: The authors have no conflicts of interest to declare. Financing Support: This work has not received any contribution, grant or scholarship
Confidentiality of Data: The authors declare that they have followed the protocols of their work center on the publication of data from patients.
Protection of Human and Animal Subjects: The authors declare that the procedures followed were in accordance with the regulations of the relevant clinical research ethics committee and with those of the Code of Ethics of the World Medical Association (Declaration of Helsinki).
Provenance and Peer Review: Not commissioned; externally peer reviewed.
© Autor (es) (ou seu (s) empregador (es)) e Revista SPMI 2020. Reutilização permitida de acordo com CC BY-NC. Nenhuma reutilização comercial.
© Author(s) (or their employer(s)) and SPMI Journal 2020. Re-use permitted under CC BY-NC. No commercial re-use.
Correspondence / Correspondência:
Tiago Tribolet de Abreu – ttabreu@hevora.min-saude.pt
Serviço de Medicina Interna, Hospital do Espírito Santo de Évora, Évora, Portugal
Largo do Sr. da Pobreza, 7000-811 Évora
Received / Recebido: 24/04/2020
Accepted / Aceite: 16/06/2020
Publicado / Published: 28 de Setembro de 2020














