Introduction
Systemic sclerosis (SSc) is a chronic inflammatory systemic disease, being the most severe within the scleroderma spectrum, with high case-specific mortality.1,2Although its pathogenesis is shared by other similar autoimmune conditions including immune-inflammatory processes, vasculopathy and fibrosis, its triggers and aetiologies remain unknown.2,3In more than 80% of the patients, autoantibodies have been identified years before the clinical onset of the disease, and therefore they are essential for an early diagnosis and treatment of these diseases.1,4Traditional classification of SSc defines this as diffuse or limited disease, depending on the extent of skin sclerosis. The clinical association with high-titer SSc patterns of ANA reactivity, generally mutually exclusive, allows to define the risk of specific complications, providing a complementary subgrouping for SSc that could enlighten therapeutic enhancements.2 Anti-Th/To antibodies are directed against subunits of human mitochondrial RNase and RNase P ribonucleoprotein complexes and produce a typical nucleolar staining pattern on IIF.5 Anti-Th/To antibodies are considered fairly specific to SSc and may be present in 2- 10% of patients.1,5 They may also be detected in primary Raynaud’s phenomenon, however, they aren’t present in systemic lupus erythematosus; polymyositis / dermatomyositis and in undifferentiated connective tissue disease.6,7Antibodies NOR90 were first identified as a novel 90-kDa protein recognized by autoantibodies that selectively stained the nucleolus organizing region (NOR) of chromosomes 13, 14, 15, 21, and 22. The 90-kDa autoantigen was later proved to be identical to human upstream-binding factor, an RNA polymerase I-specific transcription factor which plays a central role in transcriptional regulation of rRNA.4 Based on search, NOR90 is present in ~5% of SSc cases with low specificity, since it’s been also associated with other autoimmune conditions such rheumatoid arthritis, systemic lupus erythematosus; Sjögren’s syndrome or neoplastic diseases.1,5,8We examined clinical and etiologic diagnosis associated to Anti-Th/To and NOR90 autoantibodies in a cohort of patients followed in an autoimmune consultation.
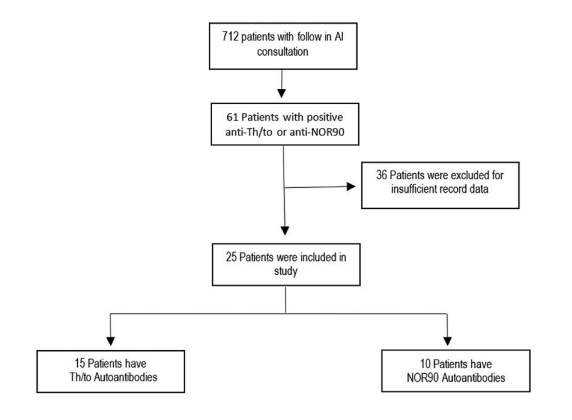
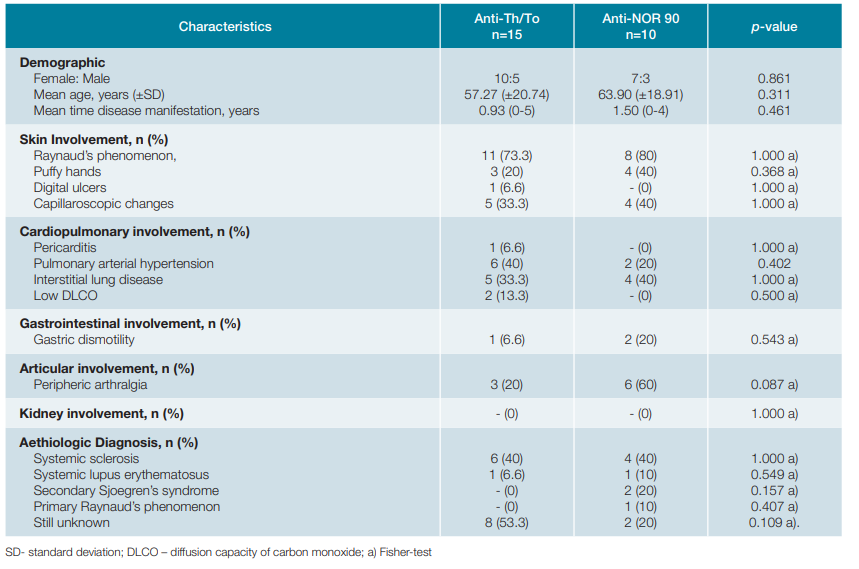
Methods In this observational retrospective study, from a total of 712 patients with follow-up in autoimmune consultation of a single centre, we included all 61 patients with positive anti-Th/ To or NOR90 antibodies, from January 2018 to March 2020. Clinical information was obtained from electronic medical records. All patients with loss of follow-up from consultation or absence of specific clinical data were excluded. Demographic characteristics, clinical features and etiologic diagnosis of the selected patients were analysed and compared between anti-Th/To and anti-NOR90 groups. All data were statistically analysed using IBM SPSS Statistics version 26.0®. Categorical variables are presented as number of cases or percentages. Continuous variables are presented as mean and standard deviation. In the bivariate analysis we used chi-square test or fisher-test as appropriated for categorical variables. The Mann Whitney U Test was used for continuous variables. All reported p-values are two-tailed and statistical significance was considered if p-value a mean time of 0.93 years from disease overall manifestations to diagnosis, with maximum period observed of 5 years (Table 1).
Skin involvement had Raynaud’s phenomenon present in 73% with capillaroscopic changes in 33.3% cases and peripheric arthralgia was identified in 20% of patients (Table 1). Cardiopulmonary manifestations with pulmonary arterial hypertension and interstitial lung disease were documented in 40% and 33.3% of patients, respectively, and pericarditis was diagnosed in 6.6% of patients (Table 1). None had kidney affections (Table 1). Systemic sclerosis was established in 40% of the Th/To autoantibody patients and systemic lupus erythematosus diagnosis was assumed in 1 patient (Table 1). Half of patients of this group still had no diagnosis assumed link to positive Th/To autoantibody (Table 1). In NOR90 autoantibody group, female gender was also more prevalent with a mean age of 63.90 (± 18.91) years and mean time from overall disease manifestation to diagnosis of 1,5 years, with maximum period observed of 4 years (Table 1). Skin involvement had Raynaud’s phenomenon present in 80% and was confirmed by capillaroscopic changes in 40% of cases (Table 1). Gastroenterology manifestations were verified in 20% patients (Table 1). Kidney affections were not documented (Table 1). Systemic sclerosis was the diagnosis determined in 40% of the NOR90 autoantibody group and systemic lupus erythematosus and secondary Sjoegren’s syndrome diagnosis were concluded in 10% and 20%, respectively (Table 1). None had neoplastic diagnosis. In both groups there weren’t any results with statistical significance (Table 1).
As shown in Table 2, there were not any other autoantibodies associations in 53.3% of Th/To group. In 4 of these patients, there were documented SSc diagnosis. In this study, 5 autoantibody type associations were documented, with anti- -Ro52 (3 cases) and anti-Ku (2 cases) being the most frequent (Table 2).
Table 2: Autoantibodies associations in anti-Th/To group
| SSc Autoantibodies Positive Associations | Anti-Th/To n=15 | Diagnosis |
|---|---|---|
| Anti-Ku | 2 | Still unknown |
| Anti-PM Scl75 | 1 | Still unknown |
| Anti-Ro52 | 3 | 1 case SLE, 1 case SSc, 1 case still unknown |
| Anti-RNA polymerase III; Anti-Centromere B | 1 | SSc |
| No associations | 8 | 4 cases SSc, 4 cases still unknown |
SLE- systemic lupus erythematosus
As shown in Table 3, there were not any other autoantibodies associations in half of the cases of NOR90 group and of these, one patient had SSc diagnosis. In the NOR90 group 5 different autoantibody type associations were also registered and the most prevailing one was with anti-Ku (4 cases with different combinations).
Table 3: Autoantibodies associations in anti-NOR90 group
| SSc Autoantibodies Positive Associations | Anti-NOR90 n=10 | Diagnosis |
| Anti-Ku | 1 | SLE |
| Anti-Scl70 | 1 | SSc |
| Anti-Ku, Anti-PM Scl100 | 1 | SSc |
| Anti-Ku, Ant-Ro52, Anti-PMScl75 | 1 | Still unknown |
| Anti-Ku, Anti-Centromere | 1 | SSc |
| No Associations | 5 | 1 case SSc, 2 cases SSs, 1 case PRp, 1 case still unknown |
SLE- systemic lupus erythematosus; SSs- secondary sjoegren’s syndrome; PRp- primary raynaud’s phenomenon
Discussion
In this study, anti-Th/To and anti-NOR 90 groups were similar in respect to clinical manifestations and etiologic diagnosis. According to literature, anti-Th/To is associated with shorter onset disease.5 In this group, the mean time from clinical manifestations to diagnosis was less than a year and skin symptoms were the earlier ones, with particular focus on Raynaud’s phenomenon. Peripheral arthralgia was described in a considerable percentage of this group. Cardiopulmonary features are frequently documented with pulmonary hypertension; interstitial lung disease and inflammatory muscle disease related.5,7,9In our study, cardiopulmonary involvement was more prevalent in comparison with the NOR90 group and pulmonary arterial hypertension was the most common manifestation. Our data confirm the absence established between anti-Th/To antibodies and renal impairment, since no patient had kidney involvement.5,7Only 1 patient was diagnosed with systemic lupus erythematosus which could be justified by an overlap of autoimmune pathologies as this autoantibody wasn’t previously related to this disease.6,7NOR90 autoantibodies have been considered as a marker of limited cutaneous SSc and mild involvement of internal organs.5 In this study we disclose higher prevalence of skin manifestations comparing with other symptoms and with anti- -Th/To group. Our data also confirm gastrointestinal involvement with gastric dysmotility demonstrated in a considerable percentage of these patients. No case of pericarditis, low DLCO or kidney involvement were identified in patients with anti-NOR90. Systemic lupus erythematosus and Sjögren’s syndrome were other etiological diagnosis identified in this population, validating its low systemic sclerosis specificity.5 Although rare, in this study, 4 patients with anti-Th/To and 1 patient with anti-NOR90, with established SSc diagnosis, did not have any association with other more common SSc’s autoantibodies, revealing the importance of their active search when SSc is suspected, especially for Th/To. Results are limited, influenced by the reduced number of cases, partially due to limited search on these two autoantibodies. Clinical prospective trials with a larger population are needed for more conclusive results.
Conclusion
In this study, anti-Th/To and anti-NOR 90 groups were similar in respect to clinical manifestations and etiologic diagnosis. Both groups had more frequent skin and articular manifestations with more cardiopulmonary involvement in anti-Th/to and gastrointestinal symptoms in anti-NOR90 group. Active search of Th/To and NOR 90 autoantibodies could be beneficial when systemic sclerosis disease is suspected, since in this study they were singly positive in 20% of these cases. A larger population study is needed to strive for more conclusive results.