Introduction
The paramedian territories of the thalami are supplied by perforating thalamic arteries of posterior circulation through 1 of 4 variants (Fig. 1). Variant I is the most common with perforating branches arising from both posterior cerebral arteries (PCAs) accounting for about 55% of cases. In variant IIa the left P1 segment is the source of both paramedian arteries (12% of cases) while in variant IIb, perforating arteries derive from the artery of Percheron (AOP) that arises from a part of the posterior cerebral artery (21% of cases). Finally, in variant III there is an arterial arc bridging PCAs together (12% of cases).1-4
AOP is an uncommon single-artery pathology that can affect bilateral thalamic structures. Bilateral thalamic infarction is rare representing around 0.6% of stroke cases and 22%-35% of thalamic infarcts.5-6
More frequent ischemic strokes such as those affecting the middle cerebral artery, produce predictable focal neurological deficits and clinical syndromes. In contrast, AOP infarcts lead to a spectrum of clinical presentations that include altered mental status, from transient or episodic loss of consciousness to coma, memory impairment, psychosis, aphasia, dysarthria, and oculomotor dysfunction.7-13The unusual presentations (symptoms and signs) are one of the reasons why AOP strokes are often missed. Other contributors are the difficulty of detecting the infarct on primary imaging and also the lack of acknowledgment of this clinical entity given its rarity.14
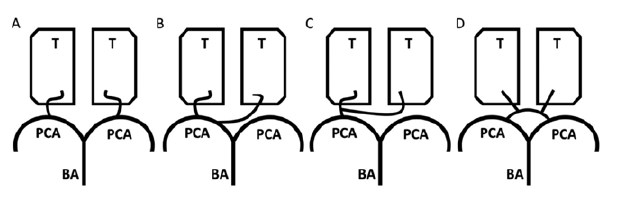
Figure 1: Paramedian thalamic artery variants. A - Type I, most frequent variant anatomy with perforating branches supplying the thalami (T) arising from the both posterior cerebral arteries (PCAs) that derive from the basilar artery (BA); B - Type IIa, both paramedian arteries originate from the P1 segment of the left PCA; C - Type IIb, the artery of Percheron (AOP) originates unilaterally from the P1 segment of PCA and then bifurcates, supplying the bilateral paramedian thalamus; D - Type III, na arterial arc connects the left and right P1 segments of PCA and gives rise to the paramedian arteries. Adapted from Amin OS, et al. Bilateral infarction of paramedian thalami: a report of two cases of artery of Percheron occlusion and review of the literature. BMJ Case Rep. 2011 ;2011:bcr0920103304.1
Case Report
A 93-year-old Portuguese female, partially dependent (Katz 3) due to osteoarthritis with no other medical history or co-morbidities was found unresponsive in the morning, eight hours after her last witnessed normal baseline. Her family was unable to awake her, prompting them to call emergency services that transported her to the hospital.
Remaining history and review of systems were limited by the patient’s condition. Physical exam on arrival to the emergency department revealed a comatose patient. She had minimally reactive, positioned at midline and symmetrical 4 mm pupils with no abnormal ocular movements and preserved corneal reflexes. Deep tendon reflexes were preserved, and muscle tone was decreased, although the patient was able to move her extremities in response to painful stimuli with apparent decrease in mobility affecting her right side. Plantar responses were flexor on both sides. The respiratory pattern was normal and cardiovascular and other systemic examination was unremarkable.
No pharmacological context that could contribute to the clinical picture was identified. Nonetheless, a putative opioid or benzodiazepine intoxication was excluded through naloxone and flumazenil administration without response.
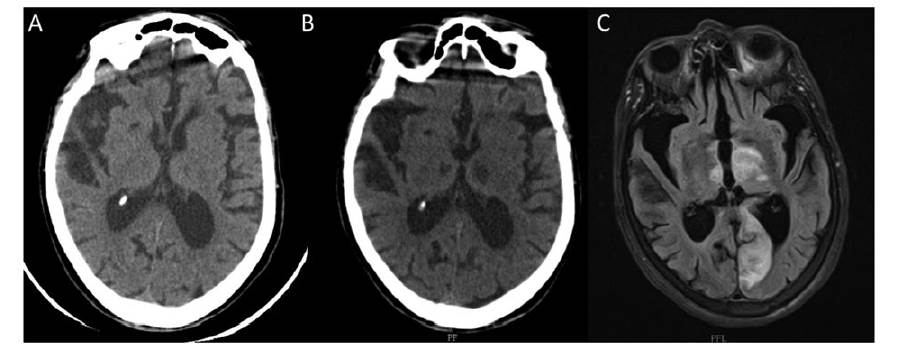
Biochemical laboratory tests and blood counts were normal, and electrocardiogram was unremarkable. The initial computed tomography (CT) scan of the head without contrast documented previous right lacunar infarct and microvascular
ischemic disease. No acute intracranial pathology was found (Fig. 2a).
Based on the vague clinical signs presented, poor focal findings, and lack of evidence supporting acute ischemia on imaging study, there was low suspicion for acute stroke and the patient was admitted for clinical surveillance and for diagnostic workup. Forty-eight hours after admission, the CT scan was repeated allowing the identification of hypodensities visible on both thalami, more evident on the left side extending to mesencephalic region. Twenty-four hours later diffusion-weighted magnetic resonance imaging (MRI) was performed revealing acute infarcts in the bilateral thalami extending toward the ventral midbrain compatible with an acute ischemic lesion affecting the AOP territory with evidence of haemorrhagic transformation (Fig.s 2b and 2c). Echocardiography, Holter and carotid ultrasound showed no clues regarding infarction aetiology.
Throughout the hospital stay, the patient maintained the comatose state and was transferred to a continuing care unit.
Figure 2: Brain imaging across time. A) Head computed tomography (CT) scan at admission showing no acute intracranial pathology documenting previous right lacunar infarct and microvascular ischemic disease (figure 2a). B) CT at 48 hours after admission
demonstrating hypodensities visible on both thalami, more evident on the left side extending to mesencephalic region. C) T2-weighted brain MRI at 24 hours after admission picturing subacute bilateral infarcts affecting both thalami and mesencephalon most evident on the left along with subacute infarct affecting the territory of left posterior cerebral artery with evidence of hemorrhagic transformation.
Discussion
The thalamus is a bilateral structure composed of several nuclei serving as a “relay centre” for a broad spectrum of neurological functions that include movement, arousal, cognition, behaviour, and emotion. This justifies the many possible presentations of an AOP stroke and reinforces the need for awareness of those. The clinical presentation may vary widely from mild symptoms such as dizziness and confusion to severe signs like coma.8,15Classic manifestations include altered level of consciousness, vertical gaze palsy, and cognitive impairment although classic signs of a stroke or focal lesion, as aphasia, dysarthria, and oculomotor disturbance may also be present.15Table 1 summarizes the common presentations seen in AOP infarction. Considering the anatomic correlates proposed in the literature, our patient’s decreased level of arousal probably is due to intralaminar nuclei damage given its input from the brainstem ascending reticular activator mechanism, which mediates alert consciousness.14
Table 1: AOP infarcts presentations in the literature.
| Category | Clinical manifestation | Refs |
|---|---|---|
| Mental status changes | Somnolence, stupor, and coma. | (3,8,12,15) |
| Behavior and memory impairment | Confusion, delirium, psychosis, apathy, hyperphagia, and pseudobulbar affect. | (9,10) |
| Ocular movement abnormalities | Horizontal and vertical gaze paresis with or without pupillary involvement | (3) |
| Motor deficits | Paresis or paralysis affecting the face or limbs. | (15) |
| Cerebellar alterations | Ataxia and dysmetria. | (12) |
| Speech abnormalities | Aphasia, dysarthria and slurred speech. | (15) |
| Other nonspecific alterations | Drowsiness, tremors, seizures, hyperthermia and bradycardia | (7,15) |
The literature reports similar aetiologies as for other perforating arteries infarctions. In a study by Xu et al, the most frequent cause of AOP infarction was small vessel disease, followed by cardioembolism.15 CT imaging frequently misses abnormalities in acute AOP infarction as was the case for our patient at admission. The same happens with CT angiography since occlusions in such small calibre arteries are usually not identified. MRI, on the contrary, has been shown to detect all AOP stroke cases in a small series.15 As result, many patients with AOP stroke remain undiagnosed several hours/days until MRI is performed.
The vague presentation of the case presented herein and negative CT scan at admission concurred to an initial low suspicion level of a cerebrovascular event. Added to the unavailability of MRI at the emergency department, the diagnosis was delayed compromising both treatment and prognosis.
Early detection and intervention significantly impact functional outcomes for patients.
Our report serves as a reminder to consider AOP infarct as differential diagnosis when assessing patients with unspecific neurological deficits of unclear origin, namely unexplained depressed level of consciousness. A low threshold
for MRI in patients presenting acutely with otherwise unexplainable neurological symptoms may facilitate diagnosis and decrease morbidity.