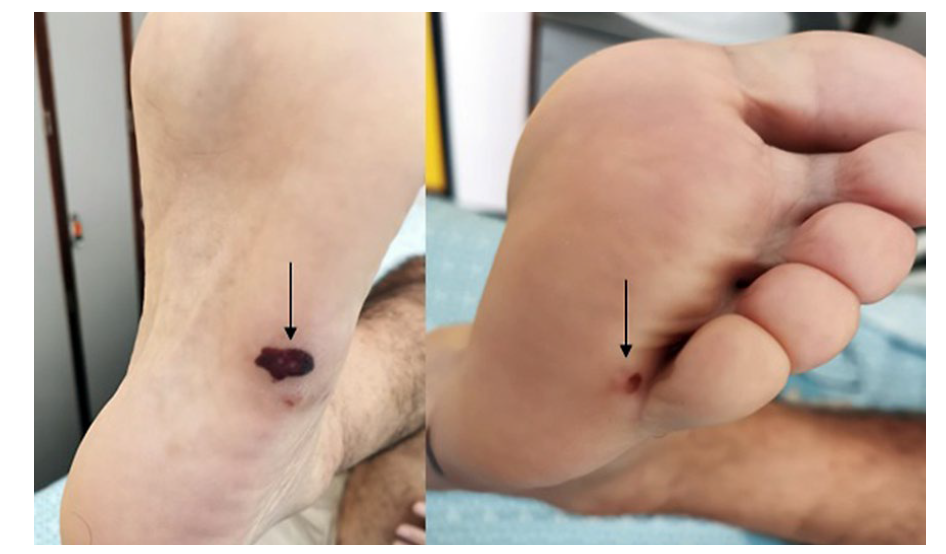
A 58-year-old man, with medical background of mitral valve prolapse and dental caries presented with a 12-day evolution of fever, malaise, low back pain and decreased visual acuity. Physical examination revealed small tender purplish nodules on palms of both hands (Fig. 1) and macular hemorrhagic lesions on the right foot (Fig. 2). No recent dental treatments were reported. Complementary study showed mitral valve endocarditis, lumbar spondylodiscitis and retinitis. A methicillin-resistant Staphylococcus aureus was isolated from blood cultures. The patient developed mitral regurgitation due to tendinous cord’s rupture, requiring urgent valve replacement. Valvular vegetations revealed the same agent. Antibiotic treatment with vancomycin, and posteriorly linezolid, led to re-solution of the lesions and clinical improvement.
Osler’s nodes are areas of painful nodular erythema, sometimes with a pink colour, usually localized on the tip of the fingers and toes, the sides of the fingers, and the thenar and hypothenar eminences.1Janeway lesions occur on the palms and soles, are non-painful and usually hemorrhagic.1 Infective endocarditis is the most common condition associated with these lesions.1 Their pathogenesis is a contested topic in the literature.1-3 Histological examination of Osler’s nodes often shows findings of sterile vasculitis, so they are considered mostly an immunologic phenomenon.2,3 On the other hand, because histological studies of Janeway lesions have revealed dermal neutrophilic microabscesses without evidence of vasculitis, and bacterial cultures are often positive, these lesions are thought to result directly from septic microemboli.2 Some data revealed that patients with Osler´s nodes and Janeway lesions had a higher rate of infective endocarditis related extracardiac complications,4 which is the case of this patient.
The authors highlight the differences between these two phenomena and their relevance on the diagnosis of infective endocarditis.