Introduction
Nosocomial infections (NI) pose a major healthcare problem with preventable associated costs. As stated by the Centres for Disease Control and Prevention (CDC), NI are a localized or systemic condition resulting from exposure to an infectious agent, at least after 48 hours of hospital admission.1 NI are associated with an increase in complications, morbidity and mortality, and an excess cost, either by direct burden of length of stay or by loss of active days.2 As of 2015, World Health Organization (WHO) has considered it a major public health problem.3 Like many adverse events, NI are potentially preventable. Efforts towards its reduction have been made by implementing local and global infection prevention and control (IPC) protocols and programs aiming to reduce NI and its costs. Best practice manuals encompass measures toward:
better hand hygiene and respiratory/cough etiquette;
equipment and surface sterilization;
screening of carriers or individuals with NI risk factors;
isolation of infected individuals, usage of personal pro-tection equipment, and creation of local commissions for outbreaks management,
proper residue and clothing handling.4
In the turn of 2019, a series of atypical pneumonia was identified in the Wuhan province of China. Viral genome sequencing was performed, and a new coronavirus (SARS-CoV-2) was identified in bronchoalveolar lavage fluid and bronchoalveolar epithelial cultures.5 Human-to-human transmission was confirmed, and it is now known that it occurs either by means of contact with droplets, coming from coughing or sneezing, faeces or by direct contact.6 Given the absence of specific direct treatment or vaccine, soon there was the need for stopping the chain of transmission by means of hand washing, generalized mask use, and social distancing. Health care professionals present an important vector of transmission and, given that asymptomatic individuals can still transmit the SARS-CoV-2, generalized preventive measures were instituted in all health care facilities.7,8
In Portugal, the first 2 cases of coronavirus disease 2019 (COVID-19) were identified on March 2nd, 2020. Since then, in health care facilities, mask usage became mandatory and health-care professionals took measures toward minimizing the risk of transmission, such as enforcing hand hygiene policies, surface and environment cleaning, as well as assuring that minimum bed distancing was accomplished.
We aim to compare the benefits of systematic implementation of infection prevention and control measures, an indirect effect of COVID-19 pandemic, on the incidence of NI in patients admitted to a non-COVID-19 medical ward.
Methods
STUDY DESIGN AND PATIENT SELECTION
We performed a retrospective study analysis of all pa-tients admitted in a non-COVID-19 Internal Medicine ward, in a central hospital in Lisbon, Portugal (Centro Hospitalar Universitário de Lisboa Central), comparing the incidence of NI between a non-COVID-19 period (March-May 2019) and a COVID-19 period (March-May 2020).
We admitted March 2020 as the beginning of the COVID-19 period since it represents a time when the additional infection prevention and control transmission measures had already been implemented in our ward.
Infections were considered as nosocomial when occurred more than 48 hours after admission in the Internal Medicine ward. This assumption is possible since the time between hospital admission and ward admission can be considered irrelevant and equivalent between both periods (emergency room average length of stay was 0.7 days in the non-COVID-19 period and 0.4 days in the COVID-19 period).
Data was collected by assessment of the electronic me-dical records. No patients were excluded.
MEASURES IMPLEMENTED
The infection prevention and control measures implemented were:
The infection control committee promoted educational and training workshops about infection protective measures;
all environmental surfaces of our ward were consistently cleaned and disinfected with alcoholic or hypochlorite solution. The target surfaces were bedside tables, beds, desks and chairs, computer keyboards, computer mice, and telephones. Besides, all door handles, floor, and toilets of our ward were cleaned and disinfected regularly;
all healthcare professionals took additional protective precautions at every interaction with the patients, through reinforcement of the already implemented hand hygiene protocols (before and after every contact with the patients or the patients’ environment) and implemen-tation of droplet (P1 face mask wearing) and contact precautions (disposable nitrile or latex gloves and disposable gowns);
all medical equipment were properly disinfected after each utilization (stethoscope, blood pressure cuff, oximeter, or electronic thermometer);
all patients and healthcare professionals wore a P1 face mask while standing on the ward;
all healthcare professionals wore exclusive hospital uniforms;
routine patient visits have been suspended. Although there was no formal evaluation of its rate of compliance, there was a permanent link between the health care professionals and the hospital infection commission, with strong awareness of the importance of the implemented measures, and all professionals took them in their daily routine
DEFINITIONS
We considered nosocomial infection, using the CDC definition, as an infection occurring more than 48 hours after hospital admission. Hospital admission was considered as the moment in which patients were admitted in our Internal Medicine ward, since we could not guarantee that the implemented protective measures were the same in the other wards or in the emergency department and so, it would create a risk of bias in our results.
The presence of infection was considered in the presence of clinical deterioration, organ-specific signs and symptoms, elevation of inflammatory markers with or without microorganism isolation, resulting in the prescription of an antibiotic.
Multidrug resistant (MDR) microorganisms were defined as having non-susceptibility to at least one antimicrobial drug in three or more antimicrobial categories.
Chronic kidney disease was considered for glomerular filtration rates < 60 mL/min (stage 3-5).
Immunosuppressive drug therapy was considered when taken daily, by oral or intravenous route.
STATISTICAL ANALYSIS
The statistical analysis was performed with IBM® SPSS® Statistics version 26 for Windows. The normal distribution of continuous variables was tested using the Shapiro-Wilk test and by visual analysis of the histogram. The continuous variables with non-parametric distribution assessed are represented using median and interquartile range (IQR). A comparison between the categorical variables was made using the chi-squared test or the Fisher´s exact test as appropriate. A comparison between a categorical variable and a continuous variable with non-parametric distribution was made using the Mann-Whitney U test. All statistical tests were bilateral and with a 5% significance level. Binary logistic regression models with a 95% confidence interval were used to study effects of different variables on pretended outcomes (occurrence of nosocomial infection). The measures of association relative risk reduction (RRR) and number needed to treat (NNT) were used to assess the effect of the infection control measures in the nosocomial infections.
RESULTS
CHARACTERIZATION OF POPULATION
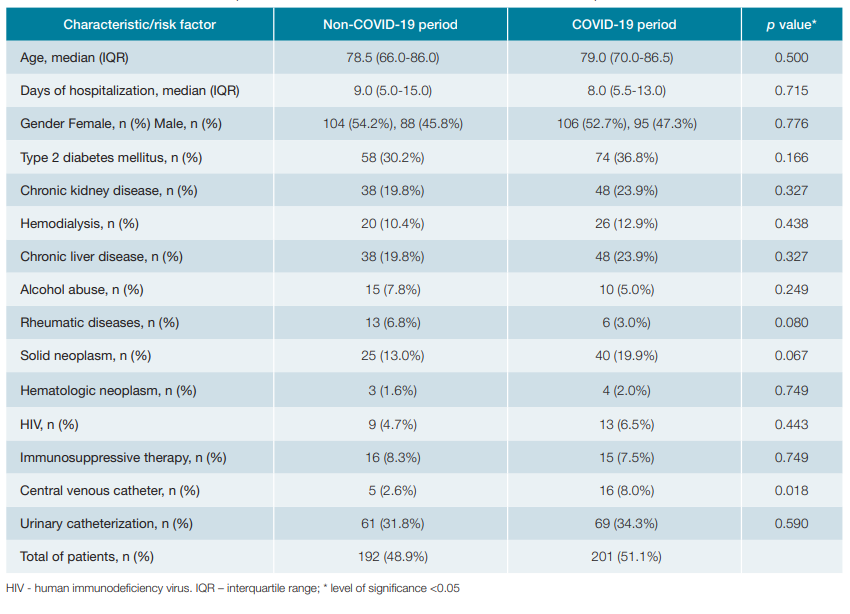
We analysed 393 patients, 192 patients being from the non-COVID-19 period and 201 patients from the COVID-19 period. The baseline characteristics are represented in table 1.
NOSOCOMIAL INFECTIONS
From the 393 included patients, 10.7% (n = 42) deve-loped a nosocomial infection. In the non-COVID-19 period, 31 patients (16.1%) had a nosocomial infection comparing with 11 patients (5.5%) in the COVID-19 period. These data showed a statistically significant reduction (p = 0.001; OR 0.301; 95% CI: 0.146-0.617). The infection control measu-res implemented were associated with a nosocomial infection RRR of 0.66 and a NNT of 9.
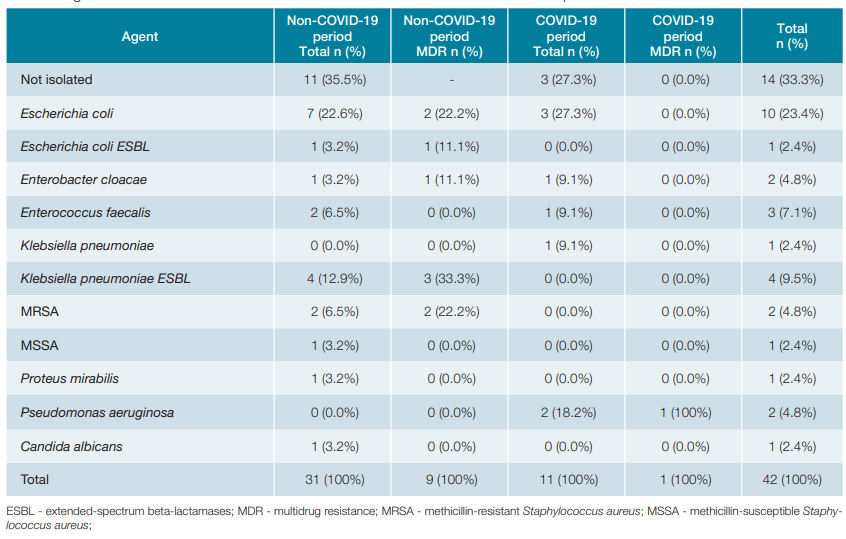
The types of nosocomial infection that occurred in our population are registered in Table 2. The most common were urinary (n = 23, 5.9%) and respiratory (n = 14, 3.6%) tract infections. Comparing the two periods, we obtained an ab-solute and relative reduction in urinary, respiratory, blood, and gastrointestinal tract infections. However, only nosocomial respiratory tract infections had a statistically significant reduction (n = 12; 6.3% vs n = 2; 1.0%; p = 0.005), The description of the agents implicated in NI and its classification as MDR microorganisms are represented in table 3. The most common isolated agents in the non-COVID-19 period were Escherichia coli (n = 7; 22.6%) and Klebsiella pneumoniae ESBL (n = 4; 12.9%), while Escherichia coli (n = 3; 27.3%) and Pseudomonas aeruginosa (n = 2; 18.2%) were the more frequent ones in the COVID-19 period. We found a statistically significant reduction on the incidence of MDR agents between the non-COVID-19 and the COVID-19 periods (n = 9; 29.0% vs n = 1; 9.1%; p = 0.009). The additional protective measures implemen-ted lead to a RRR of MDR infections of 0.89 and a NNT of 24.
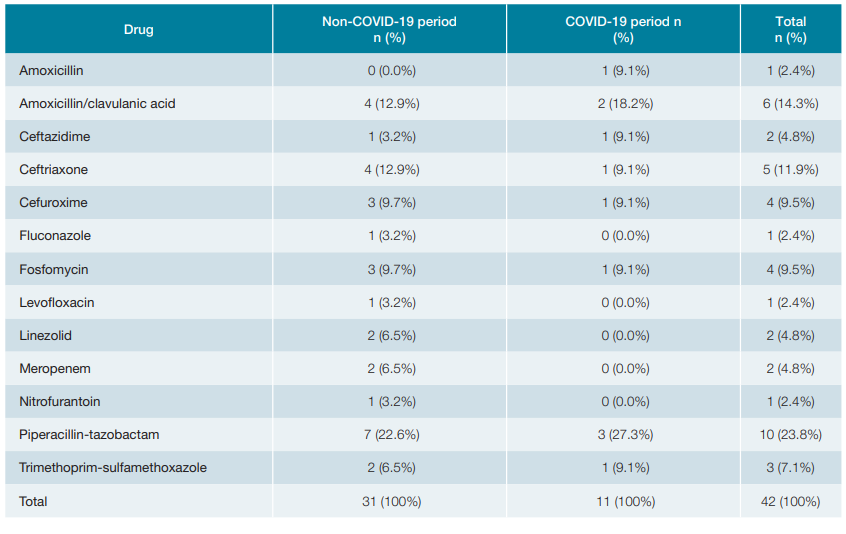
The detailed description of the prescribed drugs to treat NI is showed in Table 4. In the non-COVID-19 period, 31 patients (16.1%) were started on antibiotics for a nosocomial infection. The most used were piperacillintazobactam (n = 7; 22.6%) and amoxicillin/clavulanic acid (n = 4; 12.9%) and ceftriaxone (n = 4; 12.9%). In the COVID-19 period, 11 patients (5.5%) with NI were treated with antibiotics. The used drugs were similar to the ones used in the non-COVID-19 period, although with a less absolute frequency. As all NI were treated with antibiotics, the overall use of antibiotics was statistically significant lower in the COVID-19 period compared to the non-COVID-19 period (p= 0.001). From the 192 patients admitted in our ward in the non-COVID-19 period, 15 patients (7.8%) died. In the COVID-19 period (n = 201), death occurred in 32 patients (15.9%). The number of deaths by all causes occurred in the COVID-19 period was statistically significantly higher than in the non-COVID-19 period (p = 0.013).
Table 4: Prescribed drugs to treat patients with nosocomial infections in the non-COVID-19 and COVID-19 periods.
ADVERSE EFFECTS OF NOSOCOMIAL INFECTIONS
Patients with a nosocomial infection admitted in our ward on both periods had a median length of hospitalization of 21.0 (12.75-27.25) days, compared to 8.0 (5.0-12.0) days in those without a nosocomial infection. In both time periods, NI were statistically significant associated with a longer length of hospitalization (p < 0.001).
Considering both studied periods (n = 393), 33.1% of patients (n = 130) underwent urinary catheterization. Nosocomial urinary tract infection was diagnosed in 5.9% (n = 23) and among these patients, urinary catheterization was performed in 60.9% (n = 14). Urinary catheterization, independently of the period considered, had a statistically significant association with nosocomial urinary tract infection (p = 0.004; OR 3.406; 95% CI: 1.433-8.095).
Although central venous catheter placement was more fre-quent in the COVID-19 period (n = 16 vs n=5), the frequency of NI associated with its use was the same in both periods (n = 1), with no significance difference (p=1.000).
In both time periods, 14.3% (n = 6) patients with a fatal outcome had a nosocomial infection. However, there was no statistically significant association between having a nosocomial infection and death (p = 0.802).
Discussion
The overall NI prevalence comes in line with published data, being known that it ranges from 2.5% to 15%, regardless the type of ward or level of care considered.9-12Specific Internal Medicine prevalence data are scarce and direct comparisons cannot be made.
Our results show a decrease in the incidence of NI after systematic implementation of IPC protocols, from 16.1% in the non-COVID-19 period to 5.5% in the COVID-19 period, with one nosocomial infection evicted by each nine patients approached with such preventive measures, and a risk reduction of 1.5 times. These data confirm and underly the major importance of systematic implementation of preventive measures. Patients with occurrence of NI have prolonged length of stay in comparison with those free of such event. Also, such group exhibited a greater number of deaths during hospital stay, even though this difference had no significant statistical value.
Even though we report a statistically significant reduction in the global prevalence of NI, when analysing individual types of NI, we only validate a statistically significant reduction in respiratory tract infections (6.3% to 1%). We postulate that generalized professional mask usage may play a role in reducing the frequency of respiratory tract infections. Also, considering that all admitted patients wore masks during hospital stay, we claim that a reduction in patient-to-patient transmission may also be responsible for such reduction. On another hand, surface cleaning leads to a safer environment that can play a role in reduction oropharynx colonization by nosocomial agents that eventually would lead to infection.
When specifically analyzing nosocomial urinary tract infec-tions (UTI), another factor comes into discussion. Our data show a non-significant (p = 0.106) reduction from 15 to 8 cases (7.8% to 4.0%). Looking at both COVID-19 and non-COVID-19 periods, we report use of urinary catheter in 33.1%(n = 130) patients. Also, in both periods, there were 23 cases of UTI, of which 14 occurred in patients who underwent urinary catheterization. This difference in frequency demonstrated a statistically significant value, with a marked association (OR = 3.4) between the presence of urinary catheter and the development of UTI. The urinary catheter bias can justify the absence of statistically significant reduction in the frequency of UTI as it concurs for and increases UTI occurrence. Despite such limitation, the confirmation of the well-known association between urinary catheterization and UTI development underlies the importance of strict criteria when using such device and proactive daily evaluation of its maintenance to further reduce UTI in Internal Medicine and other wards.13 IPC protocols also focus on management of external devices, including urinary catheters. Although our rate of urinary catheter use might be considered high (33.1%), in our hospital there is a commission for the control of catheter associated UTI that focus on assuring that its use follows strict indications and that it is removed as soon as possible.
Although we cannot statistically corroborate the reduction in the remaining NI, probably due to its low number, every type of infection showed at least no increase in frequency in the COVID-19 period.
We report a statistically significant reduction in antibiotic use in the COVID-19 period consistent with the reduction in the frequency of NI. Such antibiotic usage reduction adds value to the global scenario, being a useful tool to reducing bacterial selection and, consequently, antibiotic resistance and improving personal and global outcomes.14 We also found a statistically significant reduction in the incidence of NI by MDR agents, from 29.0% in the non-COVID-19 period to 9.1% in the COVID-19 period, with one MDR microorganism infection prevented by each 24 patients approached with those preventive measures. Even though the MDR profile of an institution reflects global longitudinal policies, we postulate that the observed reduction in MDR nosocomial infections comes as a result of IPC protocols implemented and it is an added value in terms of patients’ outcome, broad-spectrum antibiotic sparing, and global hospital costs.
Although we report a reduction in the number of NI in the COVID-19 period, our data show a higher frequency of deaths in such period, in line with previous published data.15,16This significant increase of mortality rate (7.8% to 15.9%) is not associated with the occurrence of NI, as in both periods there was no statistically significant relationship between the two variables. During the pandemic, there was a subjective feeling that patients may be experiencing fear and anxiety of looking for hospital care, fact we postulate to be responsible for a delay in timing of admission and consequent worse admission status, aggravated associated prognosis, and even death. Another fact that may be responsible for such increase of this adverse outcome may be the forced reduction in programmed activity of the outpatient clinics, which are moments of major importance in the management of patients with chronic conditions and early detection of decompensation. We postulate that the significant increase in central venous catheter usage also occurred because of worse clinical baseline status of COVID-19 period patients.
LIMITATIONS
We were able to identify some limitations in our work. Being an unicenter study, our results may not be applicable to other hospital realities. Besides, being an observational study and because the collected and analysed data were obtained from electronic medical records there is a possibility that information is lacking. Finally, there is no implemented systematic screening for MDR such as carbapenamase-producing enterobacteriaceae or methicillin-resistant Staphylococcus aureus. Such implementation could strengthen our data interpretation and help reducing NI.
Conclusion
We confirm a reduction in the occurrence of NI after implementation of systematic infection control protocols to prevent SARS-CoV-2 transmission. Such reduction may have long term benefits in either economic factors, clinical outcome, or social impact of hospitalization. Further investigation to validate our data and cost-benefit analysis should be performed in order to clarify if universal implementation of our infection prevention and control measures could bring up value in the management of all patients. Such questions could be answered in a prospective multicenter study.