Introduction
Delirium is one of the most frequent neuropsychiatric com-plications not only in critically ill patients, where it is traditionally discussed, but also in the context of palliative care. Despite the recognition of its existence, it was vaguely described until the 1990s, when the formal definition appears in the fourth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM).1 Currently, and according to the fifth edition of the DSM, delirium is a complex clinical syndrome that arises in the context of acute neurological dysfunction, characterized by a disturbance of attention, cognition, perception, and orientation over a short period of time with fluctuating severity during the course of a day.2 This definition overlaps with the one established by the World Health Organization in the 11th edition of the International Classification of Diseases (ICD-11), where components of the sleep-wake cycle are added, such as reduced arousal of acute onset or total sleep loss with reversal of the sleep-wake cycle.3
From this definition, three subtypes of delirium were described according to the type of psychomotor activity: hyperactive, hypoactive, and mixed delirium.4 Hyperactive delirium, characterized by restlessness, agitation, hallucinations, and refusal to cooperate with care, is the most easily identified, but it corresponds to only 25% of cases. The remaining percentage of patients with delirium show characteristics of hypoactive delirium5 with prostration, speech slowness, and apathy or with overlapping characteristics of hyper and hypoactivity, configuring a mixed delirium.6 Precisely because it is more difficult to diagnose and often confused with fatigue, depression, or dementia,2 hypoactive delirium is associated with a worse prognosis.
Although its pathophysiology is not yet fully understood, its etiology is usually multifactorial and each individual with delirium has a unique set of underlying causes that contribute to the symptoms,1 a situation that is invariable in advanced disease in the context of palliative care. Advanced age, existence of critical illness, low functionality, and the presence of cognitive, visual or auditory disturbances are described as predisposing risk factors.7 Precipitating risk factors for delirium7 include polymedication, the load of anticholinergics, drug intoxication, the presence of catheters, infection, dehydration, ionic changes such as hyponatremia and hypercalcemia, hypoxia, endocrine and metabolic disorders, organ dysfunction, paraneoplastic syndromes and the physical restraint itself.8
Little information is available on delirium in palliative care. Studies point to a prevalence of delirium of 8.4% in inpatient palliative care, increasing to 35% when delirium and/or descriptions suggestive of delirium are considered9 and up to 88% in the hours to days preceding the end of life.10 Data on delirium in the follow-up of patients in palliative care at home are even more scarce and, despite being well described, this condition is still poorly recognized and treated in a less structured way.5 In addition to its high prevalence, delirium plays a significant role in health care1 and its diagnosis should be valued as a predictor of poor prognosis and addressed to identify and correct potentially reversible factors.
This work aims to expand the existing information on delirium in palliative care both in-hospital and at home.
Our objective was to characterize the population followed by the Palliative Care Team of the Local Health Unit of Matosinhos (ECP-ULSM) in the hospital and at home and to assess the prevalence of delirium in these patients, the factors associated with it, the therapeutic strategy used and the time of resolution.
Material and Methods
A retrospective cohort study that included all patients referred and followed up by the ECP-ULSM in-hospital and at home between January 1st and December 31st, 2019. The necessary information was obtained by consulting the electronic medical record. The study was carried out in line with the recommendations of the Declaration of Helsinki of the World Medical Association. All data was anonymized and being a retrospective analysis of deceased patients, consent has been waived. The development or not of delirium or suggestive symptoms such as memory deficit, apathy, hallucinations, mood disturbances, fluctuation in the state of consciousness, persistent agitation6 and delirium prodromes such as changes in the sleep-wake cycle, irritability, and anxiety were recorded. Delirium was assumed whenever it had been identified as a problem in the palliative care team's records - no formal scale was used. The presence of predisposing factors and the presence of precipitating factors such as the existence of neoplasm or brain metastases, the use of drugs such as benzodiazepines, opioids, anticholinergics, quinolones and corticosteroids, ionic and endocrine changes - namely in blood glucose or thyroid function - were also recorded. In addition, information was collected on medication implemented for first and second line management of delirium, on its resolution, and time to resolution.
STATISTICAL ANALYSIS
Statistical analysis was performed using SPSS® software, version 23 (IBM, Armonk, NY). Except for age (continuous va-riable) which is presented as mean +/- standard deviation, all other variables are categorical and, therefore, are presented as frequencies and percentages. The presence of association between categorical variables was analyzed using the Chi-square or Fisher test and the student’s t test or the Mann-Whitney test was used to analyze continuous variables, following or not the normal distribution, respectively. Multivariate analysis consisted of binary logistic regression, including all variables associated with statistically significant differences in univariate analysis. A statistically significant difference was considered whenever the test value (p-value, p) did not exceed the 5% significance level (p <0.05). Confidence intervals of 95% were used.
Results
DESCRIPTION OF THE POPULATION, PHARMACOLOGICAL TREATMENT, AND OUTCOMES
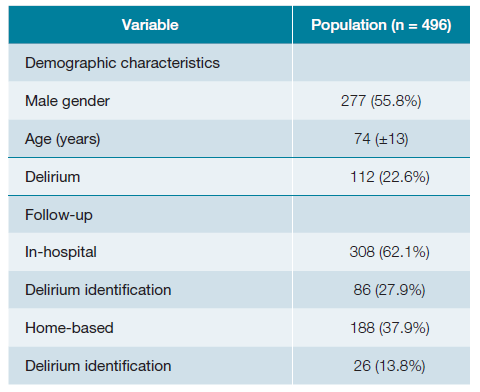
A total of 496 patients were included, 277 (55.8%) of whom were male, with a mean age of 74 (±13) years. Of these, 308 (62.1%) patients were followed up in the hospital and 188 (37.9%) were followed up at home. Delirium was identified in a total of 112 (22.6%) patients as described in Table 1.
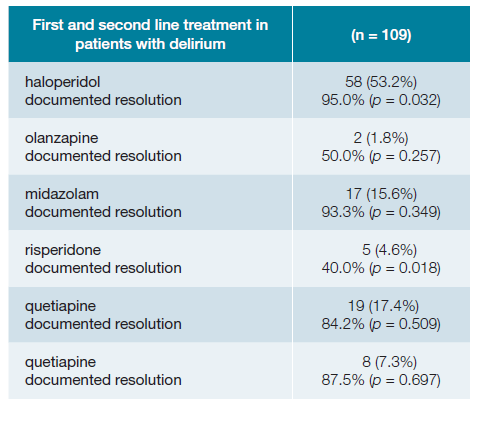
As for the pharmacological treatment of delirium, as shown in Table 2, the use of haloperidol, olanzapine, midazolam, risperidone and quetiapine as first and second line drugs was studied. The most commonly used first line drug was haloperidol (n = 58, 53.2%) with a statistically significant difference in the resolution of delirium (95.0%, p = 0.032). The drug that showed the lowest resolution was risperidone (40.0%, p = 0.018).
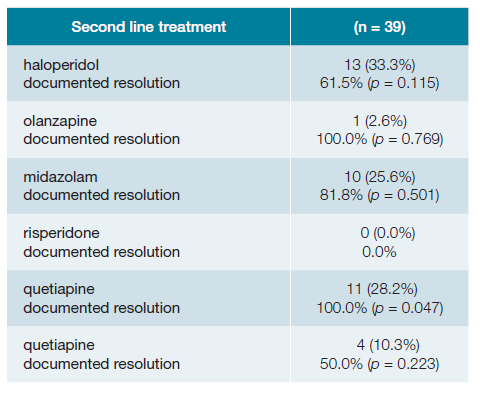
From the population of 109 patients in whom delirium was identified and pharmacologically treated, resolution was documented in a total of 98 (89.9%) patients, the majority of those in less than 5 days (n = 80, 81.6%), with 39 (35.8%) patients requiring a second line drug. Table 3 describes the second line drugs used. The most chosen second line drug was haloperidol (n = 13, 33.3%), followed by quetiapine (n = 11, 28.2%) which showed higher resolution as a second line drug (100.0%, p = 0.047) as can be seen in Table 3. There were no statistically significant differences between the use of a given pharmacological treatment and the time of resolution both in first line (haloperidol p = 0.289) and second line (quetiapine p = 0.573) therapy.
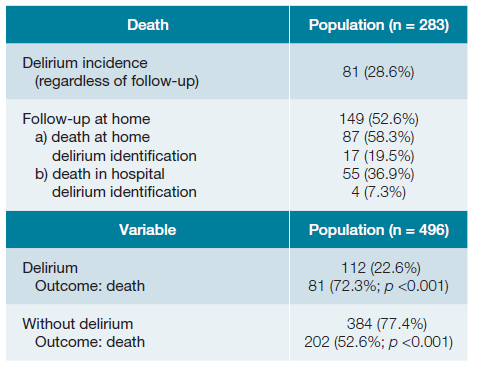
A total of 283 (57.1%) patients died, of whom 81 (28.6%) developed delirium. The occurrence of death was significantly higher in patients who developed delirium, compared to those who did not (72.3% vs 52.6%; p <0.001). Of the patients evaluated at home and who died in 2019 (149 patients), 55 (36.9%) died in the hospital and 87 (58.3%) died at home. The prevalence of delirium was higher in patients who died at home (19.5%) compared to those who died in the hospital (7.3%).
VARIABLES THAT INFLUENCE THE PRESENCE OF DELIRIUM
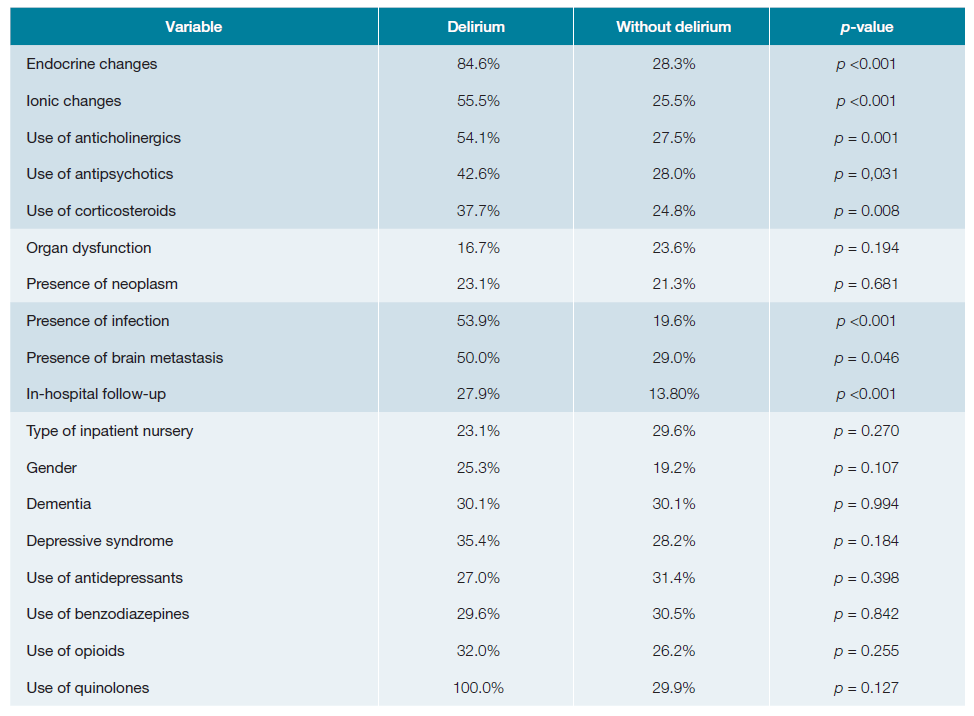
From all the 496 patients included in the study, the va-riables previously identified as precipitating risk factors were studied, and the following were significantly associated with a higher incidence of delirium: in-hospital follow-up (27.9% vs 13.8%; p <0.001), infection (53.9% vs 19.6%; p <0.001), endocrine changes (84.6% vs 28.3%; p <0.001), ionic changes (55.0% vs 25.5%; p <0.001), antipsychotics (42.6% vs 28.0%; p = 0.031), corticosteroid therapy (37.7% vs 24.8%; p = 0.008), use of anticholinergics (54.1% vs 27 .5%; p = 0.001), presence of brain metastasis (50.0% vs 29.0%; p = 0.046). None of the other variables studied showed statistically significant differences.
PREDICTORS OF DELIRIUM
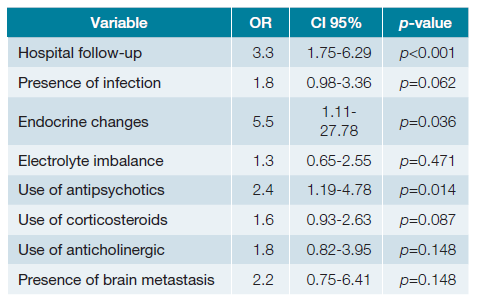
In a multivariate analysis, to adjust for confounding factors, in-hospital follow-up (OR=3.30; 95%CI = 1.75-6.29, p <0.001), the existence of endocrine changes (OR=5.50; 95%CI=1.11-27.78, p = 0.036) and the use of antipsychotics (OR=2.38; 95%CI=1.19-4.78, p = 0.014) were associated with a higher incidence of delirium.
Discussion
DELIRIUM IDENTIFICATION
Delirium is frequently associated with precipitating events that are often reversible, such as infection, dehydration and ionic changes superimposed on underlying vulnerability in the context of advanced disease,11 which is why it is extremely important to look for and identify these changes. This premise is valid not only in an inpatient context, but also in home follow-up. By allowing the family to identify symptoms suggestive of delirium, early recognition and treatment by the care team are possible, avoiding the need for emergency services and possible hospitalization. Of the 188 patients followed at home, delirium was identified in 26 (13.8%) patients, a value significantly lower than that identified in the in-hospital regimen (27.9%), and which was mostly managed at home.
In the 112 patients diagnosed with delirium, some factors were found to be associated with a higher incidence of this problem, such as: in-hospital follow-up (OR=3.30; 95%CI=1.75-6.29, p <0.001), which may be overestimated since difficult-to-manage delirium or terminal restlessness may be the reason for hospitalization or because it is more easily identified by the various health professionals; the existence of identified and corrected endocrine changes (OR=5.50; 95%CI=1.11-27.78, p = 0.036); and the use of antipsychotics (OR=2.38; 95%CI=1.19 -4.78, p = 0.014), possibly due to the presence of patients with prior changes in behavior that were medicated with these drugs.
DELIRIUM TREATMENT
Patients may be agitated without delirium (i.e., without disturbances of consciousness or cognition) for a variety of reasons, such as fecal impaction, urinary retention, uncontrolled pain or drug-induced akathisia, so it is important to know the diagnostic criteria for delirium and address any possible confounding factors.12 For this reason, not all patients with delirium (n = 112) underwent pharmacological therapeutic intervention (n = 109).
There is little research on non-pharmacological prevention and only a limited number of trials on pharmacological therapy in delirium.13 Thus, evidence for the use of antipsychotics in the treatment of delirium is also quite limited and the existing literature is often contradictory. A Cochrane review by Anne M. Finucane et al on drug therapy for delirium in terminally ill patients concluded that, based on this one study and with a small sample size, haloperidol is the most suitable drug for the treatment of patients with end-of-life delirium, with chlorpromazine being an acceptable alternative.14 The National Institute for Health and Care Excellence (NICE) guidelines15 recommend the use of haloperidol if the patient poses a danger to himself or others when non-pharmacological interventions have failed. In contrast, the European Society for Medical Oncology (ESMO)16 guidelines advise against the use of haloperidol and risperidone in cancer patients with end-of-life delirium, although there is some evidence of benefit in the use of olanzapine and quetiapine.
Of all the drugs studied, the most used was haloperidol (53.2%), perhaps because of the ease of administration in the hospital environment (intramuscular route) and at home (orally) and because of the team's own experience. However, in this sample, the data presented show greater resolution associated with the use of haloperidol, which is why it was also the drug of choice in a greater number of second line cases (33.3%). There may be a role for quetiapine as a second line drug, since it was associated with resolution of delirium 100.0% of the cases with a statistically significant difference (p = 0.047), which is in agreement with the existing literature described above.14-16
Despite this, it must be taken into account that non-pharmacological measures and the prevention of delirium come first, and the use of drugs should be reserved for cases where prevention has not been effective and where non-pharmacological therapy has failed.
The main goal of delirium management in the context of palliative care, given its poor prognosis, should be to prioritize the comfort of the patient,2 the tranquility of the care team and the informed involvement of family members and caregivers.
RESOLUTION OF DELIRIUM
According to the literature,17 the duration of delirium can vary widely, from a few days - in most patients - to weeks or months. In the latter case, the diagnosis of persistent delirium is assumed. The more effective the prevention and the earlier the diagnosis, the easier and faster the resolution. Although not using a standard scale, delirium was described as solved in most patients observed by ECP-ULSM in less than 5 days. However, in the study population, the use of the above-mentioned drugs did not influence the time to resolution of delirium in patients treated in the hospital or at home.
DELIRIUM AS A PREDICTOR OF DEATH
In palliative care, delirium is interpreted as a sign of imminent death and, in this context, the anguish felt by patients, family members and caregivers is generally aggravated by the difficulty in communication and the difficulty controlling behavioral changes.18 This premise is described in terminal patients in days to weeks, mainly in those diagnosed with advanced cancer2 in palliative care units and in hospice facilities.
Hospital mortality of elderly people with delirium ranges from 22% to 76%.19 Consistent with this evidence, the outcome of death was also higher in patients who developed delirium compared to those who did not, with statistical significance (72.3% vs 52.6%; p <0.001).
Despite the confirmation of delirium as a predictor of death, this does not mean that death will occur in the hospital. Of all the patients followed at home and who died, the identification of delirium was higher in those who died at home (19.5%) compared to those who died in the hospital (7.3%). We must note that for this study it was also included suggestive symptoms of delirium. In the end of life can be very challenging for the home-care palliative team the interpretation given by the family. But with the early identification of this disorder and the involvement of the family in its management, it was possible for the patient with delirium to followed at home to die at home.
LIMITATIONS
Despite presenting and studying a significant sample of patients (n = 496), the diagnosis of delirium was not applied according to standardized scales for this purpose, but rather assumed based on the records made by the ECP-ULSM, so there is an assumed identification bias. Underdiagnosis of hypoactive delirium and overdiagnosis of hyperactive delirium are also assumed, the latter tending to be more recognized in general wards and aggravated by the greater use of physical restraint measures and the more frequent use of haloperidol in this context.
Conclusion
This study demonstrates the non-negligible prevalence of delirium in end-of-life patients, especially in an in-hospital context, as well as its secondary causes and its value as a predictor of poor prognosis. Due to the multifactorial nature of delirium in the context of palliative care, a multidisciplinary approach that can predict and correct its precipitating factors, as well as the early implementation of quality home and in-hospital palliative care at the end of life, may provide more effective control of delirium and reducing its overall prevalence.