Introduction
Digitalization in healthcare is an inevitable reality and it is set to become an integral part of the future of clinical practice, namely in Internal Medicine. The tangible integration of existing digital technologies into healthcare delivery has become increasingly evident; such increase has been driven by its fast adoption during the global pandemic crisis. Within the intricate network of healthcare systems, substantial challenges remain, including issues of accessibility, regulation of access and sustainability of healthcare services. These challenges, far from being unsolvable barriers, can be seen as opportunities for systemic transformations. The proposal shared here aims to directly tackle these challenges by introducing an innovative technology-driven approach to healthcare provision. It seeks not only to proactively adapt to the changing healthcare landscape, but also to actively shape a paradigm in which healthcare is more accessible, patient-centered and resilient in the face of unexpected challenges that may appear. This approach aims not only to meet present needs, but also to anticipate and respond effectively to future healthcare demands.
The transformation of healthcare provision through Digital Health is supported by several lines of evolution, each representing a significant advance on the traditional paradigm. The proposal outlined for the ULS-Braga is strategically aligned with three lines of evolution, aiming to incorporate the digital transition in a comprehensive way. Next, we will explore each component of the strategy in more detail and examine how other institutions have achieved remarkable results through similar approaches.
Line Of Evolution 1: The Responsibility Of The Person (Healthy And Sick).
The importance of the patient's role in managing their own health is a global trend that transcends borders and influences innovative health systems in various parts of the world. The concept of the "responsible patient" has been a fundamental foundation for innovative healthcare systems. In Denmark, patient-centered programs have been developed, encouraging self-management of chronic diseases; the Danish patient empowerment program "Patient Empower" has shown remarkable improvements in patients' adherence to treatment and their quality of life.1 In the UK, initiatives such as the “Expert Patient Program” have provided patients with the tools and knowledge they need to take an active role in their treatment, resulting in significant improvements in self-efficacy and a reduction in complications related to chronic diseases.2 The "responsible patient" approach goes beyond self-management of chronic conditions, expanding to health promotion in general. In Singapore, programs such as the "Health Promotion Board" encourage the active participation of citizens in promoting healthy lifestyles, promoting conscious choices and preventing health conditions before they even develop.3 In Australia, the focus on health self-management is evidenced by the "Chronic Disease Self-Management Program", a program that provides Australians with practical tools and strategies to manage their health conditions, resulting in measurable improvements in quality of life and cost savings for the health system.4 In the United States, the growing emphasis on active patient participation is evident in initiatives such as the “Patient-Centered Medical Home (PCMH)”, which encourages collaboration between patients, clinicians and healthcare teams to achieve better health outcomes, especially in populations with chronic diseases.5
When considering the implementation of a "responsible patient" model in the ULS-Braga, it is crucial to adapt global strategies to local dynamics. The approach must be sensitive to the characteristics of the community, promoting patient autonomy, incorporating cultural diversity and considering the particularities of the Portuguese health system, thus resulting in tangible health benefits for the local community.
Evolution Line 2: Care Anywhere
The evolution towards an out-of-hospital approach to healthcare represents a significant milestone in the search for more accessible, patient-centered services.
Taking the example from Israel's innovative practices, especially the "Care Anywhere" program, it is possible to further explore the implications and benefits of this global transformation.6 The "Care Anywhere" approach in Israel finds resonance in many parts of the world, where similar initiatives have played a crucial role in responding to the growing demands for more flexible and accessible health services. In Sweden, for example, the "Digital Healthcare Visits" program has enabled patients to receive virtual doctor visits, increasing the efficiency of the system and reducing geographical barriers to obtaining medical care.7
The emphasis on taking healthcare beyond hospital facilities is also visible in the United States, where telemedicine has become an essential tool for expanding access to healthcare services. Programs such as "Project ECHO" connect specialists to patients in remote areas, promoting interdisciplinary collaboration and ensuring that high-quality medical knowledge is available in places previously considered inaccessible.8 The successful implementation of out-of-hospital care is also seen in India, where initiatives such as "mHealth" leverage smartphone dissemination to provide remote healthcare and virtual consultations; this approach has proven particularly effective in rural areas, where accessibility to healthcare services has historically been limited.9
When contemplating the transformation of care in non-hospital settings for the ULS-Braga, it is essential to consider the technological infrastructure, community acceptance and integration with local health systems. Adaptable and innovative strategies can include the implementation of virtual consultations, telemedicine programs and partnerships with local healthcare providers, in this case, with the Association P5 Digital Medical Center (P5), to bring care to communities. Global experience highlights that expanding care beyond traditional borders not only improves accessibility, but also promotes efficiency and continuity of health services. By incorporating these global practices and customizing them to Braga's specific reality, the Hospital can position itself as a leader in providing innovative, patient-centered care.
Evolution Line 3: The Evolution of Digital Health
The evolution of Digital Health is a global phenomenon that has radically transformed the provision of care. Estonia is a remarkable example of a nation that has embraced Digital Health in a comprehensive way. This Baltic country has successfully implemented electronic and interoperable health records for all citizens, resulting in significant efficiency in care, a reduction in medical errors and a more proactive approach to preventative healthcare.10,11By implementing electronic health records for the entire population, Estonia has not only embraced Digital Health, but has also set a standard for efficiency and innovation in healthcare management. Similar experiences can be observed in Finland, where the "Kanta" system provides an integrated and accessible approach to electronic health records, promoting continuity of care and the efficient exchange of information between healthcare professionals.12 Global initiatives, such as the use of blockchain in health record management, are being explored in countries such as Switzerland, with the aim of further increasing the security and interoperability of health data.13
Estonia's proactive approach to preventive health is a crucial aspect of digital health. The implementation of electronic records allows for a more comprehensive analysis of population health data, identifying patterns and areas for intervention even before significant clinical problems arise. This is in line with initiatives in other countries, such as the UK, which uses artificial intelligence to predict and prevent diseases at an early stage.14 However, the evolution of Digital Health does not end with the implementation of electronic records; it is intrinsically linked to continuous innovations. Noteworthy in this context are symptomchecker systems in digital health, which offer several advantages for both users and healthcare professionals, with increasing implementation and positive results, especially when properly framed with complementary support from healthcare professionals prepared to operate in the field of remote healthcare.15,16
When considering the incorporation of Digital Health ap-proaches in the ULS-Braga, it is essential to evaluate the technological infrastructure, the needs of the population served and the regulatory requirements. Adaptable strategies can, and should, be developed, such as the integration of telemedicine, healthcare applications and efficient interoperability, so that a more integrated and effective approach to local healthcare is enabled; notwithstanding, it is also crucial to develop strategies that considers the ethical challenges related to security and acceptance, in order to ensure a successful and sustainable implementation.
Pilot Study for Remote Monitoring and Follow-up of Heart Failure Patients
An innovative model for remote monitoring and follow-up of heart failure patients was developed in a collaboration between ULS-Braga (Internal Medicine Consultation of Heart Failure) and P5. This remote monitoring model (Fig. 1) represents an integrated approach to the outpatient management of chronic heart disease, and is described below, in its different phases, highlighting its scientific foundations, implications and benefits.
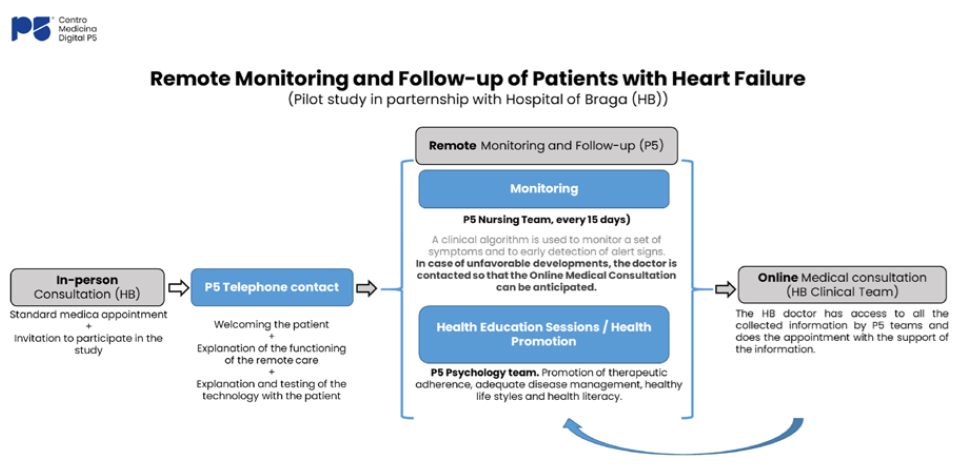
Figure 1: Schematic of the functioning of the pilot study of remote monitoring and follow-up of patients with heart failure at ULS-Braga and P5.
Initial Phase: Invitation and Welcome: The invitation to participate in the study is the starting point for a personalized care experience. Previous studies indicate that effective communication and active patient participation at the onset are associated with better clinical outcomes.17 The telephone contact made by P5 Team, not only provides an appropriate reception to the program, but also establishes an essential human connection. During this interaction, the detailed explanation of remote monitoring emphasizes the importance of active patient involvement. Practical tests ensure that patients are comfortable and confident in using the digital tools, promoting adherence from the onset.
Detailed Remote Monitoring: Regular video call sessions with the P5 nursing team (every 15 days) form the core of remote monitoring. Holding regular video call sessions for remote monitoring is in line with the recommendations for the management of Heart Failure.18 During these interactions, a detailed approach to specific heart failure symptoms, such as weight, blood pressure and edema, allows for a comprehensive assessment of health status. Early detection of warning signs allows for immediate and personalized interventions, resulting in more effective and preventive management of the disease, since early detection of symptoms and immediate intervention are key strategies for preventing hospitalizations and improving quality of life.18
Involvement of the Psychology Team: The inclusion of video call sessions with the P5 Psychology Team highlights the holistic commitment to patient well-being. These sessions not only address aspects such as adherence to treatment and knowledge of the disease, but also explore vital topics such as disease management, healthy lifestyles and health literacy promotion. This psychological support strengthens the patient's resilience and ability to effectively manage their heart failure. The literature suggests that psychological support can positively influence adherence to treatment and quality of life in patients with heart failure.19
Integrated Online Medical Consultation: The online medical consultation phase represents the convergence of all the information collected by the P5 Teams with hospital team that follows the patient. By having real-time access to vital and contextualized data, the physician can carry out a more efficient and personalized consultation. The convergence of information during the online medical consultation is in line with the growing trend towards data integration for informed clinical decisions. Studies highlight the usefulness of telemedicine in the treatment of heart failure, especially when based on real-time data.20 This approach ensures that clinical decisions are based on a comprehensive understanding of the patient's state of health, enabling a targeted response to specific needs.
Anticipating Follow-up in the Event of an Unfavourable Outcome: The ability to anticipate follow-up in the event of an unfavourable outcome highlights the proactive nature of this model. If the data indicates worrying changes, immedia-te intervention is activated. This approach not only prevents complications, but also sets a standard for preventive care, enabling better long-term results. The ability to anticipate follow-up in cases of unfavourable outcome reflects a proactive strategy, in line with the preventive approach increasingly valued in the management of chronic conditions, including heart failure.21
The international validation of this model is evident in experiences such as the "Telemonitoring in Heart Failure" program in the United Kingdom. The reduction in hospitalizations and improvement in the quality of life of heart failure patients indicate the effectiveness of this innovative approach.18 By adapting these international best practices to the specific context of ULS-Braga, this model not only redefines the standards of care for heart failure, but also places the patient at the center of an integrated and compassionate approach, driven by digital technology.
In this pilot study, 12 participants have been recruited so far. The evaluation of the pilot program confirms a positive experience, both for the participants and their families, as well as for the health professionals (Fig. 2).
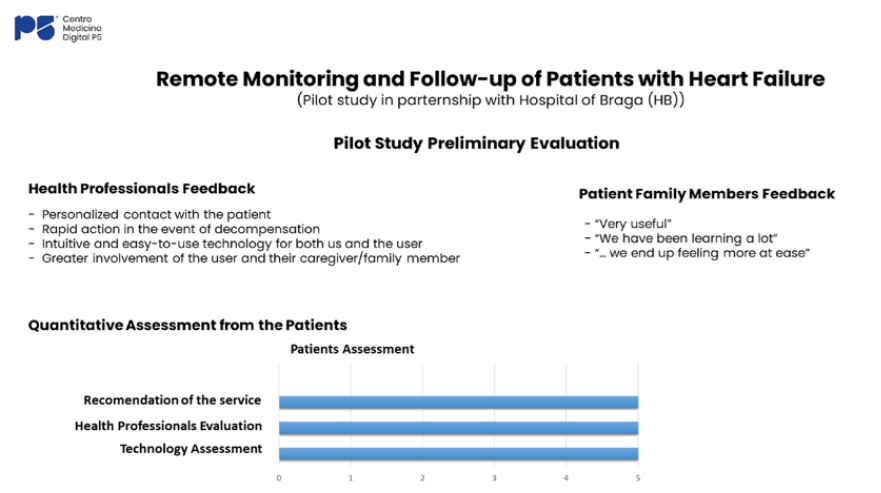
Figure 2: Results of a preliminary evaluation of the users of the pilot study of remote monitoring and follow-up of patients with heart failure at ULS-Braga and P5.
The participants, beyond their quantitative evaluation, show not only satisfaction, but genuine appreciation for the professionals involved in the program. The highlight goes to the personalized and caring approach of the health professionals. The technology used in the program also receives positive reviews, with participants emphasizing its effectiveness and ease of use. The enthusiastic recommendation to adopt this methodology for other individuals indicates not only acceptance, but belief in the transformative value of this approach.
Health professionals, for their part, emphasize key elements that contributed to the program's success. The personalized contact established with patients, where the professional-patient relationship transcended traditional boundaries, resulting in a more meaningful interaction was highlighted. A prompt and effective response to potential decompensations was also valued by healthcare professionals, as well as technology designed to be intuitive and easy to use, which facilitates the work and promotes more effective participation on the part of patients.
Family members, who play a crucial role in the process, express an extremely positive view of the program. They describe it as "very useful", which highlights the practical usefulness perceived by family members, who not only observe, but actively participate in the management of the disease of their family members. The emphasis that they learned a lot from the experience indicates a valuable educational dimension, promoting a deeper understanding of the condition and of the care process. In addition, the feeling of greater tranquillity and security shows not only the clinical effectiveness, but also the positive emotional impact that the program had on family members, relieving worries and promoting a safer and more comfortable environment.
The widespread satisfaction, along with the perceived benefits for all parties involved, validates the success of the program and suggests a promising path for future approaches in healthcare provision.
Also noteworthy were the results of the thematic sessions designed to educate participants about heart failure, which went beyond simply disseminating information and served as interactive platforms, fostering a dynamic exchange of knowledge and experiences. The comprehensive overview of heart failure gave participants a better understanding of the disease, empowering them to recognize and act upon symptoms that require vigilant attention, raising awareness and giving them the knowledge for timely self-assessment. In addition, exploring associated conditions, such as sleep apnea and chronic obstructive pulmonary disease (COPD), demonstrates the holistic approach to health and recognizes the interconnected nature of health problems by ensuring that participants are informed not only about heart failure, but also about potential contributing factors and comorbidities. This comprehensive understanding allows for a more proactive and preventative approach. The active participation of all individuals in these thematic sessions indicates a positive perception of the educational components of the program. This involvement is a key indicator of the program’s success in promoting a sense of health literacy and empowerment among participants. In short, the impact of these programs is reflected not only in the numbers, but also in the qualitative improvement in participants’ understanding of heart failure and related health considerations.
The consideration of scalability in the proposed model echoes the Swiss experience, where successful digital solutions have not only been replicated, but adapted and expanded to different specialties and regions, solidifying the benefits achieved.22 The scalability approach is not limited to physical expansion, but also relates to the adaptability of the model to the specific requirements and realities of ULS-Braga. A digital transformation must be accompanied by a continuous assessment of feasibility and local impact, which involves not just reproducing technologies, but incorporating continuous feed-back and adapting as necessary. Continuous commitment to improvement and innovation, along with a flexible and adaptive approach, will be key to maximizing the project’s benefits.
In conclusion, ULS-Braga’s pilot project proposal, which shows indicators of being successful, reflects an informed approach, based on successful experiences focusing on the digital transition of healthcare that are taking place around the world. By learning from global contexts and integrating these lessons at a local level, the proposal demonstrates a deep understanding of the dynamics involved in the digital transformation of healthcare. The search for scalability is not only aimed at expansion, but also sustainability and positive impact at a local level, solidifying the hospital’s commitment to innovation and excellence in healthcare delivery.















