Serviços Personalizados
Journal
Artigo
Indicadores
Links relacionados
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. v.17 n.1 Lisboa jan. 2010
Anorectal Melanoma
Melanoma Anorectal
Bruno Arroja1, Manuela Canhoto1, Cláudia Gonçalves1, Filipe Silva1, Isabel Cotrim1, Helena Vasconcelos1, Fernanda Cunha2
1Department of Gastroenterology, Hospital de Santo André EPE, Leiria, Portugal;
2Department of Pathology, Hospital de Santo André EPE, Leiria, Portugal; Hospital de Santo André, EPE, Leiria
INTRODUCTION
Primary anorectal melanoma is a rare condition accounting for 0,2-3% of all melanomas and approximately 1% of cancers afflicting this particular area1.
The mean survival time after diagnosis is 24 months and only 10% of all patients will be alive at 5 years. Nearly 60% of patients present with metastatic disease2.
The most frequent presentation symptom is rectal bleeding followed by change in defecatory habits1-5.
Albeit the large majority of anorectal melanomas have evident gross or microscopic pigmentation there are 30% of which are amelanotic4.
Currently abdomino-perineal resection with bilateral inguinal lymphadenectomy remains the first option procedure especially in large or obstructing lesions1-3,5.
CASE DESCRIPTION
A 77-year old female living in a nursing home with Alzheimers, diabetes and hypertension was referred to the Gastroenterology Department for a large prolapsed anorectal mass in December of 2007.
Three months previously the patient had undergone a left-sided colonoscopy performed outside the hospital after persistent rectal bleeding had ensued. A sessile polyp with 1 cm was then registered in the distal rectum.
Our physical examination identified a polypoid, prolapsed, pedunculated and mobile mass with white coloured areas alternating with necrotic ones, measuring 4-5 cm in diameter.
Laboratory data was: hematocrit 29,2%; platelet count 367,6 x10^3/μl; INR 1,09; aPTT 24,2 seconds.
Total colonoscopy did not detect further lesions along the remaining colon.
The lesion was almost completely excised by fragmentation using a large polipectomy snare (Fig. 1a, 1b).
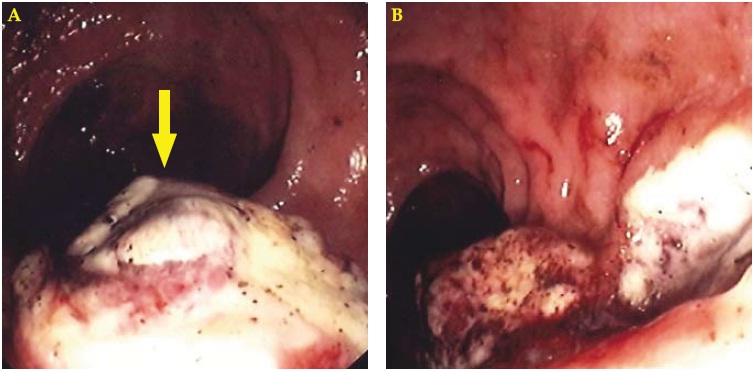
Fig. 1. Endoscopic view showing a large polypoid white lesion in the distal rectum (a). This lesion was partially excised with a polipectomy snare (b).
Histological findings were consistent with malignant melanoma (Fig. 2) and immunohistochemical stain was positive for S100 and HMB45 confirming the diagnosis.
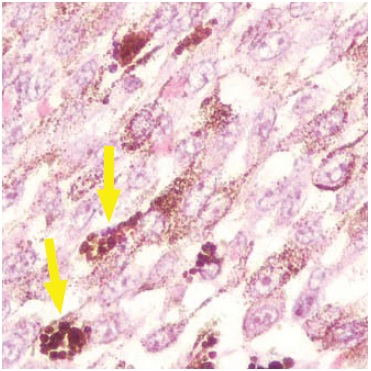
Fig. 2. Histological observation revealed pigmented areas (400 x magnification) suggesting melanoma (a).
Accordingly the patient was referred to a specialized oncology centre where abdomino-perineal resection was performed in January of 2008 showing no involvement of regional lymph nodes. Six months after surgery liver metastasis were diagnosed and the patient eventually died one month later.
The authors emphasize the rarity of this condition and the rapid tumour growth in a very short period of time.
Bibliografia
1. Balicevic D, Tomic K, Bekavac-Beslin M, Kovacevic I, Mijic A, Belicza M, et al. Synchronous anorectal melanoma. World J Gastroenterol. 2006;12:3453-3455.
2. van Schaik PM, Ernst MF, Meijer HA, Bosscha K. Melanoma of the rectum: A rare entity. World J Gastroenterol. 2008;14:1633-1635.
3. Tsigris C, Pikoulis E, Bramis J, Leppäniemi A, Alexiou D, Bastounis E. Malignant melanoma of the anorectal area. Report of two cases. Dig Surg 2000;17:194-196.
4. Hillenbrand A, Barth TF, Henne-Bruns D, Formentini A. Anorectal amelanotic melanoma. Colorectal Dis 2008;10:612-615.
5. Stroh C, Manger T. Primary amelanotic anorectal melanoma – a case report. Zentralbl Chir 2007;132:560-563. [ Links ]
Correspondência: Bruno Arroja; Morada: Hospital de Santo André EPE, Serviço de Gastrenterologia; Rua das Olhalvas – Pousos 2410 – 197, Leiria, Portugal; Contacto telefónico hospitalar: 244 817 000; Contacto telefónico pessoal: 91 9917216
Recebido para publicação: 22/03/2008 e Aceite para publicação: 30 /07/2008













