Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. v.18 n.3 Lisboa maio 2011
Apresentação invulgar de colite associada ao Clostridium difficile
Unusual presentation of Clostridium difficile-associated colitis
Rosa Ferreira1, Joana Torres1, Joana Alves2, Maria João Pereira1, Joana Carvalheiro1, Sofia Mendes1, Margarida Ferreira1, Cláudia Agostinho1, Edgard Panão1, Mário Júlio Campos1
1Serviço de Gastrenterologia, Centro Hospitalar de Coimbra; 2Serviço de Anatomia Patológica, Centro Hospitalar de Coimbra
A 67-year-old woman, resident in a nursing home since the age of 41 due to mental retardation, presented in the emergency department withmelena followed by hematochezia for the past two days. There was no history of hematemesis, nausea, abdominal pain, diarrhea or fever. She was only on antipsychotic and anti-epileptic medication.
Physical examination was unremarkable except for pallor and hypotension (95/56mmHg).
Laboratory data revealed anemia of 10.8 g/dL (normal range (NR): 12 - 16), hypoalbuminemia of 26 g/L (NR: 35 - 50) and elevation of C-reactive protein of 11.8 mg/dL (NR: < 0.5).
Upper endoscopy was performed which was normal. Total colonoscopy revealed a tortuous mucosal prominence of purple color, extending longitudinally from the sigmoid to the distal transverse colon, occupying one fifth of the lumen, partially covered with a whitish exudate not removed by vigorous lavage, resembling a colonicvarix (Fig. 1). Adjacent mucosa was erythematous and friable, with small whitish exudates, which biopsies showed colonic mucosa with superficial erosion and pseudomembranes with volcanic appearance, composed of fibrin, mucus and neutrophils (Fig. 2), suggesting Clostridium difficile (CD) associated colitis. On suspicion of infectious colitis, she startedmetronidazole 500 mg tid orally during 14 days. No rebleeding episodes were seen. Further evaluation excluded portal hypertension. Follow-up colonoscopy one month later showed complete disappearance of the endoscopic findings and no mucosal lesions. A final diagnosis of CD-associated colitis was established.

Fig. 1. Colonoscopy showing an apparent varix of the transverse colon with erythematous and friable adjacent mucosa.
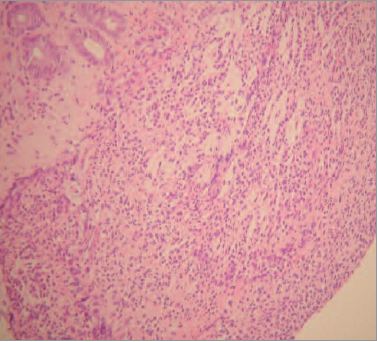
Fig. 2. Pseudomembrane of volcanic appearance composed by fibrin, mucin andneutrophils. (Haematoxylin & eosin, X 400).
Infection from CD occurs when a susceptible host ingests spores of this anaerobic, gram positive bacillus, which colonize the large bowel and release 2 toxins that may cause diarrhea and colitis1. Although the main risk factor for CD infection is antibiotic use, hospitalization, residence in nursing homes and age greater than 65 years are also predisposing factors1-4. This patient met two of these risk factors. Diarrhea, usually watery, is the main symptom2,3. Rarely, as in this case, there are bloody stools2,3.
Endoscopically, colonic pseudomembranes are almostpathognomonic for CD infection, but are not found in all areas of the colon and may be absent in half of the patients2,3. Pseudomembranes are raised yellow or whitish plaques, up to 2 cm of diameter, which are interspersed with normal mucosa and cannot be removed by lavage2. In this case, the pseudomembranes assumed an unusual form, mimicking a colonic varix, an aspect, to our knowledge, not yet described in the literature. Although CD infection may be confirmed by a positive test for CD toxins in stool, false positives and false negatives are not uncommon4. In this case, the absence of diarrhea and recent use of antibiotics, associated with atypical endoscopic features led us to startmetronidazole prior to the collection of stool samples. Treatment of CD infection involves the evaluation of the clinical and laboratory markers of disease severity1,2. The only treatments proven effective are antibiotic therapy andcolectomy for fulminant disease non-responding to antibiotics 1. Although vancomycin is currently considered the first-line treatment in severe CD infection 1, our patient was successfully treated with metronidazole. In summary, this case illustrates an atypical presentation of CD colitis, characterized clinically by gastrointestinal bleeding and endoscopically by pseudomembranes resembling colonicvarices.
REFERENCES
1. Leffler DA, Lamont JT. Treatment of Clostridium difficile-associated disease. Gastroenterology 2009;136:1899-1912. [ Links ]
2. Hookman P, Barkin JS. Clostridium difficile associated infection, diarrhea and colitis. World J Gastroenterol 2009;15:1554-1580. [ Links ]
3. Bartlett JG, Gerding DN. Clinical recognition and diagnosis of Clostridium difficile infection.Clin Infect Dis 2008;15:12-18. [ Links ]
4. Durai R. Epidemiology, pathogenesis, and management of Clostridium difficile infection. Dig Dis Sci 2007;52:2958-2962. [ Links ]
5. Tonna I, Welsby PD. Pathogenesis and treatment of Clostridium difficile infection. Postgrad Med J 2005;81:367-369. [ Links ]
Correspondência: Rosa Ferreira; Rua Carlos Seixas, nº 266, 2ºdto, 3030-177 Coimbra – Portugal; Telemóvel: +351 966 510 601; Fax: +351 239 800 053; E-mail: rosa.l.ferreira@gmail.com
Recebido para publicação: 28/07/2010 e Aceite para publicação: 20/10/2010.













