Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.19 no.5 Lisboa set. 2012
Eosinophilic esophagitis and refractory heartburn: Case report and review of literature
Esofagite eosinofílica e azia refratária: relato de caso e revisão da literatura
Inês Marquesa,∗, Ana Lagosa, Irene Martinsb, António Pintoa, Beatriz Nevesa
a Serviço de Gastrenterologia, Hospital Pulido Valente (CHLN), Lisboa, Portugal
b Serviço de Gastrenterologia, Hospital Cuf Cascais, Cascais, Portugal
*Corresponding author
Abstract
Eosinophilic esophagitis is an inflammatory condition in which there is dense eosinophilic infiltration of the esophageal lining epithelium. The adult form has only recently gained recognition as a distinct entity. Because of the reflux-type symptomatology, it is commonly misdiagnosed and treated as severe gastroesophageal reflux disease before an appropriate diagnosis is made. We herein present a case of an asthmatic young woman in whom eosinophilic esophagitis was suspected based on symptoms of gastroesophageal reflux disease refractory to standard medical therapy. Biopsies taken from esophageal normal appearing mucosa were essential to establish the diagnosis. She was successfully treated with swallowed fluticasone.
As clinical and pathologic features of gastroesophageal reflux disease and eosinophilic esophagitis may overlap, proper diagnosis requires a keen index of suspicion. Increased awareness of eosinophilic esophagitis is necessary, since treatment with topical steroids may be more effective than acid suppression.
Keywords Eosinophils; Esophagitis; Gastro-esophageal reflux disease; Asthma; Fluticasone
Resumo
A esofagite eosinofílica constitui uma condição inflamatória em que ocorre exuberante infiltração do epitélio esofágico por eosinófilos. No adulto, apenas recentemente foi reconhecida como uma entidade distinta. Devido à semelhança clínica, é muitas vezes confundida e tratada como a doença do refluxo gastroesofágico severa antes do estabelecimento do diagnóstico correto. Apresenta-se o caso de uma doente jovem com asma em quem a esofagite eosinofílica foi suspeitada perante sintomas de refluxo gastroesofágico refratários à terapêutica médica standard. A obtenção de biopsias da mucosa esofágica com aspeto endoscopicamente normal foi essencial para o estabelecimento do diagnóstico. A doente foi tratada com sucesso com fluticasona deglutida.
Como as características clínicas e anatomo-patológicas da doença do refluxo gastroesofágico e da esofagite eosinofílica poderão sobrepor-se, o diagnóstico requer um elevado grau de suspeita. Torna-se assim necessária a crescente sensibilização para esta entidade, já que a corticoterapia tópica poderá ser mais eficaz do que a supressão ácida.
Palavras-chave Eosinófilos; Esofagite; Doença do refluxo gastroesofágico; Asma; Fluticasona
Introduction
Eosinophilic esophagitis is an increasingly recognized cause of atypical chest pain and heartburn that does not respond to aggressive anti-reflux therapy. It is best known in the pediatric population, but its recognition in adults has increased over the past 10 years.
The cause of eosinophilic esophagitis is poorly understood, but allergic and immune-mediated mechanisms similar to those of asthma are implicated.1
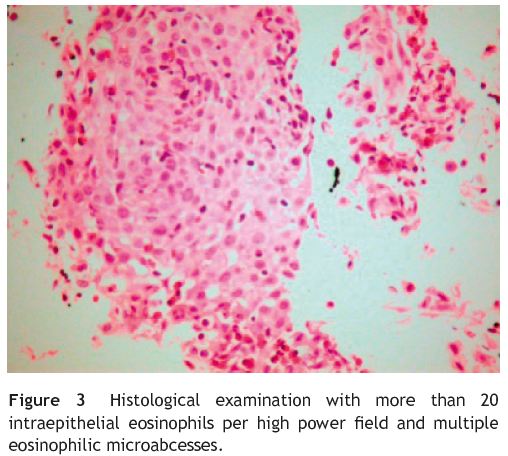
Eosinophilic esophagitis is defined as a clinicopathologic entity, combining clinical data on (1) relevant symptoms (distinct in the pediatric or adult populations, with mostly food impaction and dysphagia in adults and feeding intolerance, failure to thrive and gastroesophageal reflux disease (GERD) symptoms in children and adolescent); (2) esophageal biopsies with adequate histologic findings (≥20 eosinophils/ high-power field); and (3) exclusion of other diseases with overlapping features, especially GERD.1
Endoscopic examination of the esophagus may reveal furrows, corrugations, rings, whitish plaques, crêpe-paper like appearance and a small-caliber esophagus. Demonstration of marked eosinophilic infiltration in the esophageal epithelia is the diagnostic hallmark and biopsies should be taken even in normal-appearing mucosa if clinical suspicion is high.
Optimal treatment remains unclear.2 Swallowed fluticasone, proton pump inhibitor and avoidance of dietary and airborne allergens may be helpful in some patients. Available data suggests that eosinophilic esophagitis runs a benign course, albeit with relapses and need of retreatment.
We herein present a case of eosinophilic esophagitis in young woman with asthma and symptoms of GERD refractory to maximal doses of pump inhibitor. Awareness and a high index of suspicion were essential to establish the diagnosis. Clinical symptoms and esophageal histology improved with swallowed fluticasone.
Case report
A 22-year-old woman with a history of asthma since childhood presented with heartburn. Complaints were worse in recumbent position and after meals. There was no history of vomiting, dysphagia, food impaction or hematemesis. She had no constitutional features such as weight loss, fever or any other symptom suggesting systemic disease.
Physical examination was unremarkable and complete blood counts revealed discrete eosinophilia, with na eosinophilic count of 680/_L (10%) (upper limit of normal = 500/_L (6%)). There was no anemia, IgE levels were normal and specific IgE to pollens and grass was positive.
An upper gastrointestinal endoscopy was performed and revealed a normal appearing mucosa (Fig. 1). No biopsies were taken and she was diagnosed with non-erosive reflux disease. A 3 month trial with proton pump inhibitors at maximal doses was tried, but heartburn persisted and she began to complaining of intermittent solid-food dysphagia. Esophageal motility study with pH monitoring and barium radiography (Fig. 2) were performed and found to be normal.
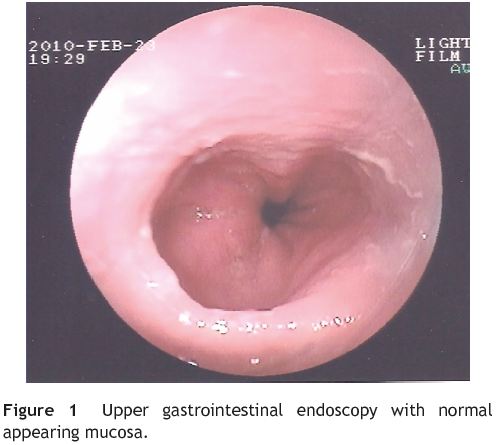

Because of persistent heartburn that did not improve with appropriate medical treatment and taking in to account her past asthmatic history, eosinophilic esophagitis was suspected. Upper gastrointestinal endoscopy was then repeated and again revealed normal-appearing mucosa of esophagus, stomach and duodenum. Notwithstanding, biopsies were obtained from the proximal and distal esophagus. Histological examination revealed more than 20 intraepithelial eosinophils per high power field and multiple eosinophilic microabcesses (Fig. 3), both diagnostic of eosinophilic esophagitis. Biopsies from stomach and duodenum were also obtained and histological findings were normal.
The patient was treated with a fluticasone inhaler (four 200_g puffs twice daily), with instructions to swallow and to rinse her mouth. She also continued treatment with pumpinhibitor (omeprazol 40 mg/day).
During the next 6 months, her symptoms improved. An endoscopy was then carried out and new biopsies from middle and distal esophagus were taken. No eosinophils were found in the biopsy specimen.
Discussion
Increased number of eosinophils in the gastrointestinal tract has been described in a variety of diseases including Crohns disease, connective tissue disorders, malignancy and hypersensivity reactions.1 However, not until 1993 was eosinophilic esophagitis described as a clinical entity.3
The pathologic mechanisms of eosinophilic esophagitis are unknown, but emerging evidence suggests that, like many other allergic diseases, it is mediated by a type 2 T helper cell immune response. Actually, up to 80% of patients with eosinophilic esophagitis have a history of atopic disease such as asthma, allergic rhinitis, eczema or allergies to food.1 Peripheral eosinophilia is seen in 31% of patients.4 Our patient showed increased blood eosinophils but the sérum IgE level was normal and she had a history of bronchial asthma.
Clinical presentations of this newly recognized disease include dysphagia (93%), food impaction (62%), atypical chest pain and heartburn (34%)4 that does not respond to standard medical treatment.
Careful endoscopic examination may reveal ringed appearance, subtle furrows, whitish plaques, fragile crepe paper-like appearance and a small-caliber esophagus. Between 9% and 32% of patients with symptoms have normal endoscopic findings.1
Barium radiography may demonstrate concentric rings or strictures and should be performed before esophageal dilatation. Esophageal manometry is of limited diagnostic value and so is not recommended as a routine test.1
Marked eosinophil infiltration in the esophageal epithelia (>20 eosinophils per high-power field) is the diagnostic Hallmark and samples should be obtained from proximal and distal esophagus,1-4 even in normal appearing mucosa in endoscopy.5 In our case report, we found normal appearing mucosa at endoscopy, but esophageal biopsies revealed marked eosinophilic infiltration. Recently, a prospective study conducted by Prasad G. et al. concluded that midesophageal biopsies taken from normal-appearing mucosa in patients with unexplained solid food dysphagia may diagnose eosinophilic esophagitis in about one in 10 cases.6
Clinical and pathologic features of gastroesophageal reflux disease (GERD) and eosinophilic esophagitis may overlap.5 Both diseases share varying degrees of esophageal eosinophilia and some authors suggest that mucosal injury caused by acid reflux may allow swallowed allergens to penetrate esophageal mucosa causing mild eosinophilia.5,7 Gastroesophageal reflux disease is actually the most common cause of eosinophilic infiltration of the esophagus. However, GERD-related infiltrates tend to be less dense and the greatest number is in the distal esophagus, whereas the dense infiltrates of eosinophilic esophagitis are seen throughout the esophagus.5,7 Because of this possible overlap, the diagnosis of eosinophilic esophagitis should be made after acid reflux has been treated or excluded.1,5 Before we considered eosinophilic esophagitis diagnosis and performed esophageal biopsies, our patient tried a trial with pump proton inhibitor at maximum doses and a pH monitoring excluded pathologic gastroesophageal reflux. Therefore, our patient met all criteria for definitive diagnosis of eosinophilic esophagitis: clinical symptoms, compatible histology and lack of responsiveness to high-dose pump protón inhibitor with normal pH monitoring of the distal esophagus.
Because many patients with eosinophilic esophagitis have atopic disease, a complete evaluation for dietary and inhaled allergens by an experienced allergist is recommended. Although we could not find any correlation between our patients reflux symptoms and exposition to pollens or grass, avoidance of allergens may be helpful in some patients.1 Large-scale studies in adults have not been conducted.
There is no consensus regarding the treatment of eosinophilic esophagitis. In adults, food allergy is less responsible and treatment with topical steroids has lead to remission of symptoms and normalization of hitopathology.1,8 Treatment involves spraying and actuation of fluticasone from an inhaler into the mouth and having the patient swallow. Patients should be instructed to avoid food and liquids for at least 30 minutes after use.1,9 A trial of a proton pump inhibitor at maximum doses for at least 8 weeks is also recommended.1 Swallowed fluticasone was very effective in our patient, leading to complete clinical remission after one month of treatment. After six months of treatment, there were no eosinophils in esophageal biopsies.
In patients whose symptoms do not improve with fluticasone, several other medications may be tried like systemic corticosteroids, cromolyn sodium and montelukast. A recent open-label trial with mepolizumab, a humanized monoclonal antibody to human interleukin 5, improved clinical symptoms in patients with refractory eosinophilic esophagitis.10
Esophageal stenosis may complicate esophageal esophagitis. Endoscopic dilation with either a guidewire or a balloon technique may be used, despite the increased risk of perforation compared with other indications for dilatation.1
The long-term prognosis of eosinophilic esophagitis is uncertain, but data suggests a benign course, despite the chronic and relapsing nature of this entity.
Conclusion
Eosinophilic esophagitis is a recently recognized disorder receiving increasing attention. Clinicians should have a high suspicion for this condition in younger patients with atopic symptoms presenting with dysphagia, food impaction or heartburn that does not respond to maximal doses of protón pump inhibitor.
Our case report emphasizes that in patients with refractory GERD symptoms, biopsies taken from esophageal normal appearing-mucosa may be worthwhile. It is imperative to consider eosinophilic esophagitis in the differential diagnosis of treatment resistant GERD, as the dichotomy of the treatment modalities may result in early recovery of this condition and avoid complications.
References
1. Nonevski I, Downs E, Falk G. Eosinophilic esophagitis: na increasingly recognized cause of dysphagia, food impaction, and refractory heartburn. Cleve Clin J Med. 2008;75:623-6, 629-33. [ Links ]
2. Hawari R, Pasricha P. Eosinophilic esophagitis. N Engl J Med. 2007;356:20. [ Links ]
3. Attwood S, Smyrk T, Demeester T, Jones B. Esophageal eosinophilia with dysphagia. Dig Dis Sci. 1993;38:109-16. [ Links ]
4. Sgouros S, Bergele C, Mantides A. Eosinophilic esophagitis in adults: what is the clinical significance? Endoscopy. 2006;38:515-20. [ Links ]
5. Odze R. Pathology of eosinophilic esophagitis: what the clinician needs to know. Am J Gastroenterol. 2009;104:485-90. [ Links ]
6. Prasad G, Talley N, Romero Y, Arora A, Kryzer L, Smyrk T, et al. Prevalence and predictive factors of eosinophilic esophagitis in patients presenting with dysphagia: a prospective study. Am J Gastroenterol. 2007;102:2627-52. [ Links ]
7. Spechler S, Genta R, Souza R. Thoughts on the complex relationship between gastroesophageal reflux disease and eosinophilic esophagitis. Am J Gastroenterol. 2007;102:1301-6. [ Links ]
8. Arora A, Perrault J, Smyrk T. Topical corticosteroid treatment of dysphagia due to eosinophilic esopahgitis in adults. Mayo Clin Proc. 2003;78:830-5. [ Links ]
9. Mungan Z, Pinarbasi B, Kaymakoglu S. Eosinophilic esophagitis: case report. Turk J Gastroenterol. 2007;18:100-2. [ Links ]
10. Stein M, Collins M, Villanueva J, Kushner J, Putnam P, Buckmeier B, et al. Anti-IL-5 (mepolizumab) therapy for eosinophilic esophagitis. J Allergy Clin Immunol. 2006;118: 1312-9. [ Links ]
Conflicts of interest
The authors have no conflicts of interest to declare.
*Corresponding author
E-mail address:inesnmarques@zonmail.pt (I. Marques).
Received 9 October 2010; accepted 15 December 2010













