Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.19 no.6 Lisboa nov. 2012
https://doi.org/10.1016/j.jpg.2012.09.004
Position paper on tuberculosis screening in patients with imune mediated inflammatory diseases who are candidates for biological therapy
Rastreio da tuberculose em portadores de doenças inflamatórias imunomediadas candidatos a terapêutica biológica
Raquel Duartea,b,c,∗,1, Sergio Campainhaa,b,1, José Cotterd,2, Bruno Rosad,2, Paulo Varelae,3, Ana Correiaf,1, Helena Canhãog,h,4, João Eurico Fonsecag,h,4
a Centro de Referência de Tuberculose Multi-resistente da Região Norte, Portugal
b Serviço de Pneumologia, Centro Hospitalar de Vila Nova de Gaia/Espinho, Portugal
c Departamento de Epidemiologia Clínica, Medicina Preventiva e Saúde Pública, Faculdade de Medicina da Universidade do Porto, Porto, Portugal
d Serviço de Gastrenterologia, Centro Hospitalar do Alto Ave - Guimarães, Guimarães, Portugal
e Serviço de Dermatologia e Venereologia, Centro Hospitalar de Vila Nova de Gaia/Espinho, Portugal
f Departamento de Saúde Pública, Administração Regional de Saúde do Norte, Portugal
g Serviço de Reumatologia, Hospital de Santa Maria, Portugal
h Unidade de Investigação em Reumatologia, Instituto de Medicina Molecular, Faculdade de Medicina, Universidade de Lisboa, Lisboa, Portugal
1 On behalf of Portuguese Society of Pulmonology.
2 On behalf of Portuguese Society of Gastroenterology.
3 On behalf of Portuguese Society of Dermatology and Venereology.
4 On behalf of Portuguese Society of Rheumatology.
*Corresponding author.
Abstract
Chronic immunosuppression is a known risk factor for tuberculosis. Our aim was to reach a consensus on screening and prevention of tuberculosis in patients with immune mediated inflammatory diseases who are candidates to biologic therapy.
Methods: Critical appraisal of the literature and expert opinion on immunosuppressive therapies and risk of tuberculosis.
Results and conclusion: The currently recommended method for screening is the tuberculin skin test and the interferon gamma assay, after exclusion of active tuberculosis. Positively screened patients should be treated for latent tuberculosis infection. Patients may start biological therapy after 1-2 months, as long as they are strictly adhering to and tolerating their preventive regimen.
KEYWORDS Tuberculosis screening; Latent tuberculosis; Biological therapies; Anti-TNF drugs; Immune mediated inflammatory diseases
Resumo
A imunossupressão crónica é um reconhecido factor de risco para a tuberculose. O nosso objectivo foi o de obter um consenso para o rastreio e prevenção da tuberculose em portadores de doenças inflamatórias imunomediadas candidatos a terapêutica biológica.
Métodos: Revisão crítica da literatura e opinião de peritos acerca das terapêuticas imunossupressoras e risco de tuberculose.
Resultados e conclusão: O método actualmente recomendado para o rastreio é o teste cutâneo da tuberculina e o doseamento do interferão gama, após exclusão da tuberculose activa. Doentes com rastreio positivo devem receber tratamento para a tuberculose latente. Estes doentes podem iniciar a terapêutica biológica após 1 a 2 meses, desde que a sua adesão seja rigorosa e apresentem boa tolerância à terapêutica profilática.
PALAVRAS-CHAVE Rastreio da tuberculose; Tuberculose latente; Terapêutica biológica; Terapêutica anti-TNF; Doenças inflamatórias imuno-mediadas
Introduction
In populations with high incidence of tuberculosis (TB), there have been an increased number of TB cases reported in patients treated with tumor necrosis factor antagonists (anti-TNF).1 In fact, the relative risk (RR) of developing TB is 1.6---25.2 times higher in Rheumatoid Arthritis (RA) patients under anti-TNF therapy than in RA patients treated with conventional immunosuppressive therapy, depending on the clinical setting and the anti-TNF used.1-7
Active TB in the context of anti-TNF therapy usually results from the reactivation of a latent infection, shortly after the beginning of the treatment.5,8 TB often presents an atypical behavior, which may pose difficulties to the diagnosis.9 In countries with high incidence of TB, cases caused by new infection are also particularly frequent. TNF is fundamental for the immunological defence against Mycobacterium tuberculosis, especially in the formation and maintenance of granulomas. Animal models confirmed that it is possible to reactivate TB after administering anti-TNF antibodies.10
Besides anti-TNFs, other biological agents were approved for immune mediated inflammatory diseases treatment. Data about the risk of developing TB infection in patients treated with these other agents are scarce. Even though this risk might be lower for some of the biological agents that do not interfere with TNF until more data is available this group assumed that this position paper should be applied to all biological treatments.
Preventive chemotherapy can significantly reduce the incidence of active TB in individuals with latent infection, identified by positive tuberculin skin test (TST) or interferon-_ release assay (IGRA).11
The currently available evidence about the best management to prevent TB in patients receiving biological therapy is limited. In this position paper on the screening and prevention of TB in patients treated with biological therapy, delegates from the Tuberculosis Committee (TC) of the Portuguese Pulmonology Society (SPP), the Rheumatoid Arthritis Study Group (GEAR) of the Portuguese Society of Rheumatology (SPR), the Portuguese Society of Dermatology and Venereology (SPDV) and the Portuguese Society of Gastroenterology (SPG), have revised and updated recommendations that had been previously developed by the GEAR --- SPR and by the TC --- SPP, first published in 200612 and latter updated in 2008.13
The main objective of this position paper is to contribute for the reduction of the number of cases of reactivated TB and new TB infections in patients with immune mediated inflammatory diseases who are candidates for treatment with biological therapy in Portugal. An additional objective is to standardize the procedures used to screen and prevent TB in the initial assessment of these patients, preferably at disease onset, before the beginning of any immunosuppressant therapy.
Recommendations
Who should be screened?
All patients with immune mediated inflammatory diseases who are candidates for the use of biological therapy should be screened for latent TB infection (LTBI) prior to starting therapy (Evidence level C).
Patients eligible for anti-TNF therapy have an increased risk of developing TB upon starting this treatment. TB in this setting can present with severe, atypical and lifethreatening manifestations. This risk exists not only due to the biological importance of TNF in the initiation and maintenance of the response against M. tuberculosis, but also because the underlying diseases (e.g. RA) and concomitante treatments (e.g. steroid therapy) increase the risk of TB per se.14-18 Most of the active TB cases in patients treated with anti-TNF are due to reactivation of LTBI. It is well known that screening for LTBI before starting anti-TNF therapy is effective in preventing reactivation of TB.17 Therefore, all national guidelines recommend the exclusion of active TB disease and LTBI in patients in whom biological therapy is considered.19-21
When to screen?
Patients with immune mediated inflammatory diseases should be screened for TB before starting biologic treatment and ideally when the disease is diagnosed (Evidence level C).
Any candidate to biological therapy should be screened for the presence of specific immune response to M. tuberculosis (including TST and IGRA) before starting these drugs and ideally when the immune mediated inflammatory disease is diagnosed, except in patients with mild forms of psoriasis, treated with topical drugs.19-21
It has been shown that certain diseases, such as RA, as well as chronic immunosuppressive therapy, such as corticosteroids (>15 mg/day for more than 2 weeks) increase the risk of TB. In addition, it is also well known that immunosuppressive therapy compromises the sensitivity of the TST and IGRA, this being especially true for TST.16,18,22-25 Therefore, it is highly desirable that the first screen for TB should be done at the moment of diagnosis, before any kind of immunosuppressive treatment or phototherapy is started.
Which tests should we use?
After exclusion of active TB, LTBI should be screened with TST and IGRA (Evidence level C and D).
In the light of current knowledge, and in the absence of a gold standard test for LTBI diagnosis,19 the screening process for LTBI requires a combination of a detailed medical history (which should include ethnicity, country of birth, history of or recent exposure to TB, previous TB and respective treatment, co-morbidities associated with increased risk of TB, professional activities with increased risk of exposure to TB), travel to endemic areas, chest radiograph (searching for changes indicative of active or residual previous TB) and tests for immunological memory against M. tuberculosis (TST and IGRA).19 In erythrodermic psoriasis TST may be impossible to perform, reinforcing the need of IGRA in these cases.
The sensitivity of both tests may be compromised in patients receiving immunosuppressive therapy, although published evidence suggests that IGRA has a higher sensitivity than TST in patients with immune mediated inflammatory diseases, even after starting immunosuppressive therapy.26-30
Currently, different guidelines are adopted regarding the use of TST and IGRA, reflecting the difficulty of choosing the best strategy.19,24,31-33 Over-treatment, implying the risk of drug toxicity due to a false-positive screening and undertreatment due to a false-negative screening are the main concerns.
Since the increase in sensitivity and specificity provided by IGRA in different studies is controversial and their positive and negative predictive values are yet to be defined, the role of IGRA is still under investigation. In this sense, IGRA cannot yet be used as a single test for immunological memory to M. tuberculosis. Thus, currently it is prudent to use both TST and IGRA in order to maximize sensitivity.19,24,31
Since patients may have false negative TST due to immunosuppression, a two step approach is advised-repeat TST 1-3 weeks after the initial negative screening.
How to exclude active tuberculosis in patients with Crohns disease?
Acid fast bacilli smear and culture should be performed in endoscopic biopsies (Evidence level C).
The distinction between Crohns disease and intestinal TB is a diagnostic challenge, as they present similar clinical, radiological, endoscopic and histological features. Investigation of patients with suspected Crohns disease should always include differential diagnosis with intestinal TB. Acid fast bacilli smear and culture are warranted in pathological examination of endoscopic biopsies. Other tests such as nucleic acid amplification, immunohistochemistry or in situ hybridization are promising techniques that have been evaluated in some studies, but they are not widely available and require further validation.34-51
How to interpret the tuberculin skin test?
TST is considered positive if induration is ≥5mm in previously immunosuppressed patients and if ≥10mm in patients not previously exposed to immunosuppressors (Evidence level D).
In order to increase the sensitivity of TST (at the expense of lower specificity) different guidelines recommend, in the immunocompromised population, an induration of ≥5mmto be the cut-off for a positive TST.19,21,52,53
The Tuberculosis Network European Trials Group (TBNET) recommends a cut-off value of 10mm, stating that the loss of sensitivity to detect infection by increasing the cut-off from 5 to 10mm is marginal, while the gain in specificity is substantial.19 Taking this into consideration, TBNET suggests that a TST≥10mm should lead to LTBI treatment, without requiring IGRA confirmation. This evidence is based on results of non-controlled and non-randomized trials and on observational studies.
According to the Portuguese clinical practice, patients with immune mediated inflammatory diseases, who are candidates for anti-TNF therapy, should undergo a TST: the test is considered positive in previously immunosuppressed patients if the induration is ≥5mm and in patients not previously exposed to immunosuppressors if the induration is ≥10mm.
Who should start latent tuberculosis infection treatment?
Patients with epidemiological risk factors for TB (history of exposure to TB, previous TB, emigrants from high TB prevalence areas, residents in high incidence areas, co morbidities associated with increased risk of TB, professional activities with increased risk of exposure to TB, travel to endemic areas), or chest X-ray sequelae of untreated previous TB, or positive TST and/or IGRA, should start LTBI treatment, after exclusion of active TB (Evidence level C and D).
Whenever there is evidence of exposure to TB (regardless the results of the screening and after exclusion of active TB) or LTBI (positive TST and/or IGRA or changes in chest radiograph suggestive of previous untreated TB), after exclusion of active TB, preventive treatment should be offered before initiating biological therapy, as these patients have a high risk of progression to disease.19,21,54-57
Due to the risk of serious forms of disease, treatment must be offered to candidates for biological therapy regardless of age and presumed date of infection.
Which latent tuberculosis infection treatment regimen should be used?
Isoniazid for 9 months (Evidence level C and D).
Several therapeutic strategies have been proposed. Isoniazid is classically recommended as this drug in immunocompromised patients has proven to be effective (data derived from multiple studies in HIV patients).58-60 Isoniazid for a period of 9 months is the most commonly used regímen and has an estimated efficacy of around 90%. This regímen is recommended by the American Thoracic Society (ATS)61 and Canadian Tuberculosis Standards,62 while the 6 months regimen, in which effectiveness varies between 65 and 69%, is proposed by the National Institute for Health and Clinical Excellence (NICE).63
TBNET recommends treatment with isoniazid for 9-12 months or isoniazid and rifampicin for 3 months (3HR).19 However, the later is associated with a lower efficacy (around 60%). Some studies indicate that 4 months of rifampicin (4R) are at least as effective as 3HR and this regime has the advantage of being better accepted by patients, having fewer adverse effects when compared with regimens based on isoniazid and is associated with a lower cost to the health system.64-68 These are very relevant advantages but effectiveness remains uncertain, as this regímen has not yet been tested extensively in randomized trials.
In the light of current knowledge, treatment with isoniazid for 9 months is the most consensual option.19,59,60 One month is defined as the minimum LTBI treatment duration before starting biological drugs.19 This recommendation is based on expert opinion.
Evaluation of the risk for toxicity due to latent tuberculosis infection treatment
Patient education, clinical monitoring, baseline and monthly laboratory testing of liver enzymes (Evidence level C and D).
Given the high risk of TB in patients starting anti-TNF, the risk of age-related hepatotoxicity69 should not prevent patients from receiving treatment for LTBI. In addition to liver toxicity, isoniazid is associated with toxicity to the nervous system.70 Vitamin B6 reduces central and peripheral effects of isoniazid and should be given to individuals with a history of alcoholism, diabetes, pregnant, postpartum, infants, malnourished, HIV-positive, people with active liver disease, cancer or history of pre-existing peripheral neuropathy.71
In case of choosing rifampicin-based regimens, interactions with other drugs should be considered, since this drug is a potent inducer of CYP450.72
Besides patient education and clinical monitoring, baseline and monthly (or biweekly) laboratory testing of liver enzymes is recommended for people older than 35 years, chronic alcohol abusers, HIV-infected persons, females during pregnancy and within 3 months after delivery and for those with chronic liver disease or taking potentially hepatotoxic concomitant medications. Transient transaminase elevations are common and may reflect the process of hepatic adaptation. However, isoniazid and/or rifampicin should be withheld as recommended if the serum transaminase level is higher than three times the upper limit of normal in a symptomatic patient or five times the upper limit of normal in the absence of symptoms.60,61
A change of the therapeutic regimen for a less hepatotoxic one (as 4R, at the expense of effectiveness) should be considered when serious hepatotoxicity is limiting LTBI treatment with isoniazid.
How should follow up be performed?
Patients should be re-screened for LTBI if the previous screen had been negative and the patient had not started biologicals, to exclude possible infection in the meantime (in the absence of a known contact with a TB patient, the screen would be valuable for 6 months). In the event of contact with active TB, TB screening should be promptly performed and in the absence of disease and LTBI, chemoprophylaxis should be guaranteed.19
Annual testing is recommended for patients, who live, travel or work in environments where TB exposure is likely, while they continue treatment with biologic agents. Patients who tested positive for TST and IGRA should only be monitored for clinical signs of TB.
Summary
1. All candidates for biologic therapy should be screened for TB.
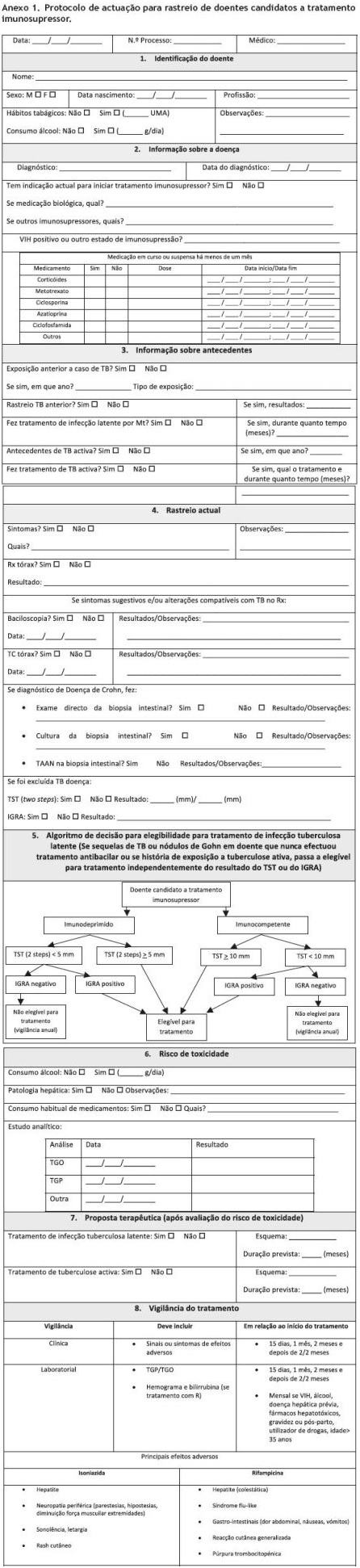
2. TB screening procedures should include risk assessment, evaluation of TB signs and symptoms, chest radiography, TST and IGRA.
3. After exclusion of active TB, the presence of a positive TST (≥10mm in immunocompetent or ≥5mm in immunocompromised conditions) or positive IGRA indicates the possibility of LTBI and LTBI therapy should be offered.
4. The existence of an untreated or inadequately treated previous TB (determined by chest X-ray sequelae and/or clinical history) should be evaluated for active TB and, if that is excluded, LTBI treatment should be given.
5. In the event of a recent exposure to a TB patient, LTBI therapy should be offered, even in the presence of negative screening tests.
6. The recommended regimen for LTBI treatment is 9 months of isoniazid.
7. Annual testing is recommended while on biological treatment.
References
1. Gomez-Reino JJ, Carmona L, Valverde VR, Mola EM, Montero MD, BIOBADASER Group. Treatment of rheumatoid arthritis with tumor necrosis factor inhibitors may predispose to significant increase in tuberculosis risk: a multicenter active-surveillance report. Arthritis Rheum. 2003;48:2122-7. [ Links ]
2. Askling J, Fored CM, Brandt L, Baecklund E, Bertilsson L, Coster L, et al. Risk and case characteristics of tuberculosis in rheumatoid arthritis associated with tumor necrosis factor antagonists in Sweden. Arthritis Rheum. 2005;52: 1986-92. [ Links ]
3. Dixon WG, Watson K, Lunt M, Hyrich KL, Silman AJ, Symmons DP. Rates of serious infection, including site-specific and bacterial intracellular infection, in rheumatoid arthritis patients receiving anti-tumor necrosis factor therapy: results from the British Society for Rheumatology Biologics Register. Arthritis Rheum. 2006;54:2368-76. [ Links ]
4. Ellerin T, Rubin RH, Weinblatt ME. Infections and antitumor necrosis factor alphatherapy. Arthritis Rheum. 2003;48:3013-22. [ Links ]
5. Gomez-Reino JJ, Carmona L, Valverde VR, Mola EM, Montero MD. Treatment of rheumatoid arthritis with tumor necrosis factor inhibitors may predispose to significant increase in tuberculosis risk: a multicenter active-surveillance report. Arthritis Rheum. 2003;48:2122-7. [ Links ]
6. Wolfe F, Michaud K, Anderson J, Urbansky K. Tuberculosis infection in patients with rheumatoid arthritis and the effect of infliximab therapy. Arthritis Rheum. 2004;50:372-9. [ Links ]
7. Wallis RS, Broder M, Wong J, Beenhouwer D. Granulomatous infections due to tumor necrosis factor blockade: correction. Clin Infect Dis. 2004;39:1254-5. [ Links ]
8. Keane J, Gershon S, Wise RP, Mirabile-Levens E, Kasznica J, Schwieterman WD, et al. Tuberculosis associated with infliximab, a tumor necrosis factor alpha-neutralizing agent. N Engl J Med. 2001;345:1098-104. [ Links ]
9. Garcia Vidal C, Rodríguez Fernández S, Martínez Lacasa J, Salavert M, Vidal R, Rodríguez Carballeira M, et al. Paradoxical response to antituberculous therapy in infliximab-treated patients with disseminated tuberculosis. Clin Infect Dis. 2005;40:756-9. [ Links ]
10. Mohan VP, Scanga CA, Yu K, Scott HM, Tanaka KE, Tsang E, et al. Effects of tumor necrosis factor alpha on host immune response in chronic persistent tuberculosis: possible role for limiting pathology. Infect Immun. 2001;69: 1847-55. [ Links ]
11. Gomez-Reino JJ, Carmona L, Angel Descalzo M. Risk of tuberculosis in patients treated with tumor necrosis factor antagonists due to incomplete prevention of reactivation of latent infection. Arthritis Rheum. 2007;57:756-61. [ Links ]
12. Fonseca JE, Lucas H, Canhão H, Duarte R, Santos MJ, Villar M, et al. Recomendações para diagnóstico e tratamento da tuberculose latente e activa nas doenças inflamatórias articulares candidatas a tratamento com fármacos inibidores do factor de necrose alfa. Rev Port Pneumol. 2006;12:603-13. [ Links ]
13. Fonseca JE, Lucas H, Canhão H, Duarte R, Santos MJ, Villar M, et al. Recommendations for the diagnosis and treatment of latent and active tuberculosis in inflammatory joint diseases candidates for therapy with tumor necrosis factor alpha inhibitors: March 2008 update. Acta Reumatol Port. 2008;33:77-85. [ Links ]
14. Doran MF, Crowson CS, Pond GR, OFallon WM, Gabriel SE. Frequency of infection in patients with rheumatoid arthritis compared with controls: a population-based study. Arthritis Rheum. 2002;46:2287-93. [ Links ]
15. Keyser FD. Choice of Biologic therapy for patients with Therapy for Patients with Rheumatoid Arthritis: The Infection Perspective. Curr Rheumatol Rev. 2011;7:77-87. [ Links ]
16. Erkens CG, Kamphorst M, Abubakar I, Bothamley GH, Chemtob D, Haas W, et al. Tuberculosis contact investigation in low prevalence countries: a European consensus. Eur Respir J. 2010;36:925-49. [ Links ]
17. Carmona L, Gomez-Reino JJ, Rodriguez-Valverde V, Montero D, Pascual-Gomez E, Mola EM, et al. Effectiveness of recommendations to prevent reactivation of latent tuberculosis infection in patients treated with tumor necrosis factor antagonists. Arthritis Rheum. 2005;52:1766-72. [ Links ]
18. Jick SS, Lieberman ES, Rahman MU, Choi HK. Glucocorticoid use, other associated factors, and the risk of tuberculosis. Arthritis Rheum. 2006;55:19-26. [ Links ]
19. Solovic I, Sester M, Gomez-Reino JJ, Rieder HL, Ehlers S, Milburn HJ, et al. The risk of tuberculosis related to tumour necrosis factor antagonist therapies: a TBNET consensus statement. Eur Respir J. 2010;36:1185-206. [ Links ]
20. Ormerod LP, Milburn HJ, Gillespie S, Ledingham J, Rampton D. BTS recommendations for assessing risk and for managing Mycobacterium tuberculosis infection and disease in patients due to start anti-TNF-a treatment. Thorax. 2005;60: 800-5; Curr Rheumatol Rev. 2011;7:77-87. [ Links ]
21. Fonseca JE, Lucas H, Canhão H, Duarte R, Santos MJ, Villar M, et al. Recomendações para diagnóstico e tratamento da tuberculose latente e activa nas doenças inflamatórias articulares candidatas a tratamento com fármacos inibidores do factor de necrose tumoral alfa. Rev Port Pneumol. 2006;XII: 603-13. [ Links ]
22. Lalvani A, Millington K. Screening for tuberculosis infection prior to initiation of anti-TNF therapy. Autoimmun Rev. 2008;8:147-52. [ Links ]
23. Kezer I, Kocabas H, Melikoglu MA, Arman M. Positiveness of purified protein derivatives in rheumatoid arthritis patients who are not receiving immunosuppressive therapy. Clin Rheumatol. 2009;28:53-7. [ Links ]
24. Chen DY, Shen GH, Hsieh TY, Hsieh CW, Lan JL. Effectiveness of the combination of a whole-blood interferon-gamma assay and the tuberculin skin test in detecting latent tuberculosis infection in rheumatoid arthritis patients receiving adalimumab therapy. Arthritis Rheum. 2008;59:800-6. [ Links ]
25. Schatz M, Patterson R, Kloner R, Falk J. The prevalence of tuberculosis and positive tuberculin skin tests in a steroidtreated asthmatic population. Ann Intern Med. 1976;84: 261-5. [ Links ]
26. Ponce de Leon D, Acevedo-Vásquez E, Sánchez-Torres A, Cucho M, Alfaro J, Perich R, et al. Attenuated response to purified protein derivative in patients with rheumatoid arthritis: study in a population with a high prevalence of tuberculosis. Ann Rheum Dis. 2005;64:1360-1. [ Links ]
27. Mori T. Usefulness of interferon-gamma release assays for diagnosing TB infection and problems with these assays. J Infect Chemother. 2009;136:198-204. [ Links ]
28. Pai M, Zwerling A, Menzies D. Systematic review: T-cell based assays for the diagnosis of latent tuberculous infection: na update. Ann Intern Med. 2008;149:177-84. [ Links ]
29. Vassilopoulos D, Stamoulis N, Hadziyannis E, Archimandritis AJ. Usefulness of enzyme-linked immunospot assay (Elispot) compared to tuberculin skin testing for latent tuberculosis screening in rheumatic patients scheduled for anti-tumor necrosis factor treatment. J Rheumatol. 2008;35:1464. [ Links ]
30. Sellam J, Hamdi H, Roy C, Baron G, Lehman M, Puechal X. Comparison of in vitro-specific blood tests with tuberculin skin test for diagnosis of latent tuberculosis before anti-TNF therapy. Ann Rheum Dis. 2007;66:1610-5. [ Links ]
31. Bartalesi F, Vicidomini S, Goletti D, Fiorelli C, Fiori G, Melchiorre D, et al. QuantiFERON-TB Gold and the TST are both useful for latent tuberculosis infection screening in autoimmune diseases. Eur Respir J. 2009;33:586-93. [ Links ]
32. Behar SM, Shin DS, Maier A, Coblyn J, Helfgott S, Weinblatt ME. Use of T-SPOT.TB assay to detect latent tuberculosis infection among rheumatic disease patients on immunosuppressive therapy. J Rheumatol. 2009;36:546-51. [ Links ]
33. Keystone E, Papp L, Wobeser W. Challenges in diagnosing latent tuberculosis infection in patients treated with tumor necrosis factor antagonists. J Rheumatol. 2011;38:1234-43. [ Links ]
34. Pulimood AB, Peter S, Rook GW, Donoghue HD. In situ PCR for Mycobacterium tuberculosis in endoscopic mucosal biopsy specimens of intestinal tuberculosis and Crohns disease. Am J Clin Pathol. 2008;129:846-51. [ Links ]
35. Kirsch R, Pentecost M, Hall P, Epstein DP, Watermeyer G, Friederich PW. Role of colonoscopic biopsy in distinguishing between Crohns disease and intestinal tuberculosis. J Clin Pathol. 2006;59:840-4. [ Links ]
36. Makharia G, Srivastava S, Das P, Goswami P, Singh U, Tripathi M, et al. Clinical, endoscopic, and histological differentiations between Crohns disease and intestinal tuberculosis. Am J Gastroenterol. 2010;105:642-51. [ Links ]
37. Park DY, Kim JY, Choi KU, Lee JS, Lee CH, Sol MY, et al. Comparison of polymerase chain reaction with histopathologic features for diagnosis of tuberculosis in formalin-fixed, paraffin-embedded histologic specimens. Arch Pathol Lab Med. 2003;127:326-30. [ Links ]
38. Amarapurkar DN, Patel ND, Amarapurkar AD, Agal S, Baigal R, Gupte P. Tissue polymerase chain reaction in diagnosis of intestinal tuberculosis and Crohns disease. J Assoc Physicians India. 2004;52:863-7. [ Links ]
39. Kim KM, Lee A, Choi KY, Lee KY, Kwak JJ. Intestinal tuberculosis: clinicopathologic analysis and diagnosis by endoscopic biopsy. Am J Gastroenterol. 1998;93:606-9. [ Links ]
40. Gan HT, Chen YQ, Ouyang Q, Bu H, Yang XY. Differentiation between intestinal tuberculosis and Crohns disease in endoscopic biopsy specimens by polymerase chain reaction. Am J Gastroenterol. 2002;97:1446-51. [ Links ]
41. Ramadass B, Chittaranjan S, Subramanian V, Ramakrishna BS. Fecal polymerase chain reaction for Mycobacterium tuberculosis IS6110 to distinguish Crohns disease from intestinal tuberculosis. Indian J Gastroenterol. 2010;29:152-6. [ Links ]
42. Singh S, Verma R, Shah D. Molecular fingerprinting of clinical isolates of Mycobacterium bovis and Mycobacterium tuberculosis from India by restriction fragment length polymorphism (RFLP). J Vet Sci. 2004;5:331-5. [ Links ]
43. Jin X.J., Kim J.M., Kim H.K., Kim L., Choi S.J., Park I.S., et al. Histopathology and TB-PCR kit analysis in differentiating the diagnosis of intestinal tuberculosis and Crohns disease. World J Gastroenterol. 2010;16:2496-503. [ Links ]
44. Amarapurkar D, Patel N, Rane P. Diagnosis of Crohns disease in India where tuberculosis is widely prevalent. World J Gastroenterol. 2008;14:741-6. [ Links ]
45. Almadi M, Ghosh S, Aljebreen AM. Differentiating intestinal tuberculosis from Crohns disease: a diagnostic challenge. Am J Gastroenterol. 2009;104:1003-12. [ Links ]
46. Leung VK, Law ST, Lam CW, Luk IS, Chau TN, Loke TK, et al. Intestinal tuberculosis in a regional hospital in Hong Kong: a 10-year experience. Hong Kong Med J. 2006;12:264-71. [ Links ]
47. Balamurugan R, Venkataraman S, John KR, Ramakrishna BS. PCR amplification of the IS6110 insertion element of Mycobacterium tuberculosis in fecal samples from patients with intestinal tuberculosis. J Clin Microbiol. 2006;44:1884-6. [ Links ]
48. Pulimood AB, Amarapurkar DN, Ghoshal U, Phillip M, Pai CG, Reddy DN, et al. Differentiation of Crohns disease from intestinal tuberculosis in India in 2010. World J Gastroenterol. 2011;17:433-43. [ Links ]
49. Gan H, Ouyang Q, Bu H, Li S, Chen D, Li G, et al. Value of polymerase chain reaction assay in diagnosis of intestinal tuberculosis and differentiation from Crohns disease. Chin Med J (Engl). 1995;108:215-20. [ Links ]
50. Li J, Lo S, Ng C. Molecular detection of Mycobacterium tuberculosis in tissues showing granulomatous inflammation without demonstrable acid-fast bacilli. Diagn Mol Pathol. 2000;9: 67-74. [ Links ]
51. Preethi G, Venkatesh K, Navaneethan U. Mimickers of intestinal tuberculosis: could this be Crohns disease? An unsolved enigma. Saudi J Gastroenterol. 2011;17:95-6. [ Links ]
52. Soborg B, Ruhwald M, Hetland ML, Jacobsen S, Andersen AB, Milman N, et al. Comparison of screening procedures for Mycobacterium tuberculosis infection among patients with inflammatory diseases. J Rheumatol. 2009;36: 1876-84. [ Links ]
53. Denkinger CM, Dheda K, Pai M. Guidelines on interferon-gamma release assays for tuberculosis infection: concordance, discordance or confusion? Clin Microbiol Infect. 2011;17:806-14. [ Links ]
54. Gómez-Reino JJ, Carmona L, Angel Descalzo M, Biobadaser Group. Risk of tuberculosis in patients treated with tumor necrosis factor antagonists due to incomplete prevention of reactivation of latent infection. Arthritis Rheum. 2007;57:756-61. [ Links ]
55. Brassard P, Kezouh A, Suissa A. Antirheumatic drugs and the risk of tuberculosis. Clin Infect Dis. 2006;43:717-22. [ Links ]
56. Tubach F, Salmon D, Ravaud P, Allanore Y, Goupille P, Bréban M, et al., Research Axed on Tolerance of Biotherapies Group. Risk of tuberculosis is higher with anti-tumor necrosis factor receptor monoclonal antibody therapy than with soluble tumor necrosis factor therapy: the three-year prospective French Research Axed on Tolerance of Biotherapies registry. Arthritis Rheum. 2009;60:1884-94. [ Links ]
57. Wolfe F, Michaud K, Anderson J, Urbansky K. Tuberculosis infection in patients with rheumatoid arthritis and the effect of infliximab therapy. Arthritis Rheum. 2010;50:372-9. [ Links ]
58. Woldehanna S, Volmink J. Treatment of latent tuberculosis infection in HIV infected persons. Cochrane Database Syst Rev. 2004;1:CD000171. [ Links ]
59. Leung C, Rieder H, Lange C, Ywe W. Treatment of latent infection with Mycobacterium tuberculosis: update 2010. Eur Respir J. 2011;37:690-711. [ Links ]
60. Duarte R, Villa M, Carvalho A. Latent tuberculosis infection treatment. Current recommendations. Rev Port Pneumol. 2010;XVI:809-14. [ Links ]
61. American Thoracic Society and Centers for Disease Control and Prevention. Targeted tuberculin testing and treatment of latent tuberculosis infection. MMWR Recomm Rep. 2000;49:1-51. [ Links ]
62. Public Health Agency of Canada and Canadian Lung Association. Canadian tuberculosis standards. Ottawa: Public Health Agency of Canada and Canadian Lung Association; 2007. [ Links ]
63. National Institute for Health and Clinical Excellence. Clinical diagnosis and management of tuberculosis, and measures for its prevention and control. London: National Institute for Health and Clinical Excellence; 2006. [ Links ]
64. Ena J, Valls V. Short-course therapy with rifampin plus isoniazid, compared with standard therapy with isoniazid, for latent tuberculosis infection: a meta-analysis. Clin Infect Dis. 2005;40:670-6. [ Links ]
65. Menzies D, Long R, Trajman A, Dion MJ, Yang J, Al Jahdali H, et al. Adverse events with 4 months of rifampin therapy or 9 months of isoniazid therapy for latent tuberculosis infection: a randomized trial. Ann Intern Med. 2008;149: 689-97. [ Links ]
66. Page KR, Sifakis F, Montes de Oca R, Cronin WA, Doherty MC, Federline L, et al. Improved adherence and less toxicity with rifampin vs. isoniazid for treatment of latent tuberculosis: a retrospective study. Arch Intern Med. 2006;166:863-70. [ Links ]
67. Lardizabal A, Passannante M, Kojakali F, Hayden C, Reichman LB. Enhancement of treatment completion for latent tuberculosis infection with 4 months of rifampin. Chest. 2006;130:1712-7. [ Links ]
68. Aspler A, Long R, Trajman A, Dion MJ, Khan K, Schwartzman K, et al. Impact of treatment completion, intolerance and adverse events on health system costs in a randomised trial of 4 months rifampin or 9 months isoniazid for latent TB. Thorax. 2010;65:582-7. [ Links ]
69. Kunst H, Khan K. Age-related risk of hepatotoxicity in the treatment of latent tuberculosis infection: a systematic review. Int J Tuberc Lung Dis. 2010;14:1374-81. [ Links ]
70. Kass J, Shandera W. Nervous system effects of antituberculosis therapy. CNS Drugs. 2010;24:655-67. [ Links ]
71. Snider Jr DE. Pyridoxina supplementation during isoniazid therapy. Tubercule. 1980;61:191-6. [ Links ]
72. Baciewicz AM, Chrisman CR, Finch CK, Self TH. Update on rifampin and rifabutin drug interactions. Am J Med Sci. 2008;335:126-36. [ Links ]
*Corresponding author.
E-mail address: rdmelo@med.up.pt (R. Duarte).
Received 10 August 2012; accepted 10 August 2012