Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.20 no.5 Lisboa set. 2013
https://doi.org/10.1016/j.jpg.2013.03.005
ENDOSCOPIC SPOT
Benign refractory esophageal stenosis treated with biodegradable stent: 18 months follow-up
Tratamento de estenose esofágica benigna refractária com prótese biodegradável: 18 meses de seguimento
Manuela Canhoto∗, Sandra Barbeiro, Filipe Silva, Bruno Arroja, Cláudia Gonçalves, Isabel Cotrim, Helena Vasconcelos
Department of Gastroenterology, Centro Hospitalar Leiria-Pombal, E.P.E., Leiria, Portugal
* Corresponding author
Treatment of esophageal strictures has evolved and biodegradable stents may be an easy alternative to plastic/metallic stents or multiple dilations.
The authors present a 43-year-old man treated with a biodegradable esophageal stent for refractory anastomotic stricture. The patient remained asymptomatic for 16 months after stent placement, without any intervention, with exception for proton pump inhibitor therapy.
The patient, a 43-year-old male, underwent partial esophagectomy for squamous cell carcinoma (T1N0) in February 2010. Three months later he developed dysphagia due to anastomosis stenosis (Fig. 1a).
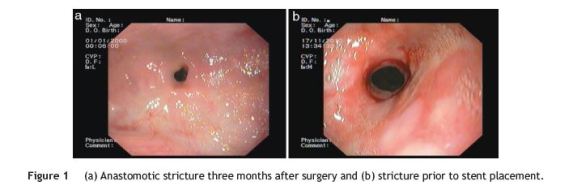
Multiple dilatation sessions (Savary-Gilliard dilators, TTS balloons) were performed every 2-3 weeks, with limited improvement (Fig. 1b). Betamethasone dipropionate injection (4 mg) was performed twice, also with no improvement. In November 2010 incisional needle-knife therapy was performed and later two additional dilation sessions, again with no satisfactory improvement.
Due to the patients weight loss and impact on quality of life, a biodegradable esophageal stent, SX-ELLA BD stent® 60×25mm, was inserted on April 2011 (Fig. 2a). There were no complications during or after the procedure.
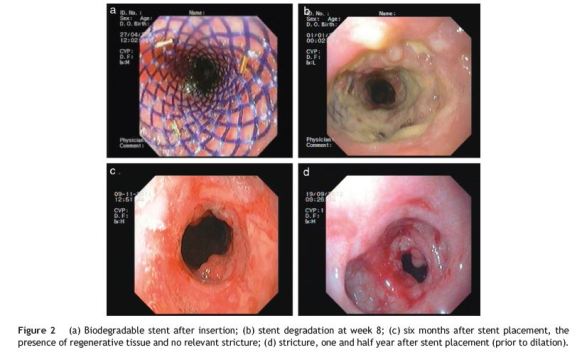
Eight weeks later he reported weight gain and no dysphagia. Endoscopy at this time revealed partial stent degradation (Fig. 2b) and lumen patency.
Six months later he remained asymptomatic (Fig. 2c).
Sixteen months after stent placement, the patient presented with dysphagia and stricture (Fig. 2d). Two dilation sessions were performed (TTS balloon, 14mm) and four months after the last intervention he remains asymptomatic.
Treatment of esophageal strictures has advanced in the last 30 years with stent development, from plastic tubes to flexible self-expanding metal (SEMS), plastic (SEPS) and new biodegradable stents (BDS).1
The SX-ELLA BD® is the first completely BDS. According to the manufacturer, the stent maintains its integrity for 6-8 weeks and begins its degradation at week 12. Stent degradation is accelerated in low pH (http://www.ellacs.eu/sx-ellastent-jicnovy-biodegradabilni-bd-stent.html).
For refractory benign esophageal strictures (RBES), the fully covered SEMS, although more expensive, may have fewer complications at stent removal, compared to SEPS.1 BDS do not need to be removed requiring fewer procedures and less complications than both SEPS and SEMS,2 offering na advantage, that could justify the highest price of all three stent types, specially for the patients who were already submitted to a considerable number of interventions.
BDS provided long-term relief of dysphagia in 33% (median follow-up of 166 days)2 to 45% (median follow-up of 53 weeks)3 of patients with RBES. A single BDS is only temporarily effective in most patients with RBES but sequential stenting may be an option to avoid serial dilations.4
As most of the cases and series reported concern highly refractory strictures, these features could be the cause of less satisfactory results and some authors propose that BDS could be more successful at an earlier stage.5
Although the BDS may be an easy alternative to repeat endoscopic dilation and other temporary stents, larger studies with longer follow-up are needed,3,5 including evaluation of efficacy, safety, patient satisfaction and costs.5
References
1. Hirdes M, Vleggaar FP, Siersema PD. Stent placement foresophageal strictures: an update. Expert Rev Med Devices.2011;8(6):733-55. [ Links ]
2. van Boeckel PG, Vleggaar FP, Siersema PD. A comparison of temporary self-expanding plastic and biodegradable stents for refractory benign esophageal strictures. Clin Gastroenterol Hepatol. 2011;9(8):653-9. [ Links ]
3. Repici A, Vleggaar FP, Hassan C, van Boeckel PG, Romeo F, Pagano N, et al. Efficacy and safety of biodegradable stents for refractory benign esophageal strictures: the BEST (Biodegradable Esophageal Stent) study. Endoscopy. 2012;44(7):649-54. [ Links ]
4. Hirdes MM, Siersema PD, van Boeckel PG, Vleggaar FP. Single and sequential biodegradable stent placement for refractory benign esophageal strictures: a prospective follow-up study. Endoscopy. 2012;44(7):649-54. [ Links ]
5. van Boeckel PG, Vleggaar FP, Siersema PD. Biodegradable stent placement in the esophagus. Expert Rev Med Devices. 2013;10(1):37-43. [ Links ]
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this study.
Confidentiality of data. The authors declare that they have followed the protocols of their work center on the publication of patient data and that all the patients included in the study received sufficient information and gave their written informed consent to participate in the study.
Right to privacy and informed consent. The authors have obtained the written informed consent of the patients or subjects mentioned in the article. The corresponding author is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
*Corresponding author
E-mail address: manela_vc@yahoo.com (M. Canhoto).
Received 17 January 2013; accepted 10 March 2013













