Serviços Personalizados
Journal
Artigo
Indicadores
-
 Citado por SciELO
Citado por SciELO -
 Acessos
Acessos
Links relacionados
-
 Similares em
SciELO
Similares em
SciELO
Compartilhar
Jornal Português de Gastrenterologia
versão impressa ISSN 0872-8178
J Port Gastrenterol. vol.21 no.1 Lisboa fev. 2014
https://doi.org/10.1016/j.jpg.2013.10.007
ENDOSCOPIC SPOT
Ischemic gastropathy: Early diagnosis and benign evolution in an elderly woman
Gastropatia isquémica: diagnóstico precoce e evolução benigna em mulher idosa
Manuela Canhotoa,∗, Sandra Barbeiroa, Filipe Silvaa, Bruno Arrojaa, Cláudia Gonçalvesa, Isabel Cotrima, Cristina Amadob, Helena Vasconcelosa
a Serviço de Gastrenterologia, Centro Hospitalar Leiria-Pombal, E.P.E., Leiria, Portugal
b Serviço de Anatomia Patológica, Centro Hospitalar Leiria-Pombal, E.P.E., Leiria, Portugal
*Corresponding author
The authors present the case of an 82 year-old female patient observed at the emergency department with upper gastrointestinal bleeding and abdominal pain.
The patient referred diffuse abdominal cramps and episode of coffee-ground emesis in the last 3-4 h. She denied any other abdominal, respiratory or urinary symptoms and the ingestion of non-steroidal anti-inflammatory drugs or corticosteroids and recent hospitalization or surgery. The patient had a chronic history of atrial fibrillation treated with amiodarone (200 mg qd). She also took omeprazole (20 mg qd) on regular basis.
She presented normal vital signs, level of consciousness and no fever. Cardio-pulmonary auscultation was normal, except for the presence of arritmic heart sounds. The abdomen was distended and tender especially at the upper quadrants with decreased bowel sounds. Rectal examination excluded melena, but the nasogastric aspiration returned a hematic gastric content. Blood tests showed leukocytosis, Hb 11.9 g/dL, and a CRP of 46 mg/L. Coagulation, platelet count, liver function tests, renal function and electrolytes were all within normal range. Plain abdominal film excluded perforation.
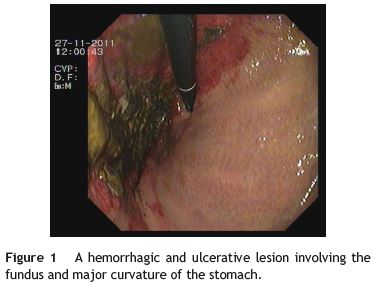
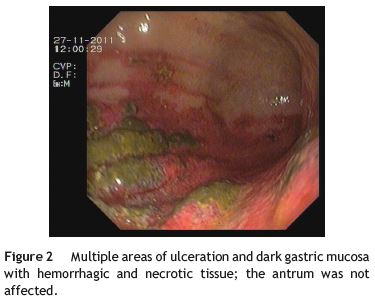
An upper endoscopy revealed an ulcerated hiatal hérnia with congestion, ulceration, and areas of apparent necrosis involving the distal esophagus, the gastric fundus (Fig. 1) and the proximal gastric body (Fig. 2), with no active bleeding. These aspects were compatible with acute ischemic gastropathy.
A computed tomography scan (CT) showed a normal aorta, celiac trunk and superior mesenteric artery. The CT also revealed gastric distension and gastric wall thickening with parietal pneumatosis and gas within the portal vein. She was admitted to the Gastrenterology ward and was started on i.v. antibiotics, after organic fluids were collected for culture. At day one at the ward, she presented with fever and elevated CRP of 155.9 mg/L, without an apparent focus of infection. The remainder days she showed clinical and laboratory improvement.
The urine culture identified an Escherichia coli infection. Blood cultures revealed no bacterial growth.
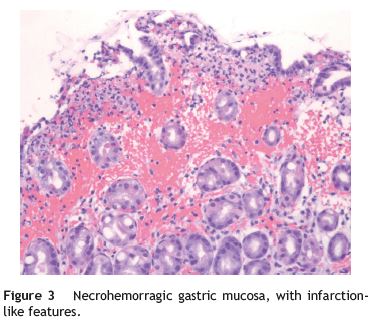
She was transfused with a total of 2 units of packed red blood cells. Samples obtained for histological evaluation were consistent with ischemia (Fig. 3).
Gastric necrosis is extremely uncommon as the blood supply of the stomach protects it from ischemia. Most frequently, it develops as consequence of acute gastric dilatation1 but can also occur after gastric surgery or therapeutic embolization.2 Mechanical factors can be implied in gastric dilatation and ischemia and infectious causes have been reported, generally involving immunocompromised patients (diabetes, neoplasia)3 and sepsis, as in the case described.
Necrosis might be partial (mostly in the lesser curve due to vascular supply) or involving the full organ.3 Emesis, abdominal pain and distension are common and initially mild, but rapid evolution to shock may occur.1,3 Plain abdominal films and CT are useful but endoscopy remains the gold tool for prompt diagnosis.2 A delayed diagnosis can be fatal.4 Patients should be treated conservatively with fluids and antibiotic unless perforation or septic shock develops, in which case gastrectomy is warranted.5
References
1. Steen S, Lamont J, Petrey L. Acute gastric dilation and ischemia secondary to small bowel obstruction. Proc (Bayl Univ Med Cent). 2008;21:15-7. [ Links ]
2. Papanikolaou IS, Foukas PG, Sioulas A, Beintaris I, Panagopoulos P, Karamanolis G, et al. A case of gastric ischemic necrosis. Endoscopy. 2011;43 Suppl. 2. UCTN:E342. [ Links ]
3. Vettoretto N, Viotti F, Taglietti LM. Giovanetti Acute idiopathic gastric necrosis, perforation and shock. Emerg Trauma Shock. 2010;3:304. [ Links ]
4. Richieri JP, Pol B, Payan MJ. Acute necrotizing ischemic gastritis: clinical, endoscopic and histopathologic aspects. Gastrointest Endosc. 1998;48:210-2. [ Links ]
5. Zerbib P, Voisin B, Truant S, Saulnier F, Vinet A, Chambon JP, et al. The conservative management of severe caustic gastric injuries. Ann Surg. 2011;253:684-8. [ Links ]
*Corresponding author
E-mail address: manela_vc@yahoo.com (M. Canhoto).
Ethical disclosures
Protection of human and animal subjects. The authors declare that no experiments were performed on humans or animals for this investigation.
Confidentiality of data. The authors declare that they have followed the protocols of their work centre on the publication of patient data and that all the patients included in the study have received sufficient information and have given their informed consent in writing to participate in that study.
Right to privacy and informed consent. The authors have obtained the informed consent of the patients and/or subjects mentioned in the article. The author for correspondence is in possession of this document.
Conflicts of interest
The authors have no conflicts of interest to declare.
Received 6 December 2012; accepted 29 October 2013













