Introduction
Leadership is considered a fundamental ingredient in management, influencing the results sensitive to nursing care (Nunes & Gaspar, 2016). The leadership and clinical nurse leader have been the target of several studies, since nurses, as leaders, are the key piece to communicate with the team and achieve objectives, with the purpose of the quality of care, the safety of the health innovation (Nunes & Gaspar, 2016; Baernholdt & Cottingham, 2011). Thus, this innovative role -clinical nurse leader - should be adapted around the world to improve the quality of care and safety of health systems (Baernholdt & Cottingham, 2011; Stavrianopoulos, 2012; OECD, 2017).
The present systematic review aims to analyze the scientific evidence about the efficacy of nurses in the development of competences associated with the practice of the clinical leader.
1. Background
Leadership in nursing plays a central role in quality care for to the client, which involves four fundamental activities: facilitating effective continuous communication; strengthening intra- and interprofessional relations; construction and maintenance of teams; and peer involvement (Baernholdt & Cottingham, 2011).
In order to evaluate the role of improving the quality of populations, evidence-based practice, and the thinking of health systems, Bombard, et al (2010) emphasize leadership and change (Bombard et al., 2010).
Bender (2016b) reports that positive results in the implementation of the clinical leader of nursing are fundamentally continuous improvement in the quality and results of health care. This author proposes an integrated model of care delivery, in which clinical nurse leader can positively influence the environment and quality of care (Bender, 2016a).
Baernholdt & Cottingham (2011) corroborate Bender by noting that the existence of a clinical nurse leader can further reduce readmission rates, improve financial gains, bridge communication gaps, improve labor, develop the critical thinking and decrease the turnover of nurses.
The nurse leader develops actions such as promoting, nurturing, testing, explaining, reexploring, analyzing and evaluating the cultivation of relationships, building relationships of trust, creativity and curiosity (Bombard et al, 2010; Houskamp, 2013).
2. Methods
This review was based on the methodology proposed by the Joanna Briggs Institute (JBI) for reviews (Peters et al, 2015), with the objective of "analyzing scientific evidence about the efficacy of nurses in the development of competencies associated with clinical leader practice".
Following the guidelines of this methodology, a preliminary exercise should be carried out before the systematic review, which consists of a primary search in databases of scientific articles and studies related to the theme under investigation. As such, an initial research was conducted on databases such as MEDLINE, CINAHL, JBI Database of Systematic Reviews and Implementation Reports and Cochrane Library and, revealing that there is no published review of the object under study.
2.1 Research objectives and issues
The objective of the systematic review was to analyze the scientific evidence about the efficacy of nurses in the development of competencies associated with the practice of clinical leader, focusing on the following questions: which competences are developed by clinical nurse leader? how are the transitions of this role carried out? how do clinical leaders feel?
The revision’s question was formulated based on the PCC strategy, where participants (P) were considered, nurses; Concept (C), clinical leadership of nursing; Context (C), all contexts of health care delivery.
2.2 Inclusion criteria
For the preparation of this review, the following inclusion criteria were considered:
-
Participants
Studies with nurses of all age groups, from all areas of specialty and professional development and who perform coordination functions at a microsystem level;
-
Concepts
Studies that address the concepts of clinical leadership of nursing, competence and experience of the clinical nurse leader.
-
Context
Studies where all care contexts are included: hospitals, primary health care, integrated continued care, nursing homes and others, in order to obtain and gather as much information as possible;
-
Type of studies
Studies of primary research, quantitative or qualitative design, as well as systematic reviews of the literature, literature reviews and relevant expert opinion articles.
2.3 Research strategy
For this review, a three-step research strategy was used. In the first stage, a research was carried out in the electronic databases CINAHL and MEDLINE, followed by an analysis of the words inserted in the title and summary of the articles identified as well as the indexed terms present in them. Subsequently, a second analysis was performed on the remaining databases of the EBSCOHost platform using all keywords and indexed terms. Thirdly, additional studies identified in the bibliographic references of the selected articles were researched. Then, two reviewers independently examined the full-text articles to verify the inclusion criteria following the guidelines of Levac et al (2010). It was not necessary to review a third reviewer, since there were no disagreements.
The established time limit was extended due to the little evidence on this theme. Thus, the period between 2010 and 2019 was defined. The terms used were those defined in the PCC (Participants, Concept and Context) that is, clinical nurs* leader, nurs*, clinical leader* for participants. The terms indexed were clinical nurs* leader, nurs*, clinical leader*. For the Concept we used the words trust, competence, effectiveness and in English, confidence, practical competence, efficacy. For the context, and being a recent role for nurses was intended to obtain maximum scientific evidence in any context of care such as: hospitals, primary health care, integrated continued care, residential structures of the elderly, using the terms in English, hospital, primary health care, long term care, nursing home*.
The information sources/databases consulted were CINAHL Plus with Full Text, Medline with Full Text, Cochrane Central Register of Controlled Trials, Cochrane Database of Systematic Reviews, Cochrane Methodology Register, Scopus, Library, Information Science and Technology Abstracts, Epistemonikos. A survey of unpublished documents was also conducted: ProQuest - Nursing and Allied Health Source and RCAAP - Scientific Repository of Open Access of Portugal Full Article.
2.4 Data Extraction
The data extracted from the articles were aligned with the objectives and research questions and their instrument indicated by the analysis methodology developed by the Joanna Briggs Institute (Peters et al, 2015). Both reviewers independently examined the first five studies using the data form, and then met to determine whether the approach to the extracted data is consistent with the research in question (Levac et al, 2010).
3. Results
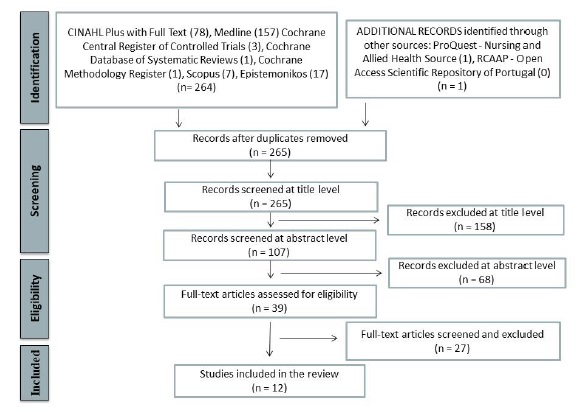
After removal of duplicate articles, 265 articles were identified for review selection. A total of 39 articles met the inclusion criteria based on the verification of titles and abstracts. The full-text articles were then read and examined and twelve met the inclusion criteria of which nine exclusively in the hospital context and three in all contexts of health care delivery.
Figure 1 specifies the results of the analysis steps, following the PRISMA Flow Diagram model (Moher et al, 2009).
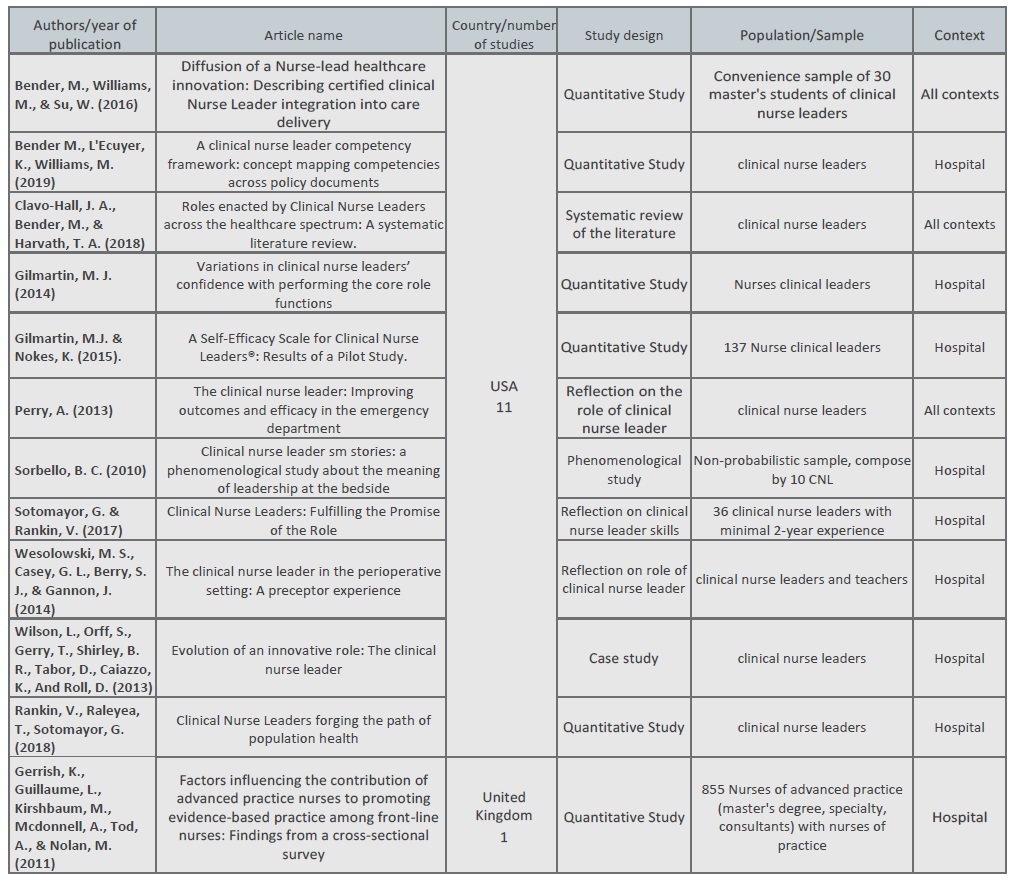
We also carried out a qualitative analysis on the selected articles, considering the following characteristics: Country of publication; Study design; Year of publication (All studies were published between 2010 and 2019. Two articles from 2010, two from 2013, two from 2014, one from 2015, one from 2016, two from 2017, one from 2018 and one from 2019); Context development of the study; Competencies developed by the clinical nurse leader (All studies presented the competencies that are developed by the clinical nurse leader as well as what differentiates him from the rest of the team); Transition of the role of clinical nurse leader (nine of the twelve articles demonstrate the transition of the role of the clinical nurse leader); the clinical nurse leader efficacy (the twelve articles included in the review, seven describe the development of the practice of clinical nurse leader, exposing facilitating and embarrassing factors to his/her development. Two articles develop a scale of evaluation of nurse perception as clinical nurse leader).
Table 1 shows the overview of the articles included in the review.
4. Discussion
In this review, twelve studies were included, including primary studies, a literature review and three reflection studies, thus meeting the inclusion criteria.
This work responds to the need for reviews on the effectiveness of the development of competencies associated with clinical leader practice. It becomes clear that the effectiveness of clinical nurse leaders enhances performance and consequently improved health care outcomes (Baernholdt & Cottingham, 2011; Bender, 2016 b, Gilmartin, 2014, Rankin, 2018).
This research also fills a gap in the transition of clinical nurse leader practice, including the characteristics identified, as well as facilitating and embarrassing factors. The contexts’ diversity of the practice of care of the articles analyzed - nursing homes, hospital, primary health care, academic - and their characteristics allow a better understanding of this theme.
Regarding the skills developed, Sorbello (2010) says that the clinical nurse leader knows the client as a person, keeps him safe, is proud of his achievements and the respect obtained by others, besides being a lawyer. This description is corroborated by Perry (2013) and Rankin, Raleyea & Sotomayor (2018), adding that clinical nurse leader sits as the client's lawyer, fights care fragmentation, serves as a unifier among different disciplines, improves safety, has critical thinking, has a good communication ability to strong evaluation skills, as well as compassion, intelligence and trust. Wesolowski et al (2014) also adds that in addition to an advocate, the clinical nurse leader is also a member of a profession, a team leader, an information manager, a systems analyst, and a professional capable of preventing risks, without ever failing to be a clinician. He is also a results manager, an educator and an eternal apprentice (Bender, L'Ecuyer & Williams, 2019). The intelligence and ability to work with others under stress are characteristic also described by Sotomayor & Rankin (2017). The clinical nurse leader should not only have a vision for function and ability to measure the impact of care, as well as critical thinking and ability to review customer outcomes, besides being able to teach and implement changes and practices based on scientific evidence (Sotomayor & Rankin,2017; Rankin, Raleyea & Sotomayor, 2018). In this way, clinical nurse leader anticipate, assess and mitigate risks, always having a strategy in mind, and are still able to solve system problems, involve stakeholders, and realize what is sustainable to change (Clavo-Hall, Bender, & Harvath, 2018; Sotomayor & Rankin 2017). These are significant and relevant changes in view of daily challenges, they can develop evidence-based knowledge and best practices while exploring solutions with the health team. Innovative approaches and the assessment of paper effectiveness, clinical outcomes and financial savings are some of its goals (Wilson et al., 2013; Sotomayor & Rankin, 2017; Rankin, Raleyea & Sotomayor, 2018).
To achieve these results, clinical leadership skills are highlighted where communication skills, trainer (information manager) collaboration and team coordination (team leadership) are essential for managing the care and resource management environment (Bender, L'Ecuyer & Williams, 2019). Bender, Williams & Su (2016) as well as Clavo-Hall, Bender & Harvath (2017) focus on a type of leadership - transformational - as well as exemplary professional practice and new knowledge, highlighting innovation. In short, he is a nurse of advanced practice who develops essential thought and critical evaluation skills to promote evidence-based practice. They subsequently use evidence to support decision-making regarding customer care, as well as to influence the team and organizational practices. The clinical nurse leader works at the unit level (clinical microsystem level) responsible for coordinating disciplines, managing clinical outcomes, with a special focus on health promotion and disease prevention in populations and implementing programs to improve clinical quality and risk management.
Thus, the essential competencies of clinical leader nurse practice are organized into three domains: (a) nursing leadership in care management, (b) management of clinical results to promote evidence-based practice and clinical decision-making and (c) promotion of quality and clinical safety (Gerrish et al., 2011; Gilmartin & Nokes, 2015; Gilmartin, 2014).
Regarding efficacy as a clinical nurse leader in their function, only seven articles correspond to this dimension. Wesolowski et al (2014) report that clinical nurse leader and their teachers have launched themselves into the learning experience confident of their performance. Sorbello (2010) adds that clinical nurse leader needs to be recognized, understood and affirmed. However, Clavo-Hall, Bender & Harvath, (2017), points out that many clinical nurse leaders perform the functions informally for which they are entitled or designated, which leads to decreased confidence in the role. On the other hand, they also fear that their role will be taken from the customer's headboard, diluted with additional projects, or eliminated as a result of economic constraints within their organizations, thereby diminishing their confidence in the performance of their function. Nurses of advanced practice with master's degree feel more effective in their ability to support colleagues and evidence-based practice. Clinical leadership is a complex process of managing relationships at the microsystem level to facilitate the restructuring of care delivery processes. Without self-efficacy and skills such as communication, advocacy and the ability to tune into multiple perspectives, a clinical nurse leader cannot properly perform the functions, such as coordination of multidisciplinary care in healthcare environments (communication and effective management) (Bender, L'Ecuyer & Williams, 2019).
Gilmartin mentions that self-confidence is an important predictor of successful career transitions, that is, it is important to trust clinical nurse leaders in their ability to act on paper, promoting improved performance, as well as job satisfaction and retention of nurses who perform this innovative role of clinical leadership (Gilmartin, 2014). Gilmartin & Nokes (2015) presents a scale of evaluation of the self-efficacy of clinical nurses’ leader - CNLSES®, offering a tool to measure the effectiveness of nurses with the performance of basic competencies associated with the role. These authors state that the transitions of the work role involve two interdependent adjustment processes: personal development and role development. The practice of clinical nurse leader, by definition, requires individuals to make career transitions, increasingly complex. Hiring clinical nurse leaders is an effective approach for organizing nursing care, maximizing research and influencing ways of providing care for all professions in the microsystem. This transition is an ongoing process, in which age, academic degree and professional experience can be a catalyst for change and wisdom (Gilmartin, 2014; Bender, Williams & Su, 2016; Bombard et al,2010).
Considering that advanced practice nurses are positive about their ability to promote evidence-based practice, there is a need to improve support, to help them overcome the barriers they face, such as work overload and lack of time and resources (Gerrish et al, 2010), as well as the balance between exits and opportunities. They easily identify where they could make additional contributions to the client, profession, organization and community (Wilson et al, 2013). Thus, it is important that institutions support their professions, be knowledge organizations, allowing nurses to empower themselves not only, but mainly to clients and their own organizations (Perry & Ca, 2013). The longer the nurse is performing their function in the unit, the greater the perception of transformational leadership practices, improving the ability to improve quality, cost and safety. The training of clinical nurse leader positions nurses for clinical leadership in the microsystem and mesosystem levels (Sotomayor & Rankin, 2017; Bender, L'Ecuyer & Williams, 2019).
Conclusions
These clinical nurse leaders are the new innovative role and are developing skills and transition processes. They are prepared to fulfill a strategic position in health teams both inside and outside the microsystem. They are trained to identify clinical outcomes and associated cost, contributing to improved safety, efficacy, efficiency, quality of care and customer focus. Advanced practice nurses are well positioned as clinical leaders to promote evidence-based practices and to exercise effective clinical leadership in both micro and mesosystem.
The qualitative results reveal the perception of a complex role and polarity at multiple levels (organization, unit, team and among nurses). Quantitative results suggest that the longer the clinical nurse leader is exercising in the unit, the greater the perception of transformational leadership practices that lead to the improvement of the quality of nursing care, with results in the customers and the shift to innovative practices.
Self-efficacy is one of the main concepts of successful role transition, job satisfaction and performance. Thus, evaluating the self-efficacy of clinical nurse leaders throughout their practice will be fundamental for the provision of care and for the management of units and organizations, to the extent that they improve the performance of these professionals with consequences in increasing the quality of care, customer safety and the other results of care units and health organizations.
The clinical nurse leader can bring new light to issues that include fragmentation of care, overcrowding and care outcomes. However, the flexibility and extensive investigation of this role allows for its use across practice settings and represents an exciting allows its use in all contexts of care practice and represents an excellent opportunity for nursing to drive quality of care to new levels while managing for nursing to direct the quality of care to new levels, and in parallel manage the resources placed at its disposal.