Introduction
The tibiotarsal joint is considered one of the most fundamental articulations of our body, conditioning the movements of the leg, and being indispensable for the human march. The most frequent injuries that affect the tibiotarsal joint are sprains and fractures and it is estimated that ankle sprains are the most common musculoskeletal injury, accounting for 16-21% of injuries (Kulunkoglu & Celik, 2019).
Lateral ankle sprains are not benign but are rather injuries that can negatively influence the long-term health and well-being of patients through the development of chronic ankle instability (CAI). The prevalence and impact of CAI in adolescent athletes are unknown. To better develop and justify prevention strategies of lateral ankle sprains and CAI, it is important to understand the origin, the associated long-term impact of CAI within populations other than adults, early diagnosis and appropriate rehabilitation of ankle injuries (Donovan et al., 2020).
The use of medical devices should enable the health professional to control the movement to be performed, in terms of direction, amplitude and muscle strength, allowing each parameter to be adjusted to the different phases of rehabilitation, always rigorously and efficiently and not putting the patient at risk during the exercises (Chang & Zhang, 2019).
Rest, ice, compression, and elevation (RICE) are early self-intervention methods for treating inflammation after trauma, such as acute ankle sprain. Inflammation causes pain and edema, which can limit the patient's ability to perform the rehabilitation required for proper healing. Gentle tension and stretching at the joint promote proper ligament fiber growth into tight, parallel strands. Accumulation of fluid and edema around an injury site also increases tissue damage, delays healing, and can result in some degree of chronic disability (van den Bekerom et al., 2012).
Patients with CAI commonly display lower levels of self-reported function and health-related quality of life (Walsh et al., 2020). Joint mobilization appears to be beneficial for improving dynamic balance immediately after application, and dorsiflexion range in the short-term. Long-term benefits have not been adequately investigated (Weerasekara et al., 2018).
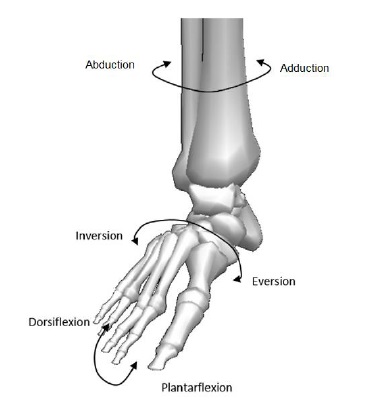
For the effective rehabilitation of this joint, there are crucial factors to be controlled, such as the degree of amplitude of each movement and the monitoring of the resistance to be applied in each exercise, taking into account that these variables are dependent from individual to individual. The process of rehabilitation of patients with this type of lesions involves repeating the six movements made possible by the tibiotarsal joint (figure 1). The reference position of the ankle, or neutral position, is when the foot is perpendicular to the axis of the leg. From this position, the ankle joint performs flexion and extension movements (dorsiflexion and plantar flexion, respectively), abduction and adduction, and rotation (inversion and eversion). Due to muscular, bone and ligament factors, the movements of the ankle have limited range of amplitude. This range is also influenced by daily and sports activities and gender (Brockett & Chapman, 2016).
In this study it is proposed to carry out the study of an existing prototype equipment, the Therapheet, where an analysis of its structure, functions and mode of operation will be undertaken. Its components and systems will also be identified and analyzed, as well as the relationships between the various components and their individual functions. This approach allowed us to propose improvements that met a set of requirements in order to obtain a unique tibiotarsal joint rehabilitation device that makes a positive difference in the lives of patients with ankle injuries and on the health professionals who treat these injuries daily.
1. Methods
1.1 Study type
This study presents a review of the tibiotarsal joint rehabilitation protocols, as well as the classification of devices used for this purpose. Thus, the purpose is to improve the Therapheet, developed at the Department of Mechanical Engineering of the University of Minho, obtaining a viable, functional and safe rehabilitation device, standing out from the rest on the market, since it allows the execution of the six rehabilitation exercises.
1.2 Objectives
This work aims to obtain a feasible, functional and safe rehabilitation device, standing out from the rest in the market as an added value in the rehabilitation of ankle injuries.
1.3 Procedures
The equipment will be preliminary tested and its operation will be based on the use of Graphe Fonctionnel de Commande, Étapes Transitions (GRAFCET) command specifications, controlling the sequences of each rehabilitation exercise, in order to obtain an automated control system. Subsequently, the device will undergo some changes, from where a new phase of testing will be carried out, using volunteers, in order to obtain feedback from several users.
The aim of this project is to propose improvements, according to a design methodology, that fulfill a set of requirements to the device, making it an instrument with more satisfactory results for the patient, and a more useful and positively differentiated option in the market. However, only some of these phases will be the subject of a more detailed study throughout this article.
2. Rehabilitation program for ankle injuries
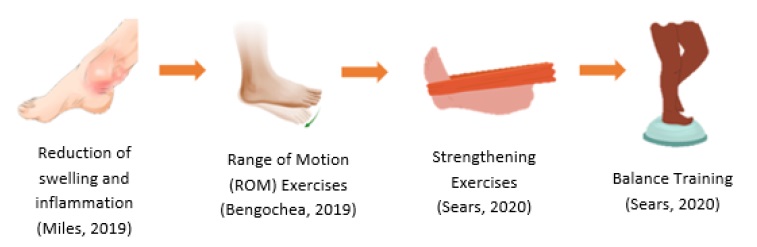
The general rehabilitation program for ankle injuries is shown in figure 2 . The initial stage of treatment right after injury is considered the acute phase of rehabilitation and is focused on reducing swelling and inflammation to promote healing of the injured tissues. A reduction in inflammation can be achieved with elevation, application of ice and compression. The affected ankle is also often immobilized. However, prolonged immobilization of the ankle can lead to reduced Range of Motion (ROM) and muscular atrophy (Tsoi, 2011).
The next phase of ankle rehabilitation typically involves ROM and muscle strengthening exercises. With reduced swelling, the rehabilitation enters into the subacute phase where active and passive ROM exercises are normally carried out within the pain-free range of the patient to improve the range of motion and reduce muscular atrophy. This has the ability to stimulate healing of torn ligaments (Tsoi, 2011).
The chronic phase (functional phase) is achieved once pain free weight bearing gait is possible. During this phase, ROM exercises are continued together with the beginning of muscle stretching and resistive exercises. The resistance level of these strengthening exercises should be increased as the patient progresses with recovery. Muscle stretching is important to assist the recovery of joint ROM while resistance training is used to improve the strength of muscles surrounding the ankle to prevent future injuries. Finally, proprioceptive and balancing exercises should be carried out towards the end of the rehabilitation program to enhance the patients’ sense of joint position, thus giving them better foot and ankle coordination and improving their ability to respond to sudden perturbations at the ankle (Tsoi, 2011).
As can be seen from the previous review, muscular strength and good proprioception are vital in preventing functional instability in the ankle. Emphasis must therefore be placed in these areas and an extensive rehabilitation program is needed to minimize the likelihood of recurrent injuries. The repetitive and tedious nature of such exercises therefore makes robotic devices an attractive alternative to manual manipulation. However, the great variability observed between different patients due to either their level of injury or their ankle characteristics, such as joint limits and stiffness, also means that any robotic device employed in this area must be adaptive to allow it to cater for the requirements of specific patients (Tsoi, 2011).
3. Ankle rehabilitation robot classification
Physical therapy is used for rehabilitation of patients dealing with musculoskeletal and neurological problems (Hussain et al., 2017). Traditionally, ankle injuries are rehabilitated through physical therapy, however, evidence suggests that without sufficient rehabilitation, 44% of people will have future problems. During rehabilitation treatment, cooperative and intensive efforts by therapists and patients are required during prolonged sessions (Zhang, 2016).
Conventionally, elastic bands, foam rollers and oscillating plates are widely used in physical therapy (Alcocer et al., 2012). However, these methods contain many limitations, such as inconsistency in treatment due to long repetitive and monotonous training sessions, and subjectivity in therapeutic procedures, often based on perception rather than objective clinical evaluation (Hussain et al., 2017). This results in the need for effective new rehabilitation techniques without increasing staff resources and burden. Robotics can deliver a transformation of rehabilitation clinics, switching from labor-intensive to technology-assisted operations, which can provide a rich flow of data that can facilitate patient diagnosis, therapy customization and keeping patient records at home or at the clinic (Hussain et al., 2017).
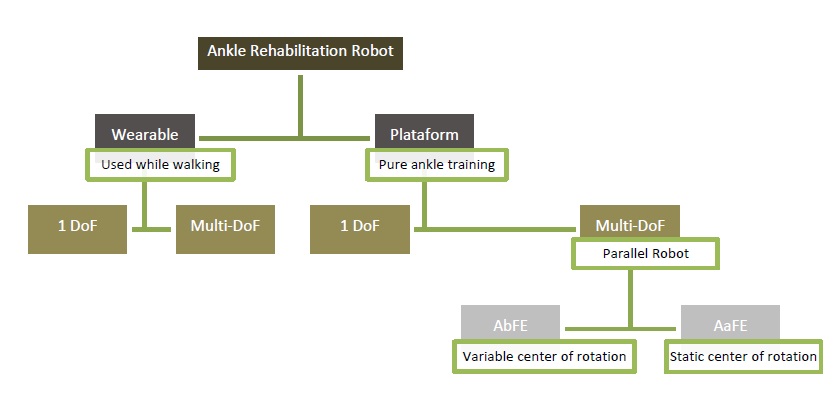
Most robot-assisted ankle rehabilitation techniques allow to improve ankle performance or gait function. These robotic devices can be divided into two categories: wearable device and platform-based parallel robots. Wearable devices generally take the form of a robotic orthosis or exoskeleton, intended for rehabilitation during gait training on a treadmill or ground. Platform-based devices typically have a fixed and mobile platform and are used for ankle training and worn by patients in a sitting position (Hussain et al., 2017; Miao et al., 2018). Both can be split into single or multiple Degrees of Freedom (DoF) devices. Devices with a DoF are usually driven by a rotary motor, while robots with multiple DoF are usually based on parallel platforms driven by linear actuators. In addition, multi-DoF platform-based rehabilitation robots fall into two categories based on their centers of rotation: actuators below the final effector (AbFE) and actuators above the final effector (AaFE). Specifically, robot systems containing AbFE require variable ankle joint positions and synergistic movements of the patient's lower limb during training, once the robot's center of rotation does not coincide with the ankle joint. On the other hand, on AaFE devices the patient can keep the ankle still and totally relaxed. From this point of view, the parallel manipulator (robot's center of rotation coincides with the ankle joint) is most suitable for ankle rehabilitation (Zhang, 2016). A robot classification scheme for ankle rehabilitation can be observed in figure 3. Therapheet can be classified as a multi-DoF plataform-based AbFE robot.
4. The therapheet device
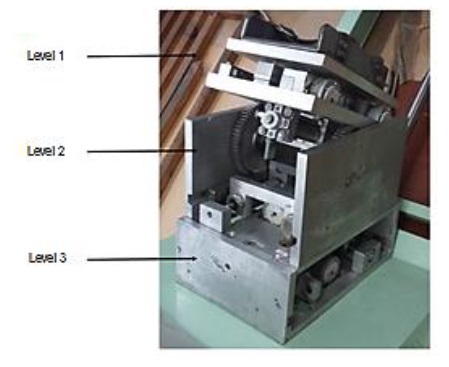
Therapheet is organized in an aluminum alloy 6061 structure, composed by three levels. In order to perform the required six ankle movements, this device contains different components in each level (see figure 4).
Level 1 performs the adduction and abduction exercises and also incorporates a platform to hold and fixate the foot during the rehabilitation process. This level enables a maximum value of 36° of movement amplitude. Level 2 admits the movements of dorsiflexion and plantarflexion, and enables a maximum amplitude of 45°. Finaly, the third level enables the inversion and eversion movements and admits a maximum amplitude of 25°. Illustration 1 depicts all the admissible movements possible to achieve with the Therapheet device; for the sake of completeness it must be referred that only the extreme positions of each pair of movements are shown in the figures of illustration 1.
The operating mode of the Therapheet is based on the use of pneumatic technology, in particular with the use of pneumatic cylinders, with a maximum operation pressure of 6 bar. The regulation of the stroke of the pneumatic cylinders is carried out in two ways, based on: (1) internal limitations, and (2) external limitations. The internal limitations are defined by the maximum stroke of the pneumatic cylinders selected specifically for this application, while the external limitations are defined by mechanical stops, strategically incorporated in the device, which restrict the stroke of the pneumatic cylinders.
Level 1 includes a rotary pneumatic actuator, a rotation platform and two linear tables engaging two stepper motors. Levels 2 and 3 incorporate two actuators in each level in symmetrical positions in order to obtain two-way movements and the intended operation is achieved by fixing one of the actuators and moving the other one to perform each exercise. In addition to the use of pneumatic cylinders, the operation of the Therapheet device is also supported by several other fundamental components such as linear tables, rack and pinion sets, linear guides, magnetic contact sensors and mechanical contact sensors.
In a simplified way, the operation of the Therapheet device consists of controlling the air pressure and its flow rate inside each actuator. In turn, each actuator is connected to a solenoid valve, and the control of compressed air at all levels is carried out by one Programmable Logical Controller (PLC) that carries out the opening or closure of all solenoid valves (electrovalves) (Ribeiro, 2014).
The Therapheet device was originally designed to support passive mobilization and resistive mobilization. That is, in a first stage of treatment, the device would perform the rehabilitation exercises in which the patient would not have to exert any force on the device (passive mobilization). In a second phase of treatment, the patient would be moving the device resistively, that is, by applying force on the device (resistive mobilization), allowing a complete rehabilitation. Moreover, the Therapheet was designed with the intention of allowing a control and graduation of the movement amplitude of each exercise, establishing a neutral position, and promoting the repeatability of the exercises to be performed. The Therapheet only allows to restore the ROM and muscle strength, not allowing the execution of proprioception exercises and balance training.
5. Project phases
A first phase of preliminary testing was carried out on the Therapheet device. These results enabled the identification of several drawbacks not consistent with the requirements needed for such a rehabilitation device. These drawbacks were the sudden movements of the Therapheet, resulting from its high mass, as well as several other dysfunctions associated with the implemented pneumatic technology. On the other hand, the device did not present an automated control system and, for this reason, it became crucial the implementation of a system suitable for controlling the device and the rehabilitation procedure.
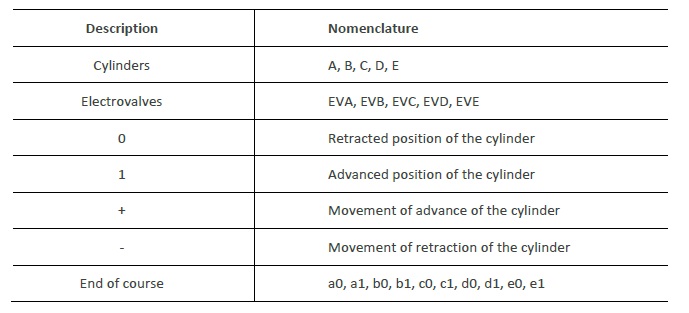
In this sense, the sequences of the rehabilitation movements were specified in GRAFCET (according to the IEC 848 standard) and, based on these sequences and in a previous research work (Cruz, 2018), the control of the implemented electropneumatic circuit was developed in a programmed logic, through a programmable logic controller (figure 5 ). For the GRAFCET command specification, in order to proceed to the device operation, it was necessary to consider the input and output information of the system. The inputs represent the information from the system, being, in this case, the sensors and, for reasons of simulation, the selectors of the types of exercises to be performed. The Therapheet device also incorporates six mechanical sensors and two magnetic sensors. For a safe and reliable operation, it is necessary to confirm the advanced and retracted position of the cylinders piston rods during each exercise. To make the simulation possible, sensors were placed at the end of the course of each cylinder piston rod to detect these positions. The outputs of the system correspond to the actuation of the electrovalves that control the pneumatic cylinders to carry out the rehabilitation process. Each cylinder is controlled by a solenoid valve; therefore the equipment operation is controlled by five solenoid valves. Illustration II presents the nomenclature used to define the GRAFCET representations of each movement of the Therapheet device.
To further improve this rehabilitation device an objectives tree was established (where the main goals were set for the Therapheet device in terms of safety, equipment features, how it is used and its production method), as well as a morphological map (where it was possible to consider several solution options to solve the problems determined during the preliminary testing phase of the device).
In this way, and to complement the pneumatic control of the device operation, for example, flow regulators were implemented in the feed tubes of the pneumatic cylinders, in order to smooth the movements of the whole device (figure 6 ).
After all these improvements, the device was subjected to a new testing phase, using healthy voluntary users of different gender and ages. Based on these tests and on the obtained results, it was necessary to verify if the modifications made to the device were appropriated or if any more changes were necessary to be considered, as well as to verify if the overall concept is the most adequate to fulfill the requirements and specifications set for the Therapheet.

Figure 5 GRAFCET representation of the combinatory movements of abduction and adduction, using the Automation Studio software (Cruz, 2018).
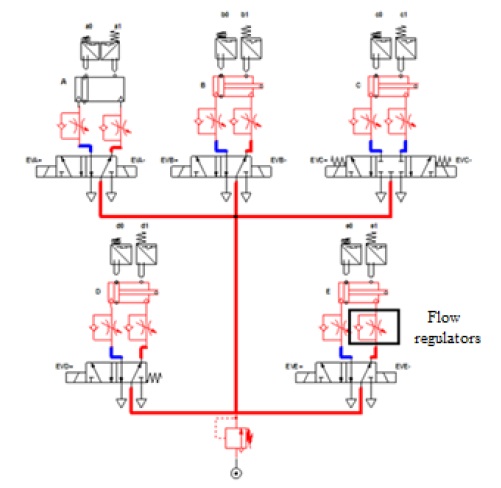
Figure 6 Pneumatic circuit implemented in the Automation Studio software for simulation (Cruz, 2018).
In this sense, the main objective of this project is to obtain a functional device that meets all safety requirements, that is, the equipment must perform the six ankle rehabilitation exercises correctly, namely the exercises of abduction, adduction, dorsiflexion, plantar flexion, inversion and eversion, in order to achieve a complete and efficient patient recovery. The safety of the patient recovery process is really an important requirement during the operation of the device, this is, the operation of the device should be smooth and exhibit non-abrupt movements in order to promote a safe rehabilitation. Patient comfort is also a major factor that must be ensured. He or she should feel safe and protected during rehabilitation sessions and should feel comfortable and confident in using the rehabilitation device. The appearance and the easy operation of the device is also an important aspect regarding the overall satisfaction of the patient. After the rehabilitation session, the patient should feel satisfied with the procedure, being also confident that the rehabilitation process has been evolved correctly.
6. Final remarks and future work
After the introduction of the automated control system and all the other improvements, the results obtained from the new tests carried out shown that the device is not yet adequate or functional for rehabilitation purposes.
The main problem of this device is its mechanical structure, comprising a series of components not yet optimized, causing some mechanical problems, such as sudden movements associated with high inertia that impairs its smooth operation, causing an unstable neutral position and noise.
The tests performed with the volunteers demonstrated that the foot placement platform needs to be adjusted in order to enable a more stable and adaptable foot attachment to each user. Taking into account the results obtained by voluntary users and considering all the analysis carried out throughout this project, it can be assumed that the device is not yet reliable, derived from the pneumatic system which is not the ideal actuation system to be implemented on such kind of device. The pneumatic system does not maintain a precise speed of movement, especially under variable load conditions.
The use of the flow regulators is also not the most adequate, since its application must be considered with or without an applied load. Moreover, this needs to be considered with the working pressure of the device: when the foot is placed on the rehabilitation platform, there must be a higher working pressure than the one when there is no loading on the platform, in order to counteract the force exerted by the foot, even in a passive movement. This means that the device loses motor torque in relation to the force exerted by the user's foot, requiring therefore a working pressure of at least 6 bar.
Conclusions
The analysis and discussion of the obtained results also suggest the need for a reengineering of the device, with the modification of its mechanical components and the pneumatic (actuation) technology, which also includes the design of an adequate controller to obtain a feasible final product. Besides these two aspects, it will be necessary to test the usability and ergonomic adaptability of the device with possible end users. During this process of improving the device, an ergonomic approach will be crucial so that the final solution is adaptable and comfortable for end users, allowing, from a biomechanical point of view, the adoption of correct postures. The ergonomic reassessment and verification of the suitability of the device for the patient for rehabilitation purposes must be carried out by performing preliminary clinical trials of the device and tests in a simulated environment with patients.
In terms of execution of the rehabilitation exercises, the equipment proved to be effective, correctly performing the six rehabilitation exercises of the tibiotarsal joint and with different amplitudes, which are only regulated manually.