Introduction
The World Health Organization considers urinary incontinence to be a public health problem that mostly affects women and consequently compromises their quality of life. Some people still see this pathology as a natural consequence of age and adapt to the changes imposed by it. Nowadays it is known that it is not just a natural consequence of age, as it can also appear in young people, including nulliparous women and athletes.
1. Theoretical framework
The important role of the pelvic floor muscles (PFM) is to support the pelvic organs, continence and childbirth (Karim, Begum et al. 2019). Continence is a complex mechanism, involving the coordination between the PFM, the urethra, the bladder and their supporting ligaments. This mechanism involves both striated (voluntary control) and smooth (involuntary) muscles (Bø 2004) The aim of this study was to describe the dynamic changes in the pelvic floor in elite nulliparous athletes.
2. Methods
2.1 Sample
This study, reporting the PF function by translabial 2D/3D ultrasonography in a sample of 8 athletes, volunteered to participate in the study. All athletes were active in the first league of their various sports and at the time of testing had been training for a minimum of 5 years, having reached a national or international level of competition. In this research note, the sociodemographic and anthropometric data were collected using a structured questionnaire. The inclusion criteria were elite nulliparous athletes trained or qualified in a particular sport, between 18 and 30 years old. The exclusion criteria were the inability to perform a correct PFM contraction, combination of multiple sports and surgical treatment of gynecological and urological illnesses.
2.2 Data collection instruments and procedures
The sports included were: volleyball (1), swimming (n=1), karate (n=1), gymnastics (n=1), horsemanship (n=1), pentathlon (n=1), javelin throw (n=1) and sprinting (n=1). Ethical approval was obtained from the Ethics Committee of the Hospital center of Trás-os-Montes and Alto Douro, Vila Real, Portugal (165/2018). All participants gave informed written consent. The evaluation and imaging were performed using GE Voluson 730 pro and were carried out by an experienced doctor, who did not have access to all the clinical information. All athletes were imaged in a supine position, after voiding. Imaging was performed in the mid-sagittal plane with the angle of acquisition set at 90º. The posterior vesico-urethral angle was acquired at rest and during a Valsalva maneuver. The most effective of at least three maneuvers was used for evaluation. The descent of the pelvic organs was assessed during the Valsalva maneuver. The levator hiatus was measured at rest, during the Valsalva maneuver and MVC of PF.
3. Results
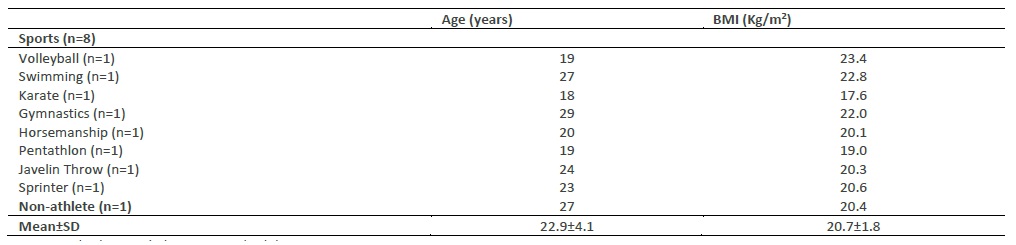
The results from the questionnaire indicate that all were asymptomatic for SUI or gynecological disorders. Eight international female league players, of different sports (age, 22.4±4.1 years and body mass, 20.7±1.9 kg) (Table 1)
Concerning the 2D ultrasound, the findings were the following: the PVU angle measurements were similar, showing no difference between them, either at rest or Valsalva. Only the karate athlete has urethral hypermobility because her value during the Valsalva maneuver was 164.40º, although it was asymptomatic. The results of bladder neck descent, relative to the symphysis pubis on maximum Valsalva demonstrate that the most favorable value was in volleyball, with no movement/descent of the bladder, while the worst value was in the javelin throw (still this value is within normal). Three athletes presented a mild rectocele, javelin throw, gymnastics and swimming modalities (Table 2).
Concerning the 3D ultrasound evaluations: the area of the levator hiatus at rest, the Valsalva and the MVC were measured. At rest, the lowest value was in pentathlon and the highest value was in javelin throw. For the Valsalva maneuver, the javelin throw athlete showed the highest value and the pentathlon obtained the lowest value. Regarding the MVC, the lowest value was in gymnastics and the highest value was in volleyball. As for the LAM assessment, no participant showed LAM avulsion. A paravaginal defect was detected in than half of the sample (n= 4). The athletes with the defect were in volleyball, horsemanship, pentathlon and sprinting (Table 2). There were no changes in normality with respect to the levator hiatal area and LAM avulsion (Figure 1).
Table 2 Biometric indices of the sui, pop, levator hiatos area, lam avulsion and paravaginal defect
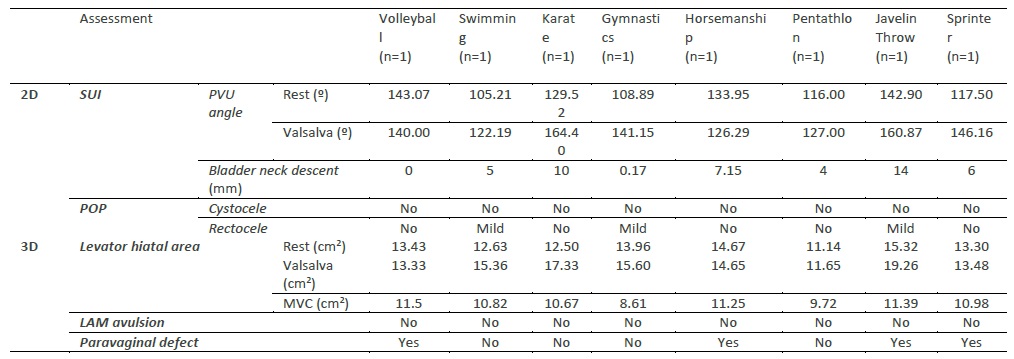
Note. 2D, two-dimensional ultrasound; 3D, three-dimensional ultrasound; LAM, levator ani muscle; MVC, maximum voluntary contraction; POP, pelvic organ prolapse; PVU, posterior vesico-urethral; SUI, stress urinary incontinence.
4. Discussion
Previous studies using 3D ultrasound imaging had evaluated functional and morphological parameters of young nulliparous athletes, such PF trauma and distension of the levator hiatos (Dietz 2019). Kruger et al (Kruger, Dietz et al. 2007) found the levator hiatal area at rest, 12.71±2.49 cm2 in the high-impact, frequent intense training (HIFIT) group and 12.77±2.43 cm2 in the control group. Found the levator hiatal area on valsalva, 21.53±9.98 cm2 in the HIFIT group and 14.91±7.18 cm2 in the control group. Found the levator hiatal area on pelvic floor muscle contraction, 10.59±1.71 in the HIFIT group and 9.72±2.11 in the control group . These findings are similar to this study. The dynamic assessment of the LAM was able to demonstrate that no participant presented LAM avulsion. Despite this, the javelin throw athlete had a markedly increased levator hiatus area during a voluntary Valsalva maneuver. This might be explained by a higher awareness by high-impact athletes regarding the kinesthetics involved in high impact exercises, which can enable them to use task-specific muscles, as well as more abdominal strength, and the resulting increase in intra-abdominal pressure they are able to develop (Kruger, Dietz et al. 2007). The volleyball athlete had the highest value of the levator hiatal area in MVC, so she contracted the PFM less. As explained above, high-impact exercises can cause PF disorders, namely weakening of the PFM, which in turn can lead to SUI (Carvalhais, Da Roza et al. 2018). This tends to be more prevalent in high-impact sports (Pires, Pires et al. 2020), such as gymnastics, track and field, and some ball games (Gram and Bø 2020).
SUI is mainly related to bladder neck hypermobility, PFM and pelvic ligaments which are weak or damaged (Lasak, Jean-Michel et al. 2018), as well as changes to the structure of the neuromuscular and connective tissues supporting the bladder neck and the urethra. If athletes continue to strengthen their PFM, urine leakage may never happen (Livingston 2016). It is extremely important to have PFM training in these athletes, as it is advised for the prevention and treatment of SUI in several studies (Hagovska, Švihra et al. 2017). In order to better accomplish the MVC, the participants received information about the structure / function of the PFM, in addition to learning to develop awareness of them. This means that the athletes received assistance in contracting the correct muscle during the MVC, without contracting the other related muscles, such as the rectus abdominis, the thigh adductor and the gluteus maximus (accessories). Doing so would mean a considerable decrease in the contractile activity of the PFM (Kruger, Dietz et al. 2007). SUI can interfere with athletes’s participation in sport and fitness activities, consequently affecting their health, self-esteem and well-being (Pires T 2020).
Two-dimensional (2D) ultrasonography has been one of the tools used to assess anatomical changes in the mobility of the pelvic organ of women suffering from SUI and POP (Dietz 2017). The findings showed that the PVU angle at rest does not show major changes. The findings during the Valsalva maneuver, demonstrated one participant (karate) had parameters compatible with urethral hypermobility. Although karate is considered a moderate impact sport, in fact the athlete mentioned that running, a high impact sport (Mitchell, Haskell et al. 2005), is also part of her daily training, which may justify these results. Women with SUI commonly (or high impact sports) show an increase in bladder neck mobility and a descent below the level of the symphysis pubis during the Valsalva maneuver. Dietz et al (Dietz, Eldridge et al. 2004) noted that the HIFIT nulliparous women group showed a considerably higher mobility of the bladder neck, as well as in the levator hiatal area than the control group. However, most of the HIFIT women were asymptomatic for UI, as observed in our study as well. The bladder neck descent measurements were the highest in the javelin throw (even though, within normal ranges). The remaining measurements were within the normal parameters (Dietz 2004). There is no definition of ‘normal’ for bladder neck descent, although a cut-off of 2.5 cm has been proposed to define hypermobility (Dietz 2004). Urethral mobility as a measure of urethral support, focuses mainly on the bladder neck (Dietz 2017). There is minimal information available on the mobility of the remainder of the urethra, which we believe is important to understand urethral support and the pathophysiology of SUI and urodynamic stress incontinence (Dietz 2019). According to Dietz et al (Dietz 2004), the retrovesical (or posterior urethrovesical) angle usually opens to up to 160-180◦, from a normal value of 90-120◦. Such a change in the retrovesical angle is often (but not always) associated with funneling. Three athletes (swimming, gymnastics and javelin throw) demonstrated a mild rectocele, but were asymptomatic for clinical symptoms of POP. The women with increased pelvic organ descent are usually associated to having ‘weak’ PFM. There is a known correlation between hypermobility syndrome and some connective tissue disorders, including an increased risk for POP (Pirpiris, Shek et al. 2010). These differences may be explained by the differences in the connective tissue itself or the muscle biomechanics, which may have originated before or after the high-impact training (Kruger, Dietz et al. 2007).
Conclusions
Although the sample is very small for large conclusions, there is a tendency for high-impact sports to suffer more changes in PFM, namely weak MVC that may lead to the appearance of SUI, as was the case with volleyball and javelin throw athletes.
Future research with a larger sample of high-performance athletes is necessary to explore whether they present similar results after the intervention.