Introduction
The increase in average life expectancy translates into an increase in the number of elderly people. In addition to a deep reflection on Portuguese and world social geography, this requires a reorganization of how health care and particularly nursing is provided, due to the particularities associated with this age group. As a result of aging, there is an increase in chronic diseases, including ocular pathologies. According to the National Program for the Health of the Elderly (Directorate General for Health (DGS, 2006), in Portugal, visual impairments are not valued in the context of chronic pathology.
Changes to vision, namely the formation of cataracts, which opacify the lens of the eye is common and very disabling. In most people aged 80 and over, cataracts are responsible for 50% of cases of total loss of vision, with 85% of cataracts being senile (considered a normal aging process), for which surgery is the only treatment option to recover visual capacity (Almança, Jardim & Duarte, 2018).
In treating cataracts, phacoemulsification is the most widely used surgical technique, due to the rapid visual recovery and reduced rate of intraoperative complications associated with it. It is a surgical procedure performed on an outpatient basis, which makes it possible to return home on the same day of surgery (or by midnight following surgery), and recovery from surgery may occur in a family environment.
Preparation for the patient’s homecoming is complex, due to the very constraints that an outpatient surgery imposes and the imperative need to promote the patient’s autonomy potential for surgical success. When changing from one health condition to another, the patient must assume the centrality of the care process (Mota, 2018). Since surgery, as a life event leads to change, it requires a differentiated intervention by nurses in facilitating the transitional course (Meleis, 2010). he preparation of the elderly person’s homecoming after cataract surgery is thereby essential, and nurses should assume their role as facilitators in this health/disease transition process. For this purpose, in the actual planning of care for the elderly, aging should not only be considered a biological phenomenon, but also a dynamic transactional process (Carvalho & Hennington, 2015).
It is important that nurses are able to understand the meaning of that experience for the patient, to assess their physical, emotional state and environmental conditions towards a healthy transition (Mota, Rodrigues & Pereira, 2011). Due to the high proximity of nurses to patients experiencing the transition process, they must be heedful to changes and demands, preparing and helping them to develop skills to deal with this situation. In order to promote self-management of health, nurses should assist patients in acquiring knowledge, skills and facilitate support (Mota, 2018). This has an impact on greater patient adherence and satisfaction, guaranteeing quality of care and impact in health gains affected by nursing care. In this context, this study intends to explore the information that nurses reveal in preparing the elderly person undergoing cataract surgery to return home. Identifying potentialities and difficulties should lead to implementing nursing therapies that meet the real needs of the elderly in their context of life.
1. Methods
Qualitative research study, data collection using the focus group technique.
1.1 Sample
Intentional sample consisting of six nurses from the same hospital unit in the central region of Portugal, with at least five years of professional experience in ophthalmic surgery (in accordance with point a) of paragraph 1 of Article 4 of Regulation No. 556/2017 of the Order of Nurses, which establishes that to recognise an increased area of competence, the nurse must have at least five years of proven professional practice).
1.2 Data collection instrument and technique
Informed of the objectives and methodological procedures of the study, six nurses were invited to participate by email. Initially, we expected to have a group of ten nurses, but four were prevented from participating for professional reasons. The focus group meeting lasted 75 minutes and was based on a scripted semi-structured discussion taking place in April 2019 in a classroom at the Northern Portuguese Red Cross Health School. The focus group was moderated by one of the researchers based on the research question and guided by discussion topics centred on self-care (hygiene, positioning, activities of daily living and management of the therapeutic regime). The focus group was recorded on audio and later transcribed in order to prepare the corpus for analysis.
1.3 Procedures
In order to guarantee anonymity, the name of the participants was replaced by a code consisting of a letter and a number (E1 to E6). After the text was transcribed, it was subjected to thematic categorical analysis according to Bardin (2015), with the categorization being carried out a posteriori, according to the categories resulting from the discussion, with categories, subcategories and sub-subcategories, to which the registration units were associated.
Participation in the study was voluntary with each participant signing an informed consent document. The study was approved by the Board of Directors and Ethics Committee of the Northern Portuguese Red Cross Health School under reference number 07/2019.
2. Results
The focus group consisted of six nurses from outpatient surgery, with an average time of professional practice in the area of ophthalmic surgery of 12.8 ± 4.9 years (maximum of 21 and minimum of 7 years). From the analysis of the results obtained, three categories emerged based on the nurses’ perspective on the elderly person’s homecoming after cataract surgery: “Facilitating/inhibiting factors,” “Management of the therapeutic regime” and “Promoting the potential for autonomy.” The categories emerged from a semantic aggregation, based on their relationship with the subcategories and the registration units. In the content analysis tables, only the registration units that best represent this unit are presented, so as to better understand them.
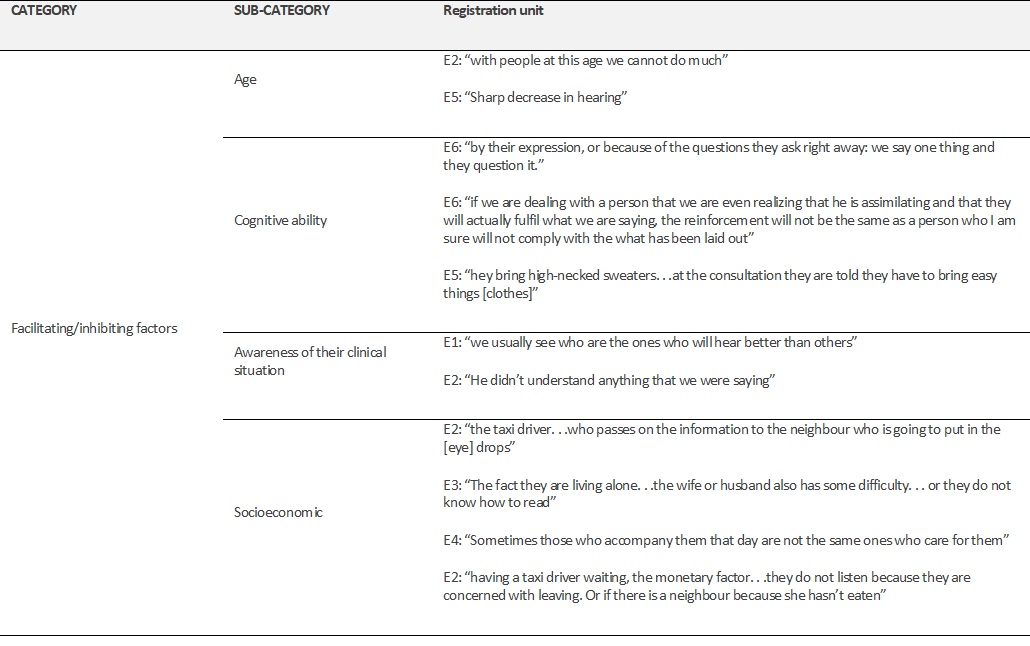
Facilitating/inhibiting factors
The “facilitating/inhibiting factors” in preparing for the homecoming that were identified by the nurses were: age, cognitive ability, awareness of their clinical situation and socioeconomic factors, as shown in Table 1.
Therapeutic regimen management
“Therapeutic regimen management” (Table 2) The “Management of the therapeutic regimen” (Table 2), contains the questions centred on the medication regimen and the prior preparation.
To manage the medication regimen well, nurses consider the information centred on the dose, schedule, and strategies relevant to manage the medication regimen, escalation therapy and their complexity.
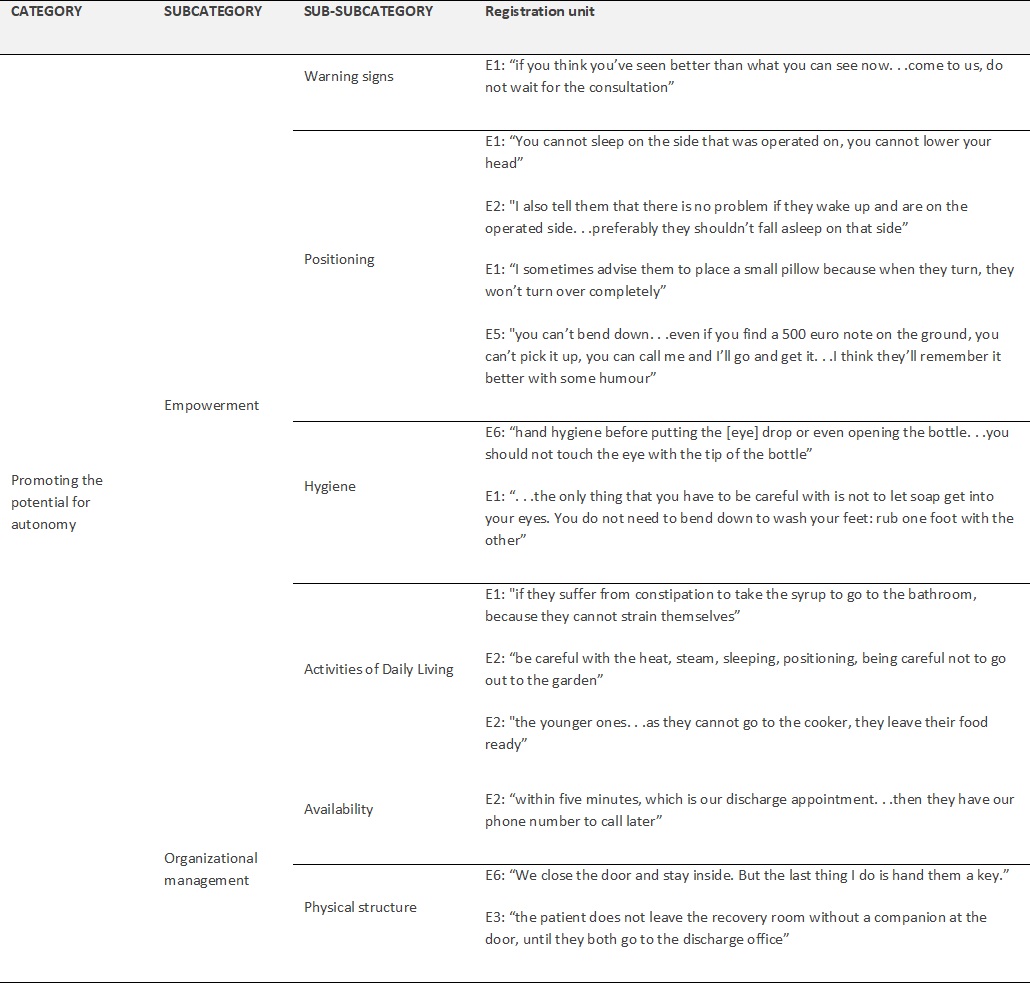
Promoting the potential for autonomy
“Promoting the potential for autonomy” as an emerging category in this study, includes factors related to empowerment and organizational management, as shown in Table 3.
With a view to promoting the potential for autonomy, nurses in empowering patients focus information on warning signs, positioning, hygiene and activities of daily living. Regarding organizational management, with a significant impact on nurses’ clinical practice, their availability to inform the patient and the physical structure of the outpatient surgery service emerges.
3. Discussion
In preparing for the homecoming of the elderly person who underwent cataract surgery, the nurses who participated in the study highlighted the fundamentals of the information centred on “Facilitating/inhibiting factors,” “Therapeutic regimen Management” and “Promoting the potential for autonomy.”
In the domain of “Facilitating/inhibiting factors,” nurses consider it relevant to take into account age, cognitive ability, awareness of their clinical situation and socioeconomic factors. For nurses to be truly significant in helping to experience healthy health/disease transition processes (Meleis, 2010), it is essential to recognize these factors in identifying real needs, but also the patients’ potential. Petronilho (2013) admits that the changes that occur in the aging process make people more vulnerable, increasing their exposure to risks, and nurses must identify their needs and develop strategies to facilitate the transition process. As a result of aging, it is essential that the assessment of the patient is multidimensional, including multiple comorbidities, (reduced) mobility, cognitive impairment, hearing, anxiety, literacy and family support, which can condition or hinder their recovery (Torrado, 2016).
As a result, the participants consider that the intervention in these patients is complex, stating that “with people at this age we cannot do much” (E2), and therefore, they recognize the need to identify an informal caregiver in order to guarantee surgical success. It is common for patients to show changes in their cognitive ability, which can affect their ability to circulate, as well as their memory, attention and evocation. As Nunes (2017) points out, factors related to aging itself can affect concentration and reasoning. Cognitive ability has a significant impact on the therapeutic regimen management (Moretti, Ruy & Saccomann, 2018). All of these factors can have significant repercussions on the person’s ability to take care of themselves, so it is essential to make the person aware of the changes that need to be made (Mota, 2018).
Moreover, the transition process is conditioned by socioeconomic factors, since the social and economic context is a factor with great impact on the way the person deals with the disease and recovery process, given that there are discrepancies when there are family support networks and/or other social agents or scarcity of support (Silva, 2016). Moreover, the transition process is conditioned by socioeconomic factors, since the social and economic context is a factor with great impact on the way the person deals with the disease and recovery process, given that there are discrepancies when there are family support networks and/or other social agents or scarcity of support (Silva, 2016). It is especially when the support system is compromised, that the nurse demonstrates their qualities and knowledge, acting as a resource, sometimes providing the elderly and the caregiver with means and strategies to deal with the health/disease process, and sometimes articulating with other members of the multidisciplinary team in order to jointly find the best solution.
Thus, care for the elderly in a surgical situation is a challenge, given that the changes resulting from the aging process and the presence of associated pathologies can compromise the functional balance and increase their vulnerability to the appearance of postoperative complications. However, when nurses are experts in the field of the aging process, the implementation of preventive measures has the potential to positively influence the patient’s surgical evolution (Silva, 2016). The overall assessment of the elderly person/family is essential for nurses to understand the person’s real needs, thereby making it possible to prepare them properly for the return home. The facilitating/inhibiting factors to the transition process may condition the way patients are able to manage his therapeutic regimen, as an activity they themselves perform and for their own benefit, to maintain their health and well-being (Oliveira, 2015).
For the patient undergoing cataract surgery, the medication regimen is a very relevant dimension in the area of therapeutic regimen management and is highly influenced by the patient’s prior preparation. It is important that nurses promote patients’ empowerment in order to promote their potential autonomy. It is therefore essential to create an atmosphere of involvement, answering questions and clarifying doubts, behaviours and attitudes, given that confidence in the health professional will be reflected in the way he adheres to the therapeutic regimen (Mota et al., 2011). The way in which the health/disease transition process is experienced influences the results. The dimensions that comprise the medication regimen are escalation therapy, the dose, the schedule, the complexity and the strategies used. With regard to escalation therapy, one of the concerns is related to the use of ophthalmic corticosteroids, prescribed to control the inflammatory process associated with cataract surgery (Branco, Bisneto & Moreira, 2017), due to their impact on the effectiveness of the treatment. The administration of eye drops every 2 hours increases the complexity of the medication regimen. This complexity is made even greater by the fact that the patients targeted by the care have impaired visual acuity, both in the eye submitted to surgery, and often in the other eye, as a result of aging itself. Oliveira (2015) mentions that the ineffectiveness in the management of the medication regimen is often associated with its complexity, lack of knowledge on how to integrate the therapeutic indications in daily life, the excessive demands on the person and the delay in or absence of positive results. In this sense, it is essential that the nurse recognizes the individuality of each person in order to implement appropriate nursing therapies for each individual.
Prior preparation was also identified in this study, as an important factor in preparing each of the elderly people to return home after cataract surgery, closely related to the preoperative consultation, in order to anticipate the needs of patients. For Silva (2016), the aim of the preoperative consultation is to decrease the levels of anxiety and includes aspects of physical preparation. The preoperative teaching to the elderly which must be adapted, given the speed of information processing is slower, which interferes with attention span, influences learning and can increase anxiety. When specific recommendations about preoperative care are provided, promoting the potential for autonomy to prepare for homecoming begins. Simultaneously, potentialities and possible difficulties of the patient family are evaluated, in order to outline strategies to facilitate self-care and favour this transition process.
With regard to “Promoting the potential for autonomy”, this includes factors related to empowerment and organizational management. Aging requires action at the level of changing behaviours and attitudes according to the “. . .social and family realities that accompany individual and demographic aging and an adjustment of the environment to the weaknesses that, more often, accompany old age.” (DGS, 2006, p.6). Regarding empowering patients to return home, Silva (2016) mentions that the great challenge facing nurses in the preoperative phase is to combine the principles and practice of surgical nursing with the unique characteristics of the elderly, as it requires capacity for perceptual assessment, careful identification of real and potential problems and meticulous planning of care tailored to their needs. In this context, nurses highlight warning signs, hygiene, activities of daily living and positioning as crucial information. Torrado (2016) warns of the fact that, although compliance with both movement restrictions and positioning is important, changing the person’s ability to retain the information transmitted may be the cause of surgical complications. In this adaptation process, the nurse must develop interventions that allow the elderly person to make the transition successfully. Valcarenghi, Lourenço, Siewert & Alvarez (2015) say that it is about empowering the elderly, so that they can take care of themselves.
The availability to promote the potential for autonomy and the physical structure of the facilities, led to the subcategory "Organizational management.” In view of patient-centred care provision, it is essential that the care time is the patient’s time, and the nurse must demonstrate availability in accordance with the patient’s care needs. Time management is one of the areas where organizations try to intervene ". . . seeking to adapt the procedures to the individual and collective performance of professionals, in order to influence their levels of productivity. . .” (Ribeiro, Vieira, Cunha, Dias & Martins, 2016, p. 8). However, when providing health care, it is necessary to balance the patient’s time with the time that health organizations allow nurses to have to perform their duties. For Ribeiro and collaborators (2016) for an adequate performance of functions, professionals should be provided with the necessary resources and means taking into account their purpose. The physical structure of health organizations influences the entire process of promoting the patient’s autonomy potential in preparation for their return home. In his study, Dias (2014), attentive to the adequacy of the physical space while preparing for the return home, mentioned that nurses consider it important that this space provides privacy and comfort both to the person undergoing surgery and to their family. The physical structure has thus proved to be important for nurses, since in order to promote the potential for autonomy not only is privacy essential, but the transmission of information must also be carried out with tranquillity, allowing doubts and concerns that can hinder the transition to be clarified and compromise surgical success.
Conclusion
Aging with health, autonomy and independence, represents a huge challenge and responsibility for society, through the definition of interventions that meet the real needs of the elderly in their life context. On the other hand, health policies emphasize the responsibility, involvement and empowerment of the person in order to facilitate the transition processes throughout the life cycle. In this context, it is up to nurses to collaborate, communicate effectively and prepare the elderly for care to be sustained on returning home. After conducting the study, we can say that nurses consider facilitating/inhibiting factors (age, cognitive ability, awareness of the clinical and socioeconomic situation), therapeutic regimen management (medication regimen and prior preparation) and promoting the potential for autonomy (empowerment and organizational management), relevant in preparation for the homecoming of the elderly person who has undergone cataract surgery, whose treatment for the recovery of visual capacity is carried out mostly under outpatient surgery, using the phacoemulsification technique.
The recognition of the information that nurses emphasize in preparing the elderly person for homecoming having undergone cataract surgery is essential for their therapeutic intervention, since it allows the clinical areas to be considered in favour of providing care that meets the real needs of the elderly, favouring a healthy transition taking into account their contexts, resources and life projects. It is thus possible to define clinical guidelines with a view to better decision making, in order to guarantee quality and continuity of care.
As for limitations of this study, we highlight the low number of nurses who agreed to participate in the focus group, as such, the discussion group was smaller than initially planned.
Future studies in this area are suggested, so as to continuously provide more adequate answers to the needs of the elderly, in an increasingly aging society.
In terms of implications for practice, this study denotes the need for nursing care to be carried out in partnership and in close proximity to the elderly and their caregivers.