Introduction
This case report refers to a 26-year-old female of the Caucasian race, married, with 12th grade, employed as an educational action technician, obstetric index 0010, gestational age of 41 weeks, with Oligohydramnios. Her religion is Jehovah's Witness, without a living will or statement signed by the pastor. She was admitted for induction of labor. The delivery occurred on the same day, and was a dystocia delivery by suction cup, with the extraction of a newborn male with 3750 kg and an Apgar score of 9/10.
Pregnancy is considered a natural physiological event that occurs without intercurrences, however, in 20% of the cases, unfavorable evolution is probable for both the fetus and the mother, thus configuring a high-risk pregnancy, defined by a wide range of clinical, obstetric, and/or social conditions that may lead to complications in pregnancy. These risks are mainly related to pre-existing diseases or pregnancy complications due to organic, biological, chemical, and occupational causes, as well as unfavorable social and demographic conditions (Brilhante & Jorge, 2020).
During vaginal delivery, there are several associated risks, namely the occurrence of postpartum hemorrhage (PPH). Hemorrhage in obstetrics is the leading cause of maternal morbidity and mortality, affecting about 2% of women in labor and 5-10% of deliveries, and concomitantly responsible for a quarter of maternal mortality. It is characterized by a loss of more than 500 ml after vaginal delivery and 1000 ml after a cesarean section, and, according to the American College of Obstetricians and Gynecologists, HPP was defined as blood losses equal to or exceeding 1000 ml or even hematic losses accompanied by signs and symptoms of hypovolaemia in the first 24 hours after delivery (Carvalhas et al., 2018). It can be triggered by prolonged labor, uterine atony (70% of cases), episiotomy, macrosomia, the use of forceps and suction cups, induction of labor, placental remnants, previous postpartum hemorrhage, and nulliparity. As prophylaxis, some studies point out that oxytocin has a more effective indication for prophylactic use than misoprostol, however, prostaglandins should be administered, uterine massage should be started after the identification of bleeding, and when it does not reverse, intravenous hydration should be administered and blood transfusion should be performed (Santos, 2020; Vieira et al, 2018). However, autologous transfusion is also increasingly used, and this treatment has shown safety and an increase in obstetric care, concerning few complications. This should be considered whenever the loss of a blood volume that implies the need for transfusion is anticipated, such as in pregnant women at increased risk of bleeding or in parturient where transfusion is not an option due to refusal (Vieira et al, 2018).
Religion plays a fundamental role in the cultural life of different groups and places which is integrated into complex forms into the beliefs, actions, and experiences of the faithful. Religion is understood as a vast system of principles, norms, and values, associated with sacred and spiritual elements, which determine the choices and behavior of human beings, structures, alongside other factors, and the cultural identity of social groups. According to Franca (2016, p.22) "the importance of religion, in structuring the identity of each one, is evident in three dimensions: an intellectual-emotional dimension, where beliefs, doctrines, reflection are included; a ritual-celebrating dimension; a praxis dimension, with the moral, charitable aspects, of the fight for justice; a community dimension, since the previous dimensions are lived communally and establish community ties". The faithful, by integrating religious beliefs and practices into their daily life, project their religious identity in the space and the social relations they establish with the community where they are inserted (Franca, 2016).
As a religion, we find their rights and duties in Law no. 16/2001, of 22 June, as well as the rights and duties of their faithful, it should be noted that Article 2, addresses the equality between all religions before the Portuguese State, which attests not only the principle of separation between the State and the churches, as well as reveals the importance that the religious phenomenon has for the legislator and Portuguese society (Pratas, 2016).
This case was chosen to consider the religion of the person under study, a Jehovah's Witness practitioner. According to the 2020 World Report of Jehovah's Witnesses, in Portugal, there are about 51,991 practitioners, available on the official website of Jehovah's Witnesses (https://www.jw.org/pt-pt/biblioteca/livros/relatorio-do-ano-de-servico-2020/). Jehovah's Witness parturients constitute a unique obstetric population because, according to their religious beliefs, they refuse total blood transfusions and its four main components, as this is forbidden by the bible since blood is considered the soul. This refusal is based on the biblical command to "abstain from blood", but this orientation often raises ethical conflicts between health professionals and the patient, in the official website of Jehovah's Witnesses (https://www.jw.org/pt-pt/pesquisar/?q=transfus%C3%B5es+de+sangue) we could consult several texts where this issue is explained. Health professionals must know how to approach these people, which options they accept if they need this type of treatment, and plan nursing care according to their beliefs.
However, during childbirth, bleeding can be unexpected, and thus, women who refuse blood transfusions have over time generated conflict situations involving doctors, users, and family members. When treating pregnant women who refuse blood transfusions and blood products, the situation becomes even more delicate due to the risk for the pregnancy itself related to bleeding but forcing someone to perform a medical treatment without their prior consent is an unethical practice because a person cannot be deprived of the right to freedom and self-determination because of religious beliefs (Bezerra, Cesar & Lara, 2015).
Ethical, moral, and legal changes associated with the technical-scientific evolution in recent years have led to new health practices, more focused on respect for autonomy, in the same way, that haemocomponents and blood derivatives play an important role within blood-based treatments. The blood treatments that can assist in this and other physiological processes can be mentioned as whole blood (transfusion), haemocomponents (plasma, RBCs, platelets, platelet-rich plasma, and platelet gel), haemoderivatives (fibrin glue, serums, vaccines, plasma expanders, and coagulation factors), also the transfusion of fresh autologous whole blood (Pre-operative collection and storage of autologous blood for later reinfusion), is refused according to the religious and ethical position on medical treatments and related issues (https://www. jw.org/en/medical-library/strategies-discharge/religious-and-ethical-stance-on-medical-treatments-and-related-issues/). Among these, the most accepted are the haemoderivatives, although there are Jehovah's witnesses who consider them as blood, that is, as soul. Hemocomponents are then the least accepted because they have more blood constituents (Azambuja & Garrafa, 2010).
From an ethical point of view, if a patient is fully informed about the risks/benefits of not receiving a blood transfusion or blood components, and persists in refusing, this decision should be respected. The respect for this autonomy is one of the fundamental principles on which biomedical ethics is based, and the autonomy principle takes into account the freedom and responsibility of the user, in deciding what is good for her, even if the choice is not shared by the physician. However, to preserve the right to autonomy in their decisions, these users must use a document registered and signed by their pastor and two other witnesses and also have an updated living will, because, if the parturient/puerperal woman presents a hemorrhage and loses consciousness and has a living will where it states the alternatives to the defined health care or a responsible person to make decisions regarding her treatment, her will should be exercised (Bezerra, Cesar, & Lara, 2015).
Law No. 25/2012 then safeguards the right to a bloodless treatment, through the possibility of previously making their wishes known in conscience through a written document, which regulates advance directives of will, namely in the form of a living will, the appointment of a health care proxy and creates the National Registry of Living Wills. However, this wish does not always end up being fulfilled, because, in an emergency, the doctor may act without respecting the choice of treatment, to save the patient's life (Pratas, 2016).
In the course of a hospitalization, sometimes there are conscientious objector physicians, and despite not having the force of law, the Code of Medical Ethics establishes, that the doctor is not obliged to provide services that contradict his beliefs. And as Jehovah's Witnesses supporters do not accept transfusions of whole blood or its primary components because it contradicts the biblical principles they defend, this refusal becomes a sensitive issue when impacting the commitment of doctors (due to the Hippocratic Oath) to defend the health and welfare of their users. Therefore, ethical conflicts are sometimes generated, because if the patient expresses his/her will and refuses some medical treatment, such as blood transfusion, and their living will is updated, the patient's autonomy of will must be respected and the doctor must obey the patient's will, but, on the other hand, if the doctor obeys the patient's will in cases of life-threatening situations, he/she will be going against his/her oath to save lives (Junior, Mendes, & Baretta, 2020).
This case report aims to develop a proposal for a care plan with emphasis on the interventions performed according to the religious beliefs and decisions of a pregnant patient.
1. Methods
The present case study is defined as a structured research method, that was applied to explore, describe, and explain the situation more deeply, based on evidence, allowing for a better understanding of certain life phenomena (Andrade et al., 2017). This case study follows the CAse REport (CARE) guidelines (Riley et al., 2017), and the flowchart was used to expose the case according to the Equator Network (2019) model.
Data collection was conducted through the interview, observation, and physical examination, of the user. To this end, it was necessary to explain to and clarify to the user about the case study and its purpose, clarifying her rights, and ensuring anonymity and confidentiality of all data obtained. Thus, we respected verbal informed consent and the ethical principles of nursing research about beneficence, non-maleficence, fidelity, justice, veracity, and confidentiality (Nunes, 2020). Verbal consent was obtained from the patient, but due to the current pandemic context, it was not possible to obtain written consent. However, to publish the study, data were substantiated, anonymity was respected, complying with the principles established in the Helsinki Declaration for studies involving human subjects (2013), and we followed the recommendations of the Oviedo Convention (Portugal, 2001) to ensure human dignity.
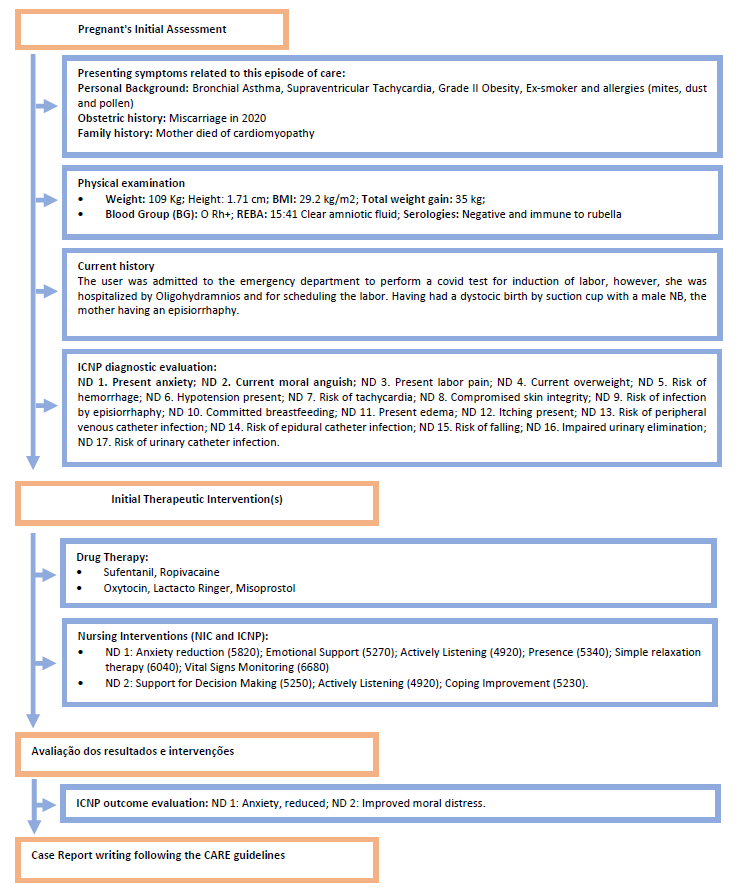
This case study was developed according to the Nursing Model Based on Activities of Daily Living - Roper, Logan & Tierney (2001) since its main assumption is that quality of life is assessed by dividing this assessment into the individual's activities of daily living. This is centered on the person, who is defined as an open system in permanent interaction with the environment, comprising twelve daily life activities which are influenced by biological, psychological, socio-cultural, environmental, and political-economic factors, i.e., these activities are conditioned by the stages of life. The individual may have times when he/she can or cannot carry out a certain activity independently. Throughout the life cycle until adulthood, individuals go through events that can affect the way they perform the activities of daily living (ADLs), becoming less or more independent in them (Fonseca, Coroado, & Pissarro, 2017).
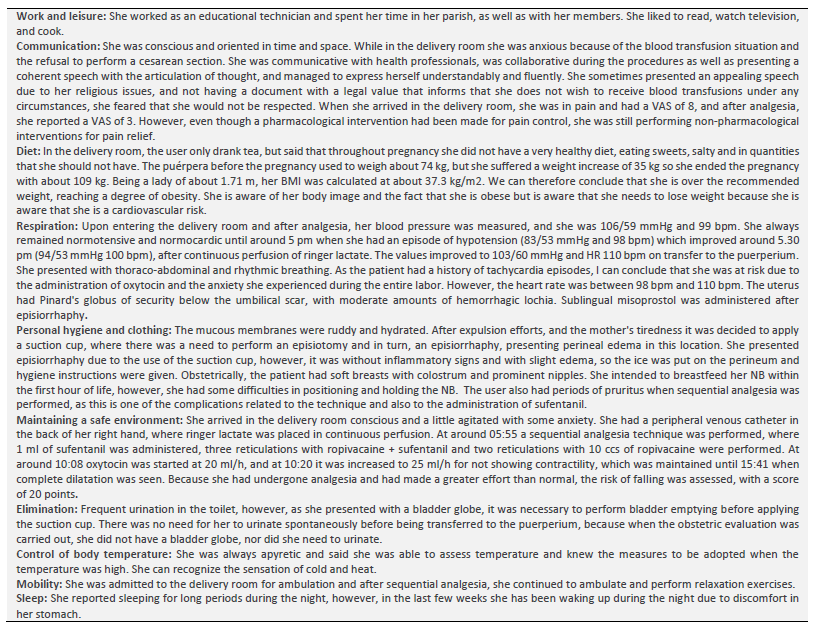
The initial assessment of the patient was based on the Activities of Daily Living Model and, after collecting data on the person and her context, a nursing care plan was developed. Next, we present the user's assessment according to the selected theoretical model (Table 1).
Nursing diagnoses (ND) were selected according to the Taxonomy of the International Classification for Nursing Practice [ICNP] (Ordem dos Enfermeiros [OE], 2016); nursing interventions were justified by the Nursing Intervention Classification [NIC] (Butcher, Bulechek, Dochterman & Wagner, 2018), outcomes were supported and assessed according to the ICNP taxonomy. The flowchart (figure 1) according to CARE guidelines (Equator Network, 2019) was elaborated for a better understanding of the case. The assessment data presented report only to the time of collection, without reference to individual habits before hospitalization.
2. Results
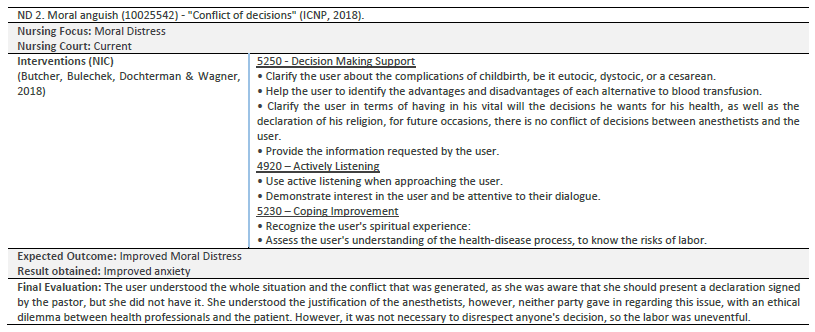
Taking into account the data presented above and after having reached the 12 Nursing diagnoses, we will only address two ND in this article: 1. Present anxiety and 2. For current moral distress, it was necessary to determine the interventions that could be planned and applied to decrease this risk. Tables 2 and 3 show the care plan developed for each ND.
3. Discussion
Labour is one of the most important moments for women, causing a constant change, i.e., it transforms the woman into a mother, physically and emotionally. Childbirth is much more than a physical event and what happens during it can have a decisive influence on the relationship between mother, child, and the remaining family, as well as the woman's reproductive future (Ferreira, 2017). However, it can cause a woman's risk of bleeding, the more pathologies the woman has associated, the longer the duration of labor and its assistance, such as prolonged third stage of labor, macrosomia, uterine atony, induction of labor, episiotomy, nulliparity, the use of forceps and suction cups, and difficulties in the descent of the fetal presentation (Vieira et al., 2018).
To ensure the decision of this patient, we had to consider her background, and since she had grade 2 obesity, bronchial asthma, and tachycardia, we had to analyze the risks of these to prevent a possible hemorrhage, as well as the possible risks of labor. Because the consequence of obesity in childbirth, regardless of the route of delivery, is more often the increased occurrence of endometritis, infection of the surgical wound, episiotomy lacerations, and postpartum hemorrhage. In addition, obesity makes pregnancy a high-risk pregnancy due to maternal and neonatal complications associated with cardiovascular diseases, gestational hypertension, diabetes mellitus, venous thromboembolism, increased incidence of cesarean sections, fetal macrosomia, shoulder dystocia, low birth weight, and neonatal hypoglycemia, among others (Paiva, Nomura, Dias, & Zugaib, 2012; Nogueira & Carreiro, 2013). As well as dystocia by suction cup delivery can sometimes lead to injuries in the perineum, and, in turn, increase the risk of postpartum hemorrhage. Sometimes the injury to the perineum is one of the most common traumas during childbirth, i.e., lacerations of the external genital organs, which, in turn, may increase hemorrhagic losses (Ferreira, 2017).
Being a Jehovah's Witness and refusing a blood transfusion, we had to try to explain the risks that could reverse labor and the possible forms of treatment, but she maintained her opinion and preferred us to administer the preventive forms (oxytocin, prostaglandins) and if she needed another treatment, she would consider another option. The possible treatments for postpartum hemorrhage depend on the severity of the hemorrhage and may require a blood transfusion. However, preventive measures are always taken, such as palpation of Pinard's globe of safety, uterine expression, surveillance of lochia loss, monitoring of vital signs, administration of intravenous oxytocin, administration of isotonic crystalloids to restore hydro-electrolyte balance (e.g. Ringer's lactate) (Vieira et al, 2018). However, considering the patient's religion and the need for health professionals to be constantly updated on new forms of treatment, we should consider other options accepted by the patient, such as autologous and blood product transfusion (Azambuja & Garrafa, 2010).
Based on the pathologies, risks of labor, and religion, and as shown in Tables 2 and 3, the diagnoses of Anxiety and Moral Distress were identified, and it was possible to conclude that, with the nursing interventions performed on both main diagnoses, there was an improvement in anxiety and, in turn, an improvement in moral distress, since no bleeding occurred, even though an episiorrhaphy and a suction cup delivery were performed (Freixo, 2015).
The importance of controlling anxiety is essential because it represents a risk to fetal growth and behavior and because of lower fetal weight (Pinto, Caldas, Silva, & Figueiredo, 2016). Pregnancy anxiety is sometimes triggered by a set of concerns related to childbirth and the newborn's health, and, in this case, it was because the user's decisions and beliefs were not respected. Therefore, nurses should pay attention to the user's beliefs and identify possible psychological changes during childbirth and postpartum, to perform preventive interventions and provide a proper reception to each parturient woman, improving the woman's level of knowledge and, in turn, providing less anxiety (Araújo et al., 2020). In other words, in this case, it was essential to accompany the pregnant woman and remove all her doubts regarding labor and its possible risks and provide her with the necessary knowledge regarding her decision on the treatment to be performed in a possible postpartum hemorrhage.
The nurse is then essential in the implementation of interventions and the understanding and interaction of the health disease process, to implement the interventions and subsequently assess them, considering the individualization of care. For, the role of nursing in childbirth should start early, helping and assisting women who wish to experience motherhood and trying to reduce its risks of it. The health professional who will establish a bond with the parturient woman will provide her with more security and confidence for her doubts and decisions aiming at the woman and fetus' health welfare.
However, the refusal of blood and blood component transfusion by parturients and puerperal has generated many legal, ethical, and bioethical conflicts, so when the life of a patient is at risk and she refuses blood transfusion, the doctor experiences a situation of difficult resolution, since she must choose between respecting the patient's autonomy or the legal codes governing her practice (Bezerra, Cesar, & Lara, 2015).
Conclusion
About the relevant issue in this study, since this patient had no document proving her religion, the relationship between health care professionals and the patient was a little more complicated, because, on the one hand, they wanted to respect her decision, but, on the other hand, if there was any risk to her life, health care professionals would not be able to respect her. This meant that care was more directed to the patient's anxiety, trying to explain the situation and, on the other hand, giving hope to the patient to reduce anxiety.
The ethical dilemma was caused by the fact that the team of obstetricians and anesthetists were conscientious objectors and the fact that the patient did not have a legal document stating that she did not want to undergo the procedure.
with legal value stating that they do not wish to receive blood transfusions under any circumstances. The document is drawn up by local laws and informs what the bearer's personal decision is regarding blood fractions, procedures involving the use of her blood, and other matters of a medical nature. The medical team tried to explain the situation to the user so that she would be aware of the problem that this issue was raised, however, the user kept her decision and at the end of delivery there were no complications and no need for treatment with blood transfusion.
This situation has led us to reflect on how important it is to have all our health decisions recorded in the living will so that the will is respected, even in the case of risk to life. But on the other hand, it is health professionals who make decisions that go against their ethical code.
The development of this case report allowed reflection on the importance of religion in the healthcare provided to patients, namely the importance of nursing care in these situations.
The possible limitations of this Case Study refer to the articles used since only the articles available online and free of charge were used, and the most recent ones possible, which may have led to the non-inclusion of some studies related to the topic, available in databases to which I had no access.