Introduction
Respiratory rehabilitation (RR) is a key treatment strategy in respiratory pathology (Rocha, Pestana, Correia, Gomes, & Gouveia, 2018). The General Directorate of Health (GDH [2009]) defines it as a global and multidisciplinary intervention aimed at patients with chronic respiratory disease who are symptomatic and often have reduced activities of daily living. It is designed to reduce symptoms, optimise functionality, increase social participation and reduce healthcare costs, through the stabilisation or regression of the systemic manifestations of the disease. RR has several benefits, such as decreased dyspnea and fatigue, increased tolerance to exertion, reduced hospital admissions, improved quality of life, and promotion of healthy behaviours (Gronkievwicz & Coover, 2011). It is considered an effective therapeutic approach, whose success will depend on the experience and skills of the multidisciplinary team, the adherence of the person, in this case the paediatric patient and family, and the economic and social conditions (GDH, 2009; Postolache & Cojocaru, 2013). Respiratory problems may have significant repercussions on the person's autonomy and quality of life (Gronkievwicz & Coover, 2011). RR integrates several components, namely respiratory functional re-education (RFB), inhalation therapy optimization, and exercise training (Cordeiro & Menoita, 2014; Rocha et al, 2018), playing a key role in reducing hospital admissions and improving the quality of life of people with respiratory pathologies.
When applied in paediatric age, RR is beneficial in situations of respiratory compromise, complications of neurological or cardiovascular diseases and postoperative care (Cordeiro & Menoita, 2014).
In the context of the SARS-COV-2 pandemic, health services needed to reorganise the care provided, prioritising the fight against the spread of the disease. In São Miguel, in the Azores, the Hospital do Divino Espírito Santo de Ponta Delgada, EPER (HDES) closed the respiratory kinesiotherapy (CR) service, leading to people with respiratory problems and in need of respiratory rehabilitation being deprived of this care.
With the increase in acute illnesses and the consequent increase in paediatric hospital admissions, the articulation and complementarity between hospital and primary health care became essential for the admission of users in this age group to primary health care. This articulation ensured the continuity of respiratory kinesiotherapy, preventing complications due to its deprivation, namely more frequent antibiotic therapy and increased frequency of hospitalisations.
Regarding the effects of respiratory rehabilitation, research has supported the benefits of its implementation. The study carried out by Lopes, Delgado & Ferreira (2004) with children with asthma and their parents demonstrated the importance of the guidance given by nurses specialised in rehabilitation, showing that the information provided by these professionals on asthma triggering factors resulted in better adherence to therapy. It also had an effect on the reduction of emergency room visits. They also found that, of the children with poor adherence to treatment, around 84% had to go to the emergency room or had their crises treated at home, while in the group of children with good adherence to treatment, the percentage of these complications was 65%. The study also revealed that 26% of children did not perform the inhalation technique correctly (Lopes, Delgado & Ferreira, 2004).
Postiaux, Dubois, Marchand, Demay, Jacquy & Mangiaracina (2006) conducted a longitudinal prospective study with 19 children diagnosed with acute viral bronchiolitis and assessed different parameters before and after respiratory functional re-education sessions, with a total of 57 sessions. Prolonged slow expiration and provoked cough were performed as respiratory rehabilitation techniques, with evaluation of their efficacy. The authors concluded that there was a significant improvement of the clinical parameters, more specifically in the values of heart rate which reduced from 149 bpm to 134 bpm and of SpO2 which improved from 96% to 98%. These authors refer to this protocol as safe and capable of reducing the symptoms of bronchial obstruction in moderate acute viral bronchiolitis (Postiaux, Dubois, Marchand, Demay, Jacquy & Mangiaracina, 2006).
More recently, Postiaux, Louis, Labasse, Gerrold, Kotik & Lemuhot (2011) in a randomised study concluded that effective functional rehabilitation in children with acute respiratory bronchiolitis consists of 15 prolonged slow expirations and 5 provoked cough manoeuvres. The study included 20 children, with a mean age of 4.2 months, divided into two groups: one group with 8 children who received 27 sessions of hypertonic nebulisation and the other composed of 12 who received 31 sessions of hypertonic solution nebulisation and the new respiratory functional rehabilitation protocol. The Wang clinical severity score, SpO2 values and heart rate were used for evaluation before each session and 30 to 120 minutes after. There were improvements in the different percentage values for the group that underwent respiratory functional rehabilitation and with better values after 120 minutes. The mean hospital stay was not significantly different between the groups (Postiaux, Louis, Labasse, Gerrold, Kotik, & Lemuhot, 2011).
Also in 2011, the Portuguese Nursing Association in a study with asthmatic children who underwent conventional breathing exercises and playful breathing exercises highlights the change in lung mechanics and the reduction of physical activity limitation.
In cystic fibrosis, in which mucus obstruction leads to a pronounced inflammatory response, damaging the airways, leading to bronchiectasis and respiratory failure, the process is characterised by episodic exacerbations with infection and progressive decline in lung function. Secondarily, bronchiolitis and purulent plugs occur in the airways. Thus, the rehabilitation of respiratory function involves the elimination of secretions, contributing to reduce the number of respiratory infections and also reducing the risk of lung injury, since the drainage of secretions is essential to ensure the preservation and improvement of lung function and allow for the effectiveness of inhaled antibiotics (GDH, 2015).
Respiratory functional re-education is considered to be an important component in the maintenance care and treatment of patients with respiratory pathology. Therefore, a respiratory functional re-education project should be effectively individualized, taking into account several aspects: "the pathology, the degree of severity of the problem, the patient's age, learning ability, project goals, existing resources, and the person's motivation processes, among others" (Cordeiro & Menoita, 2014).
When developing a respiratory rehabilitation plan for children with respiratory pathologies, crisis prevention should play an important role. The rehabilitation nurse should teach the parents/caregiver about the triggering factors of a crisis, transmit information about the factors that can be controlled, and assess the correct therapeutic administration. It is also crucial in these projects to involve parents/carers in defining the project, so that therapeutic adherence, which is important to ensure the effectiveness of the rehabilitation treatment, can be ensured (Parentes, 2014). As such, it is of great importance to promote family health literacy in order to transform the reality at home beyond the hospital setting (Prato, Silveira, Neves, Bulbot, 2014).
It is at home, despite the scarcer resources, that the specialist nurse in rehabilitation nursing has the opportunity to care for the person/caregiver/family with a higher degree of adequacy to reality (Silva, 2016). In fact, the home environment is hardly reproduced in an inpatient or outpatient setting (Silva, 2016).
In this context, the use of telehealth seems to be an interesting solution in the context of the SARS-COV-2 pandemic. The term telehealth describes the provision of health care at a distance using information and communication technology (ICT) sources and allows the inclusion and participation of a multidisciplinary team (WHO, 2020).
The SARS-COV-2 pandemic has prompted health services to rapidly expand telehealth which should not be considered a temporary solution but a sustainable alternative for safe healthcare delivery (WHO, 2020).
Thus, this article aims to disseminate the effectiveness of a respiratory rehabilitation (RR) project, using telerehabilitation, in reducing the prevalence rate of nursing diagnoses in a sample of paediatric individuals with respiratory pathology, thus contributing to their well-being in the context of a pandemic.
1. Methods
The project Paediatric Respiratory Rehabilitation in a Pandemic Context - Respiratory Telekinesiotherapy & Home Visitation aimed to ensure continuity of care with regard to respiratory rehabilitation in the paediatric population that was deprived of this care with the closure of the Respiratory Therapy Service of the HDES, as a consequence of the pandemic. The target population was paediatric individuals with respiratory pathology. The sample used in the study was not probabilistic by convenience, consisting of all children and adolescents referred by the external consultation of paediatrics of the HDES.
This was a quantitative, analytical and longitudinal research design.
A non-experimental, pre-test, post-test study design was chosen.
Thus, in coordination and complementarity between the Hospital and the Health Unit, a RR project was designed by the Rehabilitation Nursing Team of the Unidade de Saúde da Ilha de São Miguel (USISM).
The project was implemented with the participation of four Specialist Nurses in Rehabilitation Nursing (RNR) who work in the multidisciplinary team of the USISM in home respiratory rehabilitation.
An intervention was designed with the purpose of optimizing the respiratory function of pediatric patients with sequelae and complications related to their clinical cardiorespiratory status, using telerespiratory rehabilitation. More specifically, it was proposed to improve by 90% the nursing diagnoses: impaired ventilation, ineffective airway clearance, activity intolerance and lack of knowledge about the inhalation technique. We proposed to train 80% of users/parents to follow the orientations given within the RR project and to reduce by 40% the incidence rate of hospital admissions due to acute respiratory pathology.
The project Paediatric Respiratory Rehabilitation in the Context of a Pandemic - Respiratory Therapy Telekinesitherapy & Home Visitation, on the one hand, ensured continuity of care regarding respiratory rehabilitation in the paediatric population that was deprived of this care with the closure of the Respiratory Therapy Service of the HDES as a consequence of the pandemic, but, on the other hand, it allowed the effectiveness of such a programme at home to be tested.
Thus, before the beginning of the programme, a first contact was established with the participants, with a view to explaining what was going to be done, requesting consent, as well as completing a questionnaire for socio-demographic characterisation and assessing the participants' health condition and respiratory function, completing and raising the appropriate nursing diagnoses. Afterwards, the intervention was applied, focusing on Respiratory Telekinesiotherapy (RCT), which is an innovative, safe and effective working method that consists in performing breathing exercises in consultation, by video call. This measure was aimed at the population whose respiratory pathology was stable and who mastered the breathing exercises but who could not suspend the Respiratory Rehabilitation (RR) as it was harmful to their health condition. In these sessions, the sessions of RR begun in the HDES were continued, with a periodic evaluation of the need to readjust the therapeutic plan. Exercises were implemented to improve muscle function and strength and consequently reduce dyspnea, training of the respiratory muscles to promote increased tolerance to effort, improved quality of life and dyspnea. They were also used to teach aspects related to breath control, bronchial hygiene, therapeutic regime, nutrition, physical activity, activities of daily living, among others. They were also ideal moments for early detection of exacerbations of the pathology.
Another intervention was the home visitation (HV), restricted exclusively to those at high risk of respiratory pathology exacerbation and consequent hospital admission, often detected during RCT sessions. At the HV, an evaluation of the child's health condition was made, corrective measures of the therapeutic regime were implemented and, if deemed necessary, the child was referred to the HDES external consultation service for assessment by the paediatrician.
For individuals who did not reside on the island of São Miguel, and with the awareness that access to these individuals was more difficult, it was defined that, at the time of referral by the paediatrician, an assessment was made of the child still on the island of São Miguel. After the child had returned to the island, the RCT sessions would start. If changes in the breathing pattern were observed, the paediatrician would be notified and these patients would be sent to the island of São Miguel for a more adequate evaluation. At this time, the team would carry out a DV at the place where they were staying.
The development of the rehabilitation programme was carried out in the following stages: preparation of the programme; training of the nurses involved; contact with the paediatrician responsible for the assessment of the children to establish referral channels; implementation of the project.
Data were analysed according to their nature, namely descriptive and inferential statistics using the Statistical Package for Social Sciences (SPSS) version 25.
For the participation in this study, the participants' parents were asked to give their informed consent, and the ethical precepts to be followed in this type of research were respected, according to the standardised in the Declaration of Helsinki (1964), which translates the international recommendations on clinical research. Authorisation for this study was also requested to the Board of Directors of the USISM.
2. Results
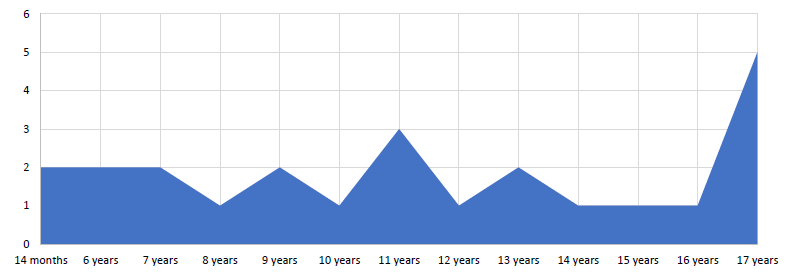
The convenience sample consisted of 24 individuals of both sexes, aged between 14 months and 17 years, with the distribution shown in chart 1. The mean age was 11 years, with a standard deviation of 1.10.
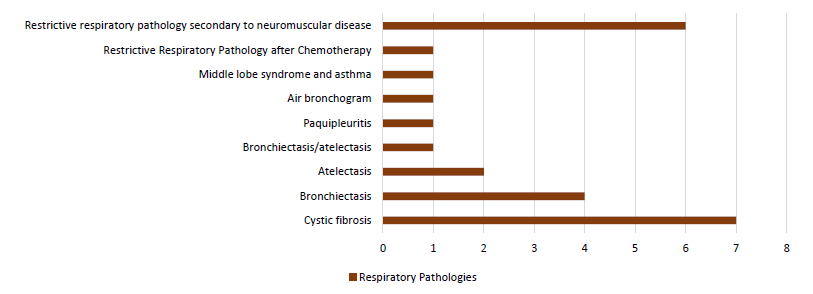
With regard to the pathologies that were at the origin of referral, they were cystic fibrosis (7); restrictive respiratory pathology secondary to neuromuscular disease (6); bronchiectasis (4); atelectasis (2); bronchiectasis/atelectasis (1); pachypleuritis (1); air bronchogram (1); middle lobe syndrome and asthma (1) and restrictive respiratory pathology after chemotherapy (1) (chart 2).
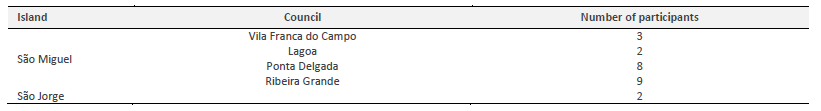
In what concerns the place of residence, 91.6% live on the island of S. Miguel, while 8.4% live on the island of S. Jorge. With regard to the distribution by municipality of residence on the island of São Miguel, 9 lived in the municipality of Ribeira Grande, 8 in Ponta Delgada, 3 in Vila Franca do Campo and 2 in Lagoa (Table 1).
With regard to their ability to perform their usual activities, after the application of the Functional Disability Scale (version for children and adolescents), 20.8% of the participants presented, at the lowest level, a lot of difficulty and the remaining presented, at the highest level, some difficulty (79.2%).
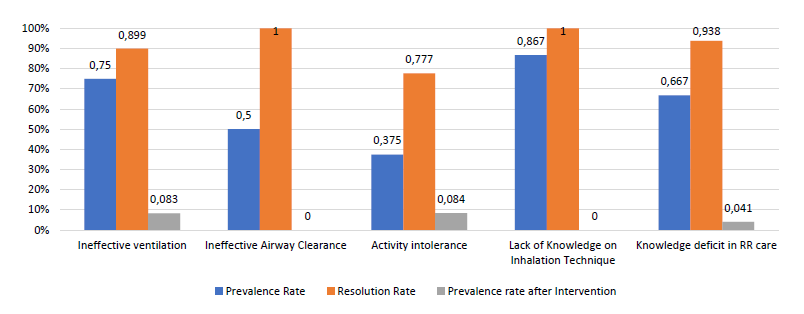
When admitted, the children presented as nursing diagnoses impaired ventilation (75%), ineffective airway clearance (50%) and activity intolerance (37.5%). They also presented knowledge deficit on the inhalation technique (86.7%) and knowledge deficit on RR care (66.7%) (chart 3).
After the implementation of the project that included the VD and RCT, by the REs, we found that the prevalence rate of Nursing diagnoses of the admitted population reduced considerably. As regards the diagnosis of impaired ventilation, the resolution rate was 88.9%. The diagnoses of ineffective airway cleaning and incorrect inhalation technique recorded a 100% resolution rate. As regards the diagnoses of activity intolerance and lack of knowledge on the care to be provided within the RR project, the resolution rate decreased by 77.7% and 93.8%, respectively (chart 3).
Thus, when the prevalence rate of nursing diagnoses was reassessed in November 2021, the prevalence rate decreased dramatically (chart 3). With regard to the nursing diagnoses of ineffective ventilation, activity intolerance and lack of knowledge about the care provided within the scope of the RR project, the prevalence rate was 8.3%, 8.4% and 4.1%, respectively. The nursing diagnoses of ineffective airway clearance and lack of knowledge about the inhalation technique were fully resolved (chart 3).
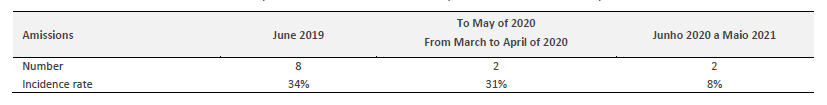
To understand the impact of the project on hospitalisations, the incidence rate of hospitalisations in this population was calculated between the months of June 2019 and May 2020 (1 year before the intervention) and June 2020 and May 2021 (table 2).
The analysis of Table 2 shows that the number of hospitalisations in the year prior to the implementation of the project was 8, while in the year during which this project took place, the number was 2, which is identical to the number that occurred in the 3 months during which this population was deprived of CR. With regard to the incidence rate of hospitalisations, it was found that from June 2019 to May 2020, it was 34%, similar to that presented in the time period from March to May 2020. The rate recorded between May 2020 and May 2021 was 8%, a reduction of 76.5% when compared to the previous homologous period.
3. Discussion
The pandemic context in which we have been living since March 2020 imposed the implementation of innovative solutions in the field of health, definitively transforming this field, not only by the challenges imposed, but also by the knowledge acquired and the responses created.
If we consider that the start of the pandemic was marked by bewilderment and the implementation of measures of confinement and closure of health services in the uncertainty of what measures would be the most appropriate, at a later stage the deconfinement and the need to ensure adequate monitoring of people with chronic diseases, marked a Public Health strategy, reasoned, integrated and explicit.
Considering the need to ensure compliance with the criteria for access to health care, to guarantee the rights and legitimate interests of individuals and to ensure the provision of quality health care, the concerted implementation of innovative strategies seems the most appropriate solution, with attempts to adapt to the new reality, an example of which are distance consultations to enable the continuity of safe health care provision.
An example of this is teleconsultation, which appears as a possible response to the gaps created by the restructuring forced by SARS-CoV2, currently constituting a window of opportunity for the reorganization of services and care provision itself. Teleconsultation, along with eHealth, are areas in expansion, recognised for their enormous potential as an adjunct to the sustainability of health systems.
Telemedicine, which is incorporated into health care delivery, already existed before the pandemic, but the pandemic has enabled not only its rapid integration, but also its expansion to new areas of health.
For Ribeiro (2019), information technology in health enhances access to care, allowing to cover populations distant from large urban centres, as well as those living in rural areas.
If we consider that technology has never been as present in our daily lives as it is today, according to Ribeiro (2019), the sustainability of health services has never been more dependent on information technology, since digital capabilities allow for the profitability of existing resources, personalization of care, improvement of outcomes, reduction of costs, and changes in management models in the health system and services.
Increasingly, the focus of healthcare will be on a vision centred on people with the support of technology, always taking into account the balance between face-to-face contact and the use of technological tools.
In a region where geographical discontinuity is high, as is the case of the Autonomous Region of the Azores, digital can be an alternative for healthcare, and can become an asset in the event of restrictions in access to healthcare. However, achieving a balance between this alternative and face-to-face care is indispensable in this process.
Rethinking the path taken, the option for the organisation of a project of this nature respects what is determined for intervention in paediatric respiratory rehabilitation. In fact, the objective is not so much to rehabilitate, but to enable, i.e., to help the child/caregiver to develop new abilities that would naturally arise during his/her development, in the absence of disease or disability. In order to meet the objectives of functional respiratory rehabilitation, its projects involve different specific interventions such as patient and family education, measures to modify risk factors, nutritional and psychosocial support, respiratory functional re-education, exercise training and activities of daily living, optimisation of inhaler therapy and respiratory assistance (Bandeira & Castro, 2003).
In fact, the pedagogical dimension of the project implemented to support paediatric patients with respiratory pathologies sought to improve their breathing patterns and, consequently, their health through crisis prevention. Undoubtedly, it is essential to teach the patients themselves and their parents/carers. Issues such as triggering factors of a crisis, information on controllable factors and correct therapeutic administration should be addressed. It is also crucial, in these projects, to involve the parents/primary caregiver in defining the project, so that therapeutic adherence, which is important to ensure the effectiveness of the rehabilitation treatment, can be ensured (Parentes, 2014). As such, it is of great importance to provide the family with health literacy in order to transform the reality at home beyond the hospital setting (Prato, Silveira, Neves, & Bulbot, 2014).
In this sense, although resources are scarcer at home, this is the place that allows nurses to rehabilitate the person/caregiver/family with a higher degree of adequacy to reality. To this end, the HV became essential, as it was possible to observe, in loco, the housing conditions and family dynamics. As Vilaça et al. (2005) point out, in this regard, the HV is one of the tools nurses can use in their intervention, being able to observe and record the family's activities and socio-affective relationships, the actual context or environment (the housing, hygiene and sanitation conditions) and, consequently, plan and promote activities that encourage self-care according to the identified reality.
The use, in this specific case, of telerehabilitation with regular and systematized consultations and the use of exercises that can be applied and digitally monitored through the use of computers and digital platforms created for this purpose, proved to be an extremely effective measure, allowing on the one hand the continuity of care in the pandemic context and, on the other hand, reducing the risk of spreading the virus.
In the area of respiratory function re-education, the use of telehealth should be a proactive rather than reactive strategy as an alternative to provide services that decrease the impacts of social distancing through the promotion of user-centred care with an emphasis on communication and health literacy (Gronkievwicz & Coover, 2011).
Telerehabilitation is defined as the provision of rehabilitation services through information and communication technologies. The literature lists benefits to the telehealth model. This model allows shifting the locus of control from the professional to the user and can improve patient education, self-management, outcomes and satisfaction, as well as strengthen the user-health professional alliance.
The combination of the HV and RCT allowed the initially outlined objective to be successfully achieved. In fact, with regard to the nursing diagnoses of ineffective airway cleaning and lack of knowledge of the inhalation technique, the interventions ensured a 100% resolution rate when the initial proposal was 90%. As regards the nursing diagnoses knowledge deficit about the care provided within the scope of the RR project, the resolution rate reached 93.8%, with a prevalence rate of 4.1%. It should be recalled that the proposed resolution rate for this diagnosis would be 80%. As regards impaired ventilation, the diagnostic resolution rate was considerably high (88.9%), which influenced the decrease of the prevalence rate 75% to 8.3%. Even so, the 90% resolution rate was not reached, with a slight deviation of 1.1%. In relation to the diagnosis of activity intolerance, the prevalence rate was reduced from 37.4% to 8.4%, with a resolution rate of 77.7%, against the proposed 90%. It should be noted that the observed deviation is associated with more complex clinical situations, and it was not possible to reverse the nursing diagnosis as proposed.
These results confirm the effectiveness of the outlined project in reducing the prevalence rate of nursing diagnoses. As a direct consequence of this reduction, the satisfaction of the individuals in the sample and their parents with the results obtained is noted, as well as the decrease/reduction of hospital admissions. In fact, 8 of the individuals had a history of one or more hospital admissions for respiratory disease in the previous year, but after the RR project, two readmissions were registered in the same time frame, with an incidence rate of hospitalisation falling to 76.5%, instead of the 40% initially proposed when the project was designed.
According to the classification system of patients in Homogeneous Diagnosis Group - DRG contemplated in Ordinance 207/2017, the cost of a hospitalisation for respiratory tract infection and for Cystic Fibrosis can oscillate, according to the level of severity, between 1 and 4. In order to calculate an estimate of the economic costs that a hospitalisation for these pathologies represents for the state, a midpoint was defined, namely level 2, with an estimated cost of 2427.13€.
Between June 2019 and May 2020, it is estimated that the costs for the region with the hospitalisations of these individuals stood at 19,417.04€. The cost that the hospitalisations represented after the implementation of the project was set at €4,854.26. There is, therefore, a saving of 14,562.78, demonstrating the effective contribution to the prevention of hospital admissions that the project, with an average of 12 sessions, represented.
The results also inform the gains in subjective well-being (SWB) of these individuals and their families, namely in the assessment they make of their lives (life satisfaction, moods and emotions). Subjective well-being, perceived and assessed through individual experiences, is nothing more than the self-assessment manifested by positive affections that outweigh negative ones, by overall satisfaction with life, as well as by satisfaction related to specific aspects or domains, such as health, work, independence, among others (Diener & Suh, 1997 as cited in Sposito et al., 2010).
The method used to measure the SWB was the one suggested by Albuquerque and Tróccoli (2004), consisting of the use of self-report on the satisfaction with their life and the frequency of recent affective emotions of pleasure and displeasure. According to the authors, this form of measurement is the most appropriate since it is up to the individual to assess his/her life satisfaction. Of the various predictors of SWB, health is the most effective one (Simões et al., 2000), although, in SWB, subjective health (the individual's perception of his/her physical condition) is considered as a predictor, rather than objective health (assessed by professionals). A person with health problems may have decreased perceptions of well-being and satisfaction, significantly affecting quality of life.
The investment that the implementation of this project implied was limited to the acquisition of computer equipment that allowed interaction with participants by teleconsultation for the RCT sessions. Even so, the investment was lower than the savings obtained with the reduction of hospitalisations.
In order to objectively assess the users' level of satisfaction with the outlined intervention, we applied the Satisfaction of Users with Nursing Care at the Health Centre - SUCECS26 form, which aims to assess the users' satisfaction with nursing care as a relevant indicator for continuous quality improvement in nursing care. The dimensions under analysis in the SUCECS26 form are: quality of care, individualisation of information, involvement of the user, information on resources, formalisation of information and promotion of the link. The level of satisfaction was 98.5% with regard to information on resources, 97.4% for the promotion of the link and 100% for the remaining dimensions, concluding that the participants in the study were satisfied with the implemented project.
Translated with www.DeepL.com/Translator (free version)
Conclusion
The Paediatric Respiratory Rehabilitation in a Pandemic Context - Respiratory Telekinesiotherapy & Home Visitation project has improved access to RR projects for paediatric patients who were deprived of this care with the closure of the HDES CR Service. Its implementation contributed to reduce respiratory pathology exacerbations, with resolution rates of nursing diagnoses ranging from 77.7% to 100%. It was also possible to realize that this reduction in the prevalence rate contributes to a greater subjective well-being in the dimension of subjective health, according to the individual assessment of paediatric patients and their parents/caregivers. The reduction in the prevalence rate of nursing diagnoses has a direct influence on the likelihood of hospital admissions, being, therefore, avoidable, leading to a reduction of costs with hospital admissions, as its incidence rate suffered a positive variation of 76.5%. With the application of the SUCECS26 form, the satisfaction of participants with the implemented intervention was confirmed. Despite this being the greatest recognition that one can have, it must be underlined that this project, Paediatric Respiratory Rehabilitation in a Pandemic Context: Respiratory Telekinesitherapy and Home Visitation, was a finalist in the 14th Edition of the Good Health Practices award, in the category of best project, won the 10th Edition of the Sustainable Health Award in the category of integration of care, and was the winner of the 2nd edition of the Luísa Soares Branco Award. All this culminated in a vote of congratulation unanimously approved by the Legislative Assembly of the Azores Autonomous Region.
In this sense, this research proves that simple measures and creative strategies can represent an effective measure of improvement for health care and, in this case, rehabilitation, with direct implications on the quality of care and, consequently, on the lives of those who benefit from it.