Introduction
In Portugal, Ambulatory Surgery (AS) is legally framed in Ordinance no. 163/2013 of 24 April, and is defined as a "scheduled surgical intervention, performed under general, loco-regional or local anaesthesia, which, although usually performed in an inpatient setting, can be safely performed in own facilities in accordance with the current legis artis, in an admission and discharge regime within a period of less than twenty-four hours". According to Order No. 1380/2018, published in the Official Gazette on 8 February, the AS represents an important instrument for increasing effectiveness, quality of care and efficiency in the hospital organisation, allowing the patient to recover in a familiar environment, thus enabling an organisation of the hospital structure in order to dedicate hospitalisation to the most complex situations, rationalising health expenditure with a correct reorientation of hospital costs. It has well-defined clinical and social inclusion criteria. Balona (2016) mentions that AS aims at increasing patient satisfaction and providing a better response in terms of community health, by reducing the number of hospitalised patients, reducing the rate of healthcare-associated infections, and shortening waiting lists.
With the increase in the number of chronic diseases, whose causes have been related to lifestyle, psychological and social factors stand out.
For Dela Coleta (2010), social psychology has provided specific or applicable theoretical contributions to the area of health, with several works appearing in recent years seeking to explain the role of variables and psychosocial processes in the prevention, treatment and maintenance of health behaviours. Thus, according to this approach, every human event is a bio-psycho-socio-cultural phenomenon. From this perspective, the surgical act, involves the totality of factors involved, from the person's reactions to the diagnosis to the need for surgery, as well as the culture and psychosocial context in which the patient is inserted, such as family support in the postoperative period. Any new or unknown event generates in people a feeling of anxiety and fear. Anxiety is the reaction to danger or threat. In the context of surgery, it is possible that the anticipation of this event triggers potentially negative feelings based on each individual's cognitive assessment. According to CIPE 2015 (ICN 2016, p. 40), anxiety is a "negative emotion: feelings of threat; danger or distress".
The fear of pain, anaesthesia and surgery, can be overwhelming for many people. According to Breda (2019), throughout the various phases of the surgical process, patients express a fear related to the immediate postoperative period, namely regarding pain, nausea and vomiting, the beginning of feeding and the first rising, but also, uncertainties with the moment of discharge and post-surgical recovery at home. The nurses involved in the process should also reassure the patient by providing all the necessary information and clarifications so that he/she does not experience this feeling.
Social support is important in the context of adherence and adaptation to the surgical process. The presence of a companion at discharge and the presence of an adult for the first 24 hours after surgery are considered inclusion criteria for AS (Manual of Good Practice in Ambulatory Surgery, 2019); however, living far from the hospital, in a house with many stairs and no lift, and not having transportation are exclusion criteria for AS. Given the importance of psychological and social factors, it would be essential to standardise the psychosocial factors for inclusion of patients in AS.
This study aimed at mapping the scientific evidence on psychosocial factors for the inclusion of patients in AS. Thus, the following research question emerged: What are the psychosocial factors for patient inclusion in ambulatory surgery?
1. Methods
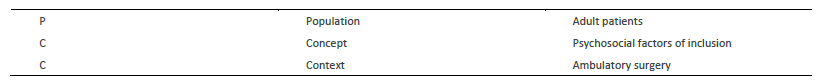
Scoping reviews, according to the Joanna Briggs Institute eligibility criteria (Peters et al, 2020), presuppose rigour and transparency and can potentially contribute to the advancement of knowledge about healthcare practice, policy and research. This scoping was guided by the PCC strategy (P: population, C: concept and C: context), which is presented in table 1.
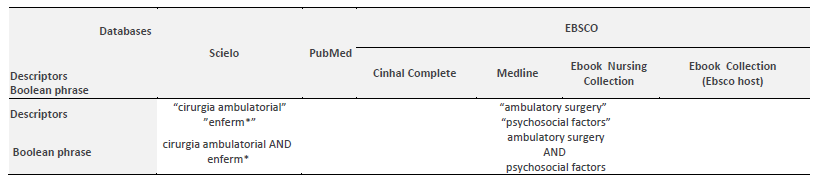
To search and collect data, we used the SCIELO and PUBMED platforms and, via EBSCO, the CINHAL Complete, Ebook Nursing Collection, Ebook Collection (Ebsco Host) and MEDLINE using the descriptors "psychosocial factors", "ambulatory surgery", "ambulatory surgery", "nurs*" and the Boolean operator AND, resulting in the search strategy shown in table 2.
The inclusion criteria defined for the search were academic journals, studies written in English and Portuguese, with accessible full text. The exclusion criteria were studies conducted within the scope of paediatrics. The studies were selected based on the titles and abstracts, when available, according to the inclusion criteria initially described. In cases of doubt, the full text was read, with the objective of obtaining more elements for the decision as to the relevance of the material for review. This was carried out by two independent reviewers, and the possible different opinions were resolved in a consensual manner, with the purpose of validating the eligibility of a given publication.
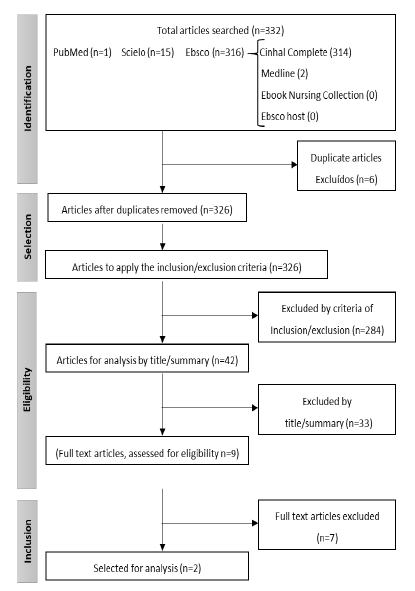
Figure 1 below shows a representative scheme of the article selection according to the PRISMA-ScR methodology (Tricco et al., 2018).
2. Results
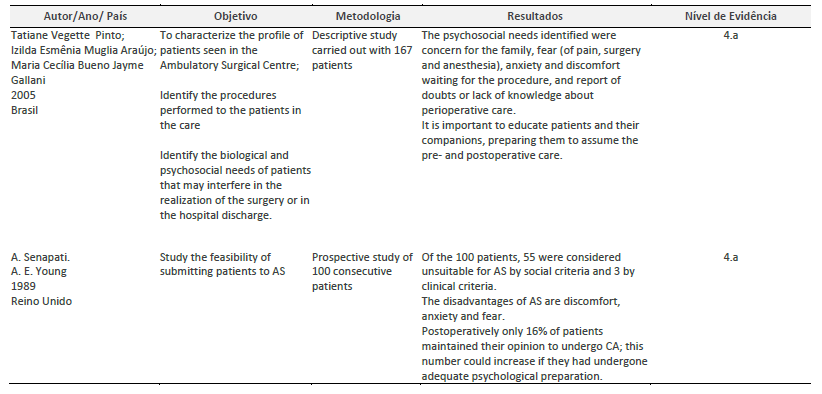
For a better organization of the extracted data, an instrument was developed as shown in Table 3, based on the Joanna Briggs Institute Manual (Peters et al., 2020) with the most relevant information to answer the initial question. The level of evidence was classified according to Joanna Briggs Institute (2014).
Two articles were included in the study which highlighted as psychosocial factors the fear of pain, anesthesia, surgery, anxiety, discomfort, the existence of a companion/caregiver at home, living with many stairs, no lift and being far from the hospital and having no transport.
According to Senapati et al (1989), most patients were considered unfit for AS, of which 3 by clinical criteria and 55 by social aspects. All were asked before surgery and after discharge whether they preferred the ambulatory or inpatient regime and only 16% of patients maintained the choice for AS. This number could have increased, i.e. adherence to AS, if they had had adequate psychological preparation.
According to Pinto et al (2005), most interviewees had some information on the surgical process, had performed the minimum preoperative care and were able to list most of the postoperative items, however, half of the group still had preoperative concerns. All patients were prepared to return home, reporting few doubts and showing knowledge about the care to be provided at home, which allowed assessing the guidelines on the postoperative period as adequate and should be encouraged and paid attention to by nurses. A low level of registration was also found, thus the need to establish minimum standards of conduct and registration is evident.
3. Discussion
The person who will undergo a surgical procedure should be cared for in a holistic way, based on the assumption that he/she is a biopsychosocial being and that his/her emotional state will inevitably affect his/her physical condition (Costa et al., 2010).
Both articles recognised the existence and importance of psychosocial factors in patients selected for AS, such as fear, anxiety, discomfort and social support. Patients' level of anxiety in the preoperative period has been associated with numerous personal and social factors which should be determined so as to allow for an appropriate management of pre- and postoperative anxiety, namely personalised interventions in people with risk factors, with a view to making the operative experience safer (Cunha, 2011). Silva and Amorim (2017), who aimed to assess the relevance and benefit of pre-surgical nursing consultations to alleviate anxiety, concluded that this type of adequate and consistent consultation is essential to reduce levels of discomfort and insecurity. In our clinical practice in AS, we perceived that patients experience, throughout the surgical process, multiple emotional conflicts caused by the fear of the unknown and anxiety related to doubts and uncertainties associated with the surgical procedure, recovery and need for support after discharge.
Both authors emphasised the importance of an adequate preoperative psychological preparation, as well as the clarification of all doubts and the provision of continuous information, as pointed out by Gonçalves et al. During our professional practice, we found that this previous psychological preparation promotes patients' adherence to AS.
The provision of information to patients is essential both to increase their knowledge and help them adapt to lifestyle changes after surgery. Nurses must focus their care not only on the technical, but also on the psychosocial aspects (Bayraktar et al, 2018).
Pinto et al (2005) recommended the establishment of minimum standards of care to meet the detected needs through continuous information, and also encouraged the health care team to keep records of perioperative interventions and conditions. Nursing records allow visibility to nurses' autonomous decision-making (Martins et al., 2008).
Although Segal & Fandiño (2002) consider that there is no consensus on the psychological and psychiatric criteria for exclusion from surgery, which is the responsibility of the multidisciplinary team, other authors, such as Machado et al (2015), agree that it is necessary to establish a dialogue in the preoperative period to convey information about the procedures and nursing interventions and, essentially, to share the patient's emotions.
In fact, there is scientific evidence that psychosocial factors exist in the context of AS, but it was not possible to identify them as psychosocial factors for patient inclusion in this regime.
Conclusion
AS has undergone an accentuated development over the last decades, thus improving the well-being and safety of the patients who resort to this type of surgery, promoting a quick family and professional reintegration. However, not everyone can be submitted to this type of intervention, as there is a series of defined inclusion criteria that should be respected: the clinical and social ones, aiming at a careful selection of patients and adequate procedures, both from the surgical and anaesthetic point of view.
Despite the concern with psychological factors in the surgical process, there is a lack of articles that demonstrate them as predictive factors of good or bad prognosis or of the effectiveness of the surgical procedure.
We consider this study to be relevant, since the articles emphasise the importance of psychosocial factors, thus influencing adherence to AS and conditioning its effectiveness and success; however, we found no scientific evidence that would allow considering them as inclusion factors in this regime.
Among the limitations of our study, we highlight the gaps in the production of scientific knowledge, as well as the lack of research on the Portuguese reality.
This study contributed to gather information on the importance of psychosocial factors in OS, and may be used as a basis for the creation of an assessment tool and promote the development of new studies that allow introducing them as inclusion factors for OS patients.
As a final reflection, we believe that the contributions of this study should be taken into account as it is an update of the existing scientific evidence on this topic. It allowed understanding the importance of adequate psychological preparation, promoting the nurses' role in this area, through the continuous improvement of nursing care, with gains in health.