Introduction
Globally, Healthcare-Associated Infections (HAIs) are considered a serious public health problem (Bekele et al., 2020) and frequently occur in healthcare facilities (Dhedhi et al. 2021). Annually, according to the European Center for Disease Prevention and Control (ECDC), it is estimated that 3.1 million people contract HAIs. Between 2016 and 2017, Portugal had a prevalence of HAIs of 9.1%, the second highest in Europe (OECD, 2018).
Health professionals, particularly nurses, have an increased risk of acquiring infections, assuming a relevant role in formulating and implementing policies that contribute to the control, prevention, and minimization of infections. (SookKyoung et al., 2021).
The Standard Precautions (SP), proposed by the United States Centers for Disease Control and Prevention (CDC), are basic guidelines to reduce the risk of transmission of microorganisms and protect health professionals from infectious diseases, through recommendations for safe practices of infection control in health institutions (DGS, 2017; Dhedhi et al. 2021). These recommendations include hand washing, proper use of gloves, use of personal protective equipment (EPI), respiratory etiquette, safe injection practice, patient placement, workplace exposure hazards, safe handling of clothing, safe waste collection, treatment of clinical equipment, and environmental control.
According to the Annual Report on Infections and Antimicrobial Resistance (2018), the overall percentage of compliance with good hand hygiene practices situated at 73.6% in 2017, and compliance with the use/replacement of gloves is situated up to 82.3%. The same states that the health professional has an increased risk of 1.2 to 10% of acquiring VHC infections after being bitten. According to the study developed by SookKyoung and his collaborators (2021), it was found that 60.4% of nurses reported having suffered a needlestick injury. The same study reports that participants' knowledge of respiratory etiquette is 82%.
The PP was adopted in Portugal called Basic Infection Control Precautions (PBCI), complying with the standard published by the General Directorate of Health (DGS) constituting the basis of good care practices. They aim to prevent the transmission of HAIs and simplify the dissemination, understanding, and implementation of its different components. These measures must be used in all users, regardless of their infectious status, to guarantee the safety of the user, the professional, and the citizens who come into contact with the health services (DGS, 2017).
Some factors influence adherence to PBCI, namely the unavailability and inaccessibility, and resistance of professionals to the use of EPI, inadequate knowledge about PBCI, low perception of the effectiveness of prevention and risk perception, lack of support by management for safe work practices and lack of professional performance feedback (Bekele et al., 2020).
Knowledge, awareness, and compliance with PBCI are important conditions for reducing HAIs. In a study carried out by Dhedhi and his collaborators (2021), it was found that 12.2% of the participants had little knowledge about the proper use of SP. However, despite its importance in reducing the transmission of infectious agents in the workplace, there are low adherence rates among health professionals (Al-Faouri et al., 2021). Data from a study carried out by Brandão and his collaborators (2022) reveal that health professionals comply with SP by 66.8%. Another study developed by Wong and his collaborators (2021) alludes to low adherence when caring for the user (54%) and performing invasive procedures (46%).
To increase adherence to the PBCI and reduce/eliminate the factors that influence non-adherence, managers must promote the existence of facilitating resources, the implementation and access to norms, procedures, and guidelines, and guarantee the education and continuous training of professionals of health and the supervision of clinical practices. To this end, actions must be developed that involve a combination of education, awareness, and organizational, environmental, and management changes, which must go far beyond the individual focus. (Al-Faouri et al., 2021).
A previous search conducted in CINAHL® Plus with Full Text and Nursing & Allied Health Collection via EBSCO, and MEDLINE® via PubMed revealed the lack of published literature reviews in this specific area. In this way, it was decided to carry out the present scoping review that aims to map the factors that influence adherence to standard precautions among/by nurses. This review intends to answer the following research question: What are the factors that influence adherence to SP among nurses in clinical practice?
1. Methods
It was decided to carry out a scoping review protocol based on the methodology proposed by the Joanna Briggs Institute (Peters et al., 2020). This type of study allows for more in-depth and up-to-date knowledge about the phenomenon under study and the identification of existing gaps. This protocol aims to map the factors that influence adherence to standard precautions among/by nurses (Aromataris & Munn, 2020). In the search for scientific evidence, the PCC strategy (population, concept, context) was used, as shown in Table 1 (Tricco et al., 2018).
Tabela 1 PCC Acronym.
| Population (P) | Nurses in care delivery |
| Concept (C) | Factors that influence adherence to PBCI by nurses |
| Context (C) | Clinical practice |
A three-stage research strategy was adopted (Peters et al., 2020), the first of which began with an initial search in the CINAHL® Plus with Full Text and Nursing & Allied Health Collection databases via EBSCO, MEDLINE ® via PubMed, which allowed the identification of the most frequently used words in titles and abstracts, as well as the indexing terms used. In the second stage, a search was carried out in the databases through the combination of keywords and descriptors that make up the Boolean phrase, which is adapted to each database. The third step consisted of searching pertinent literature reference lists to find complementary studies.
Protocol and registration
This protocol was written per the guiding guidelines by the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR®️) (Tricco et al., 2018). The protocol was registered on the Open Science Framework (OSF) platform (DOI 10.17605/OSF.IO/68VZ7), which can be consulted through the link: https://osf.io/68vz7/.
Eligibility criteria
The inclusion criteria defined for this protocol were studies published between 2017-2022, available in free full text, in Portuguese, English, and Spanish.
This review will consider quantitative, qualitative, and mixed studies, as well as primary studies, systematic reviews, dissertations, opinion articles, and gray literature. As an exclusion criterion, it was defined that studies addressing other professional groups would not be considered. Subsequently, the lists of references in the literature will be checked to identify complementary studies.
Information sources
The research strategy and identification of studies were carried out in June 2022, in the electronic databases CINAHL® Plus with Full Text and Nursing & Allied Health Collection via EBSCO, MEDLINE® via PubMed using the following descriptors, as shown in Table 2. It should be noted that no evidence of the scoping review type was found on this topic. Keywords included in titles and abstracts of significant articles will be used to develop the full search strategy.
Tabela 2 Search descriptors
| Descritores DeCS | ||
| Inglês | Espanhol | Português |
| Knowledge | Conocimiento | Conhecimento |
| Nursing | Enfermería | Enfermagem |
| Infection Control | Control de Infecciones | Controle de Infecções |
The Boolean operators AND and OR will be used, with AND being used to identify studies between themes and OR for synonyms, according to the combinations between the descriptors, according to Table 3.
Tabela 3 Descriptors and synonyms used in databases.
| Base de dados | Termos controlados |
| Pubmed | ("Knowledge"[MeSH Terms] OR "Knowledge"[Title/Abstract]) AND ("infection control"[Title/Abstract] OR "infection control"[MeSH Terms]) AND ("Nursing"[MeSH Terms] OR "Nursing"[Title/Abstract])" |
| Medline | TX Knowledge AND TX Infection Control AND TX Nursing |
| Cinahl | TX Knowledge AND TX Infection Control AND TX Nursing |
| Nursing & Allied Health Collection | TX Knowledge AND TX Infection Control AND TX Nursing |
Selection of studies
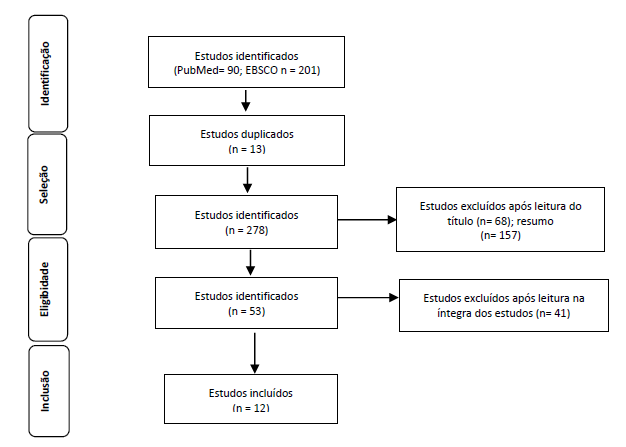
After the research, the articles will be deposited in the Rayyan program and the duplicates will be removed. The studies that constitute the corpus of analysis of this review will be obtained through a strategy that contemplates the identification, selection, eligibility, and inclusion of the same conducted by the inclusion criteria and by the search limiters. Subsequently, the title and abstract will be read and then the selected studies will be read in full. Data will be extracted from the studies included in the scoping review by two independent reviewers, resorting to a third reviewer in case of disagreement, who will decide on the inclusion or exclusion of the article. The results will be written according to the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR®) (Page et al., 2020). The selection process will be documented through a PRISMA flow diagram, as shown in Figure 1 (Tricco et al., 2018).
2. Data presentation
Were identified 12 articles that will be synthesized and presented descriptively and narratively using an evidence table constructed by the researchers, which contains the following items: the study code and author(s), country and year, type of study, objective(s) and the main results according to table 4. The identification, characterization, and synthesis of knowledge in this area will seek to be aligned with the objectives and the proposed review question. The results will later be reported in full in the final scoping review and presented according to the Preferred Reporting Items for Systematic Review and Meta-Analyses Extension for Scoping Reviews (PRISMA-ScR) for preparation of the final article.
Conclusion
It is expected that this review will constitute a starting point for mapping the available scientific evidence regarding the factors that influence adherence to basic infection control precautions among nurses. It will contribute to defining interventions and/or programs that maximize compliance with basic precautions, minimize repercussions on clinical practice and improve healthcare quality.
Author contributions
Conceptualization, M.F. and M.S.; data curation, M.F. and M.S.; formal analysis, M.F., M.S., J.T., A.L. and T.M.; investigation, M.F., M.S., J.T., A.L. and T.M.; methodology, M.F. and M.S.; project administration, M.F. and M.S.; resources, M.F., M.S., J.T., A.L. and T.M.; validation, M.F., M.S., J.T., A.L. and T.M.; visualization M.F., M.S., J.T., A.L. and T.M.; writing-original draft, M.F. and M.S.; writing-review and editing, M.F. and M.S.