Introduction
According to the Medical Subject Headings (2017), the nursing workload is defined as the total amount of work to be performed by one or more nurses in a given period. In the critical care setting, in which patients require specialized care due to risk to life or the risk of organ or multiorgan failure, or in which differentiated treatments are needed (Ordem dos Enfermeiros, 2018), nurses implement interventions to meet patient needs in numerous clinical contexts and/or in care transitions. The inter-hospital transport of critically ill patients arises in response to these patients’ need for clinical treatments and follow-up involving advanced technologies and specific techniques and knowledge, to improve the quality of care provided (Eiding et al., 2019; Kiss et al., 2017).
Increasing clinical specialization, combined with the demand for sophisticated technologies, has led to a growing need for inter-hospital transfers of critically ill patients to ensure the best possible care (Kiss et al., 2017). It is associated with multiple risks and is recognized as a highly challenging process requiring further study (Dabija et al., 2021; Eiding et al., 2019). These transfers are fundamental in the management of patients requiring care from specific specialties and diagnostic and/or therapeutic technologies that are unavailable at the clinical center of origin (Ordem dos Médicos (Colégio de Medicina Intensiva) & Sociedade Portuguesa de Cuidados Intensivos, 2023).
Inter-hospital transport of critically ill patients, guaranteeing the continuity and quality of care, can be a challenge (Eiding et al., 2019). The level of care provided during the inter-hospital transfer of these patients cannot be lower than that provided at the unit of origin (Dabija et al., 2021), and may potentially need to be increased during transport (Ordem dos Médicos (Colégio de Medicina Intensiva) & Sociedade Portuguesa de Cuidados Intensivos, 2023).
Critical care nursing is defined as specific care aiming to ensure the continuing provision of care to a patient at risk of death due to an organ or multiorgan failure, aiming to respond to the patient’s needs by maintaining vital functions to prevent complications and future disabilities, to promote a total improvement (Ordem dos Enfermeiros, 2018). Inter-hospital transport involves an increased workload for nurses due to the transfer of the patient, which can lead to complications, in an unknown environment in which there may be machine failures/backup system failures, and even human error either by nurses or physicians (Dabija et al., 2021; Eiding et al., 2019; Lee & Jeong, 2018; Kiss et al., 2017). Thus, while inter-hospital transport can save lives it can also put the patient at risk (Dabija et al., 2021; Eiding et al., 2019).
The workload is one of the stressors among nurses in inter-hospital transport, and an increasing workload can lead to physical, psychological, and behavioral reactions (Dabija et al., 2021; Lee & Jeong, 2018; Eiding et al., 2019; Kiss et al., 2017). Thus, the workload must be calculated correctly to allow adequate work allocation. Nurses’ workload can be calculated using a variety of methods, including the subjective perception of work intensity, average time spent to complete the main activities, and directly with the use of objective workload assessment instruments (Lee & Jeong, 2018).
This study aimed at mapping the available evidence on nursing workload in the inter-hospital transport of critically ill patients. Thus, the following research question emerged: What is the workload of nurses in the inter-hospital transport of critically ill patients?
1. Methods
A scoping review was conducted to analyze/identify gaps in the current knowledge and to characterize the key characteristics and factors involved in this topic (Peters et al., 2021).
A scoping review was performed according to the recommendations set out by the Joanna Briggs Institute (JBI) (Peters et al., 2021) and the Preferred Reporting Items for Systematic Reviews and Meta-Analyses extension for Scoping Reviews (PRISMA-ScR) checklist (Page et al., 2021).
The review employed the framework of the population, concept, and context (PCC) eligibility criteria proposed by JBI (Peters et al., 2021). Regarding population, we considered studies on critical care nurses. With respect to concept, studies addressing workload are reviewed. Finally, the context studied was inter-hospital patient transfers.
Preregistration of the study was carried out in Open Science Framework, entitled “Nurses’ workload in the inter-hospital transport of critically ill patients: a protocol of scoping review”, with Registration DOI: 10.17605/OSF.IO/W27TD, available in Internet Archive link: https://archive.org/details/osf-registrations-w27td-v1.
The international research standards contained in the World Medical Association Declaration of Helsinski (2013) were followed in this scoping review, without the participation of human beings, it is exempt from approval by an ethics committee.
A search strategy (Table 1) was developed according to the three steps defined by the JBI (Peters et al., 2021) to gather all published and unpublished articles. The initial search was limited to the MEDLINE (PubMed) and CINAHL Complete (EBSCOhost) databases to evaluate the search terms through analysis of the words included in the titles, abstracts, and descriptors of the articles identified. In the second stage, using the keywords and descriptors identified, a search was conducted on the following databases: MEDLINE (PubMed), CINAHL Complete (EBSCOhost), Scielo, Cochrane (EBSCOhost), LILACS, and MedicLatina (EBSCOhost). In the third stage, the RCAAP, DART-Europe, and OpenGrey databases were searched to identify articles from the grey literature. Websites are relevant to the area of study and articles cited in reference sections were also included in the review.
Table 1 Search strategy
| Strategy | Database | Results |
|---|---|---|
| (((Workload[Title/Abstract]) OR (Workload[MeSH Terms])) OR ((Staff Workload[Title/Abstract]) OR (Staff Workload[MeSH Terms]))) AND (((Patient Transfer[Title/Abstract]) OR (Patient Transfer[MeSH Terms])) OR ((Transportation of Patients[Title/Abstract]) OR (Transportation of Patients[MeSH Terms]))) | MEDLINE | 110 |
| (((TI Workload) OR (AB Workload) OR (MH Workload)) OR ((TI Staff Workload) OR (AB Staff Workload) OR (MH Staff Workload))) AND (((TI Patient Transfer) OR (AB Patient Transfer) OR (MH Patient Transfer)) OR ((TI Transportation of Patients) OR (AB Transportation of Patients) OR (MH Transportation of Patients))) | CINAHL Complete | 67 |
| Cochrane | 2 | |
| MedicLatina | 81 | |
| (((Workload) OR (Staff Workload)) AND (Patient Transfer)) | Scielo | 5 |
| LILACS | 6 | |
| OpenGrey | 29 | |
| DART-Europe | 7 | |
| RCAAP | 23 |
Articles were selected according to the framework proposed by the JBI (Peters et al., 2021). Concerning study design, the review included all qualitative and quantitative primary research articles, literature reviews, and grey literature. Abstracts, communications at conferences, and opinion articles were excluded.
The review included articles published in Portuguese, Spanish, and English, with no limitation on the time of publication. The search was conducted between 3 December 2021 and 18 January 2022.
All the studies identified were organized using the EndNote® software. Duplicate articles were eliminated. Two independent reviewers (MR and LM) analyzed the titles and abstracts of the articles identified to assess their relevance. Both examined the full texts of the articles to verify that they met the selection criteria. Disagreements were resolved by consensus, without the need for recourse to a third reviewer. Full texts were recovered for all articles meeting the pre-established selection criteria.
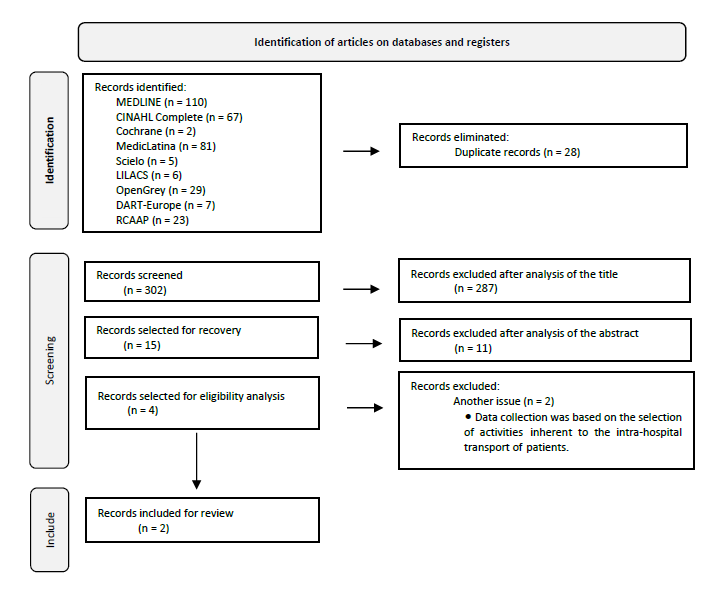
The article selection process is presented with the PRISMA-ScR flow diagram (Page et al., 2021). This selection process is shown in the PRISMA-ScR flow diagram (Figure 1), which presents the results of the three main stages of identification, screening, and inclusion. Of 302 eligible articles, two focused on nursing workload in the context of inter-hospital transport of critically ill patients and were finally included for review.
2. Results
Data were extracted from the selected articles according to a structure developed for this scoping review by the study objectives and the study topic, as recommended in the JBI manual (Peters et al., 2021). Data were organized by author(s), year of publication, country, objective/purpose, sample, study design, and results (Table 2).
Table 2 Data extraction.
| Number | Author(s) | Year | Country | Objective/purpose | Sample | Study design | Results |
|---|---|---|---|---|---|---|---|
| 1 | Blay, Duffield, & Gallaghe | 2012 | Australia | To discuss the impact of the patient transfer on nursing workload and patient outcomes. To discuss the literature on patient transfers, nursing workload, and patient safety. | - | Review | Measures to increase patient flow result in an increase in patient transfers and nursing workload. Frequent patient transfers may increase the risk of medication incidents, infections, and falls. |
| 2 | Mueller, Fiskio, & Schnipper | 2019 | United States | To examine the association between certain characteristics of the transfer process, including time of transfer, the workload of the admitting care team, and the clinical outcomes of patients transferred. To examine the association between “weekend” transfers, “night-time” transfers, “time delay” between transfer acceptance and hospital arrival, and “busyness” of the admitting team on the day of the transfer. | Retrospective analysis of patients aged ≥ 18 years who were transferred to the Brigham and Women’s Hospital, a tertiary-level hospital with 777 beds, from another acute care hospital, between January 2005 and September 2013. | Retrospective study | Among the 24 352 patients transferred, night-time transfers were associated with an increase in the adjusted odds of transfer to the intensive care unit. These results suggest that critically ill patients present poorer outcomes when transferred outside of peak hours and at times of high care team workload. |
Levels of evidence were characterized according to the system proposed by the JBI (Peters et al., 2021). A narrative review was performed to develop a qualitative synthesis of the data reported in the studies (Bardin, 2016). The reviewers conducted a thematic review of the content of the articles, identifying themes aligned with the study objective and the implications for future research, evaluating policies and their implications. In the results section, we describe the themes identified in the literature on nursing workload in the context of inter-hospital transport of critically ill patients.
The article selection process demonstrated an intensive workload, with the increased responsibility of the nursing team in the context of inter-hospital transport of critically ill patients.
The studies included for review were conducted in Australia (n = 1) and the United States (n = 1)., presenting different study designs: one review (n = 1) and one retrospective study (n = 1).
From the analysis of the results, three key themes were identified: time management, human resources management, and transfer time.
Time management
Inter-hospital transport has a significant impact on nurses’ workload and responsibilities due to the limited available time for managing the transfer, concerning patient assessment and familiarisation, workload planning, and care provision throughout the transfer process (Blay et al., 2012). Admission of a critically ill patient to the destination hospital after transfer also has a significant impact on the time and workload of the admissions team (Mueller et al., 2019).
Human resources management
The increase in night-time transfers, during shifts in which nurse staffing ratios are typically lower than during day-time shifts, further decreases staffing levels, consequently increasing workload and the impact on the staff (Blay et al., 2012). Staffing of the admissions team at the destination hospital is also reduced at the time of arrival (Mueller et al., 2019).
Transfer time
Night-time transfers have become increasingly common over the years; this period is characterized by lower nurse staffing ratios than during day-time shifts, which has a significant impact on nursing workload (Blay et al., 2012). Night-time and weekend transfers are associated with poorer outcomes (Mueller et al., 2019).
3. Discussion
The scarcity of studies on nursing workload in the context of inter-hospital transport of critically ill patients demonstrates the currently limited body of scientific research into this topic. As a result, the work required of nurses in this context remains largely or completely unacknowledged about the additional workload and, consequently, the need to increase nurse staffing ratios in response to the transfer requirements.
The studies reviewed were published in Australia and the United States, countries with mixed public-private healthcare systems where insurance coverage is needed to access healthcare. As transfer services are not covered by this insurance, the results of these studies cannot be extrapolated to other countries.
The poor level of evidence of the studies reviewed further demonstrates the pressing need for additional research into nursing workload in the context of inter-hospital transport of critically ill patients, both due to the shortage of evidence and due to the characteristics of the countries in which research has been conducted and the limited available evidence on the current situation.
Thus, given the relevance of this scoping review, which aims to map the scientific evidence on nursing workload in the context of inter-hospital transport of critically ill patients, three main themes were identified: time management, human resources management, and transfer time.
The studies reviewed show that the inter-hospital transport of critically ill patients does have an impact on the nursing workload. The negative impact of these transfers on nursing workload (Eiding et al., 2019) can only be fully understood if the workload measured takes into account every aspect of patient transfers (Blay et al., 2012). Patients transferred between hospitals are more vulnerable to the workload of the admitting team at the destination hospital (Mueller et al., 2019). The impact of these transfers on nursing workload and the responsibilities of nursing staff has recently been recognised (Dabija et al., 2021; Eiding et al., 2019; Kiss et al., 2017), but is not currently considered in measures of nursing workload (Blay et al., 2012).
With the growing sophistication of healthcare provision, these patient transfers will also become increasingly common to meet patients’ clinical needs (Eiding et al., 2019; Mueller et al., 2019; Kiss et al., 2017). Many critically ill patients are transferred to other institutions to undergo imaging studies or for management by other clinical specialties (Eiding et al., 2019; Kiss et al., 2017). We must not underestimate the frequency of these transfers or dismiss their substantial impact on the workload of nursing staff (Blay et al., 2012).
The inter-hospital transport of critically ill patients involves an intense workload, and the transfer of intensive care patients by a nurse has an impact on the time management of nursing staff (Eiding et al., 2019), potentially resulting in the equivalent of seven workload hours. Pre-transfer preparations take an average of 22 minutes and post-transfer activities can take 31 minutes, demonstrating the significant impact of these transfers on nursing workload (Blay et al., 2012). With the high number of transfers performed, the time dedicated to these patients may be limited (for instance, resulting in “work compression,” the attempt to provide the same amount of care in a shorter time) (Mueller et al., 2019). Independently of the destination service, the inter-hospital transport of critically ill patients limits the time available to nurses for patient evaluation and familiarisation, workload planning, and care provision (Dabija et al., 2021; Kiss et al., 2017; Blay et al., 2012), resulting in a reduction in the available time for the provision of care to the patient being transferred (Conde et al., 2021; Mueller et al., 2019).
Nurse staffing ratios also have an impact on the care provided to patients, insofar as the need to transfer critically ill patients to another centre reduces staffing ratios at the centre of origin, which subsequently impacts human resources management due to the increased nursing workload (Eiding et al., 2019; Blay et al., 2012); likewise, staff availability at the destination service is also reduced during admission of the patient (Kiss et al., 2017; Mueller et al., 2019).
Transfer time also has an impact on the inter-hospital transport of critically ill patients, with night-time transfers, particularly from Friday to Sunday, being associated with poorer outcomes (Mueller et al., 2019).
Conclusion
The nursing workload in the context of inter-hospital transport of critically ill patients is largely unacknowledged at present.
Nurses involved in these transfers must guarantee the continuity and quality of care provided to these patients, maintaining the level of care provided at the hospital of origin and even, where necessary, increasing the level of care, in a setting of constant interdisciplinary collaboration. The review highlights the impact, in terms of time, that these transfers have on nursing workload: the role of nurses in this context is fundamental and becomes increasingly challenging due to the limited available time for patient evaluation and familiarisation, planning, and care provision.
The intense workload and time demands associated with inter-hospital transport of critically ill patients, together with the reduction in nurse staffing levels during night shifts, have a significant impact on the nursing workload. Nurses play a key role in every stage of the inter-hospital transport of critically ill patients.
The limitations of this study are related to the scarcity of existing evidence on the nursing workload in the context of inter-hospital transport of critically ill patients.
The studies included in the review were not conducted in Europe. Given their low level of evidence, there is a need for experimental studies analyzing the impact of these transfers on nursing workload.
Identifying issues related to nursing workload in the context of inter-hospital transport of critically ill patients offers a picture of the state of the art in the area, enabling the development of projects to meet nurses’ actual needs in this context.
Acknowledgments
The authors thank Jack Leyden for his help with the English translation of the manuscript.
Author contributions
Conceptualization, M.J.R., L.M. and A.S.P.; data curation, M.J.R. and L.M.; formal analysis, M.J.R. and L.M.; funding acquisition, M.J.R., L.M. and A.S.P.; investigation, M.J.R. and L.M.; methodology, M.J.R. and L.M.; project administration, M.J.R; resources, M.J.R., L.M. and A.S.P.; software, M.J.R. and L.M.; supervision, M.J.R.; validation, M.J.R., L.M. and A.S.P.; visualization, M.J.R., L.M. and A.S.P.; writing - original draft, M.J.R. and L.M.; writing - review & editing, M.J.R., L.M. and A.S.P.;