Introduction
Patients hospitalized in the ICU undergo standardization and depersonalization, either by being separated from their personal belongings, which represent support of their individual identity, or by the primary purpose being the satisfaction of their biological needs due to their illness situation (Laerkner et al., 2017).
In this context of illness, they may be subjected to sedation and analgesia techniques, mechanical restraint, and/or the need for invasive mechanical ventilation, through endotracheal intubation or tracheostomy, or non-invasive ventilation, through nasal or facial masks (Pina et al., 2020), which will change the functioning of the phonatory apparatus, or compromise speech intelligibility from moderate to severe (Pinto, 2022), and/or alter their consciousness’ level and neuromuscular function, further restricting communication’s forms, such as writing and non-verbal communication (Gomes, 2020). This event occurs at the worst phase of the critical patient's life, making them fragile and causing their desires, feelings, will, and needs to be postponed (Mortensen et al., 2019).
The loss of speech may lead to serious consequences, such as negative feelings, both in the patient and in those who are trying to communicate with them (Hoorn et al., 2016). Negative consequences for patients include stress, fear, anger, anxiety, frustration, hopelessness’ feelings, and loneliness (Haap et al., 2015a; Pina et al., 2020). Patients mention communication compromise as one of the most stressful, inhuman, and frustrating events during hospitalization (Istanboulian et al., 2019). From the healthcare professionals' perspective, the inability to communicate is associated with feelings of powerlessness, frustration, and dissatisfaction with the care provided (Pina et al., 2020).
The authors Hoorn et al. (2016) and Istanboulian et al. (2019) report that there are various modern communication tools available for healthcare professionals to effectively communicate with critically ill patients; however, these communication tools are not frequently and correctly used by professionals.
In this regard, a study was developed on "Communication with the Critically Ill Patient," involving a literature review and a questionnaire was applied to the multidisciplinary team of the ICU in a National Health Service hospital, evaluating the relevance of the topic of communication with the critically ill patient, identifying communicative barriers and facilitators, and the professionals' knowledge about this topic.
1. Communication with the critically ill patient
Critically ill patient requires intensive care due to the instability, vulnerability, and complexity caused by their illness state and face a high risk of developing further complications, including the risk of death. The illness process and treatment techniques, such as orotracheal intubation and sedative and analgesia medication, deprive the critically ill patient of speaking and communicating their needs, concerns, and symptoms with healthcare professionals, inducing the development of severe emotional reactions (Al-Yahyai et al., 2021; Hoorn et al., 2016; Nyhagen et al., 2023). These reactions can also be induced by the ICU environment because the patients find themselves surrounded by professionals, excessive noise and sensory stimuli, unfamiliar equipment, and materials, often without the ability to question, express, or clarify any doubts (Correia, 2022).
Communication is the ability to generate, send, receive, and perceive messages and interact with other individuals face-to-face or remotely in a particular social context. Usually, humans use speech for communication; however, communication is multimodal because the conveyed message doesn't solely depend on the language used but also on intonation given, context, and body expression, in the case of face-to-face communication (Encarnação et al., 2015).
Communicating with patients is crucial to improving the quality and safety of healthcare. It is highly challenging to understand a critically ill patient who is entirely unable to verbally communication (Hoorn et al., 2016; Gomes, 2020). Communication has assumed a pivotal role as a therapeutic instrument, as the therapeutic relationship is only possible through communication, making these two concepts inseparable (Pinho, 2020).
Lightly sedated patients have shown a desire to communicate, regardless of their critical condition, physical weakness, therapeutic and technologies dependence (Noguchi et al., 2019), therefore, efforts must be made to increase the likelihood of the patient communicating and interacting with the surrounding environment, as it is an important factor for improving care provision and their own recovery and rehabilitation, avoiding isolation, confusion, and complications associated with the loss of the ability to speak (Handberg & Voss, 2018).
The main communication themes in a hospital setting mentioned by patients are pain, comfort (warmth/cold, position, etc.), hunger/thirst, hygiene, and anxiety. Besides basic needs, patients also wish to communicate about their health status, discharge planning, involvement in the decision-making process (Encarnação et al., 2015), and know information about their family, social, and professional contexts (Nyhagen et al., 2023).
Healthcare professionals recognize communication as an extremely important skill, but the inability to communicate verbally, coupled with difficulties in interpreting atypical signals produced by patients, leads to communication challenges, increasing their stress levels and feelings of incompetence, frustration, guilt, dissatisfaction, and despair. This array of emotions leads to abandoning communication attempts, causing the professional to focus only on the physical and technical aspects of interaction (Correia, 2022; Gomes, 2020). Nyhagen et al. (2023) reinforce that professionals and patients sometimes perceive the same situation differently; while professionals are concerned with technical issues, patients might have other concerns, emphasizing the need for comprehensive knowledge about the patient's family and socio-professional aspects.
Literature highlights the negative impact that communication experiences have had on critically ill patients who are unable to verbally express themselves. Studies report the importance that patients admitted to the ICU themselves have to the ability to communicate, allowing them greater participation and involvement in the entire clinical process and increased interaction with family, friends, and caregivers. People undergoing mechanical ventilation reported moderate to severe difficulties in communicating without speaking, attributing negative aspects to the experience of unsuccessful communication attempts, describing it as disturbing, frustrating, and frightening (Pina et al., 2020).
Communication difficulties are reflected in increased stress, depressive symptoms, loneliness, resentment, fears, insecurity, vulnerability, agitation, anger, delirium, and even violence (Pinto, 2022).
Once the impact of communication difficulties on critically ill patients is acknowledged, healthcare professionals have shown greater awareness and sensitivity in dealing with individuals with communication restrictions, implementing strategies to facilitate communication (Pinto, 2022).
AAC (Augmentative and Alternative Communication) is a set of tools and strategies to overcome communication barriers that can be implemented in two ways: through unaided systems, using symbols that do not require a physical aid or tool device (e.g., speech, gestures, sign language), or aided systems, using low-tech devices (e.g., images, photographs, drawings, pictograms, communication boards and tables) and/or high-tech devices (electronic speech-generating devices, specialized computer communication interfaces, among others) (Istanboulian et al., 2019; Lloyd et al., 2018). High-tech AAC software can be installed on a tablet or through a specific speech output system (Lloyd et al., 2018).
As communication facilitation tools/strategies, professionals commonly use: communication boards (alphabet, figures), writing (using paper and pen), lists of activities/questions (with pre-established sentences), and gestures (Gomes, 2020).
Through communication strategies like AAC, patients are able to express their needs, thoughts, and feelings, resulting in fewer misunderstandings overall, optimizing the time professionals spend on this activity (Gomes, 2020). Effective communication increases satisfaction levels and reduces anxiety by enabling patients to convey their concerns to professionals (Al-Yahyai et al., 2021).
The difficulty in implementing changes and forming teams, high staff turnover, lack of incentives for professionals, leading to their demotivation, and heavy workload that doesn't allow professionals time for further training and improvement projects are also aspects cited by some authors as causes of the communication problem with critically ill patients (Pinho, 2020). The limited adaptation and adjustment of practices to the individuality of each patient lead to continued communication difficulties, demanding significant effort from the patient, both at the motor and emotional level (Pinto, 2022).
Data suggests that educating and training a team of healthcare professionals to use AAC, allows to reduce hospitalization times for critically ill patients and their morbidities (Handberg & Voss, 2018).
2. Methods
After consulting the literature evidence regarding the benefits of communication with critically ill patients as a starting point for the present study, the decision was made to evaluate the knowledge of healthcare professionals in communicating with critically ill patients. To achieve this, the following research question was outlined: What knowledge do ICU professionals have about communicating with critically ill patients?
As a secondary research question, the study defined: What are the training needs of ICU healthcare professionals regarding communication with critically ill patients?
The objectives of this study are to evaluate the knowledge of healthcare professionals about communication with critically ill patients in the context of the ICU and to identify the communicative barriers and facilitators with critically ill patients.
Sample
The target population for this study will consist of all healthcare professionals working in the ICU who agree to participate voluntarily in this study by completing informed consent.
As an exclusion criterion, professionals who do not work in the ICU and the researchers of the study, because they are part of the team in question. Therefore, the present sample will be non-probabilistic/intentional, composed of participants who agree to collaborate in the study.
Instruments and Data Collection Procedures
To conduct the research, an exploratory study was chosen. The research design can be characterized as transversal. An instrument composed of two parts was used: sociodemographic, academic, and professional characterization of healthcare professionals working in the IMS; and questions about communication with patients.
To carry out the study, positive opinions were obtained from the Ethics Committee and the Hospital Administration Board where the study was conducted.
Access to the questionnaire was obtained via institutional email for all healthcare professionals providing care in the ICU. Upon accessing the questionnaire, professionals were informed that their participation was voluntary and that all information obtained through the questionnaire was anonymous and confidential, only being used for research purposes, with their privacy being ensured at all times.
Statistical Analysis
In order to achieve the initially outlined objectives, the study results are presented and analyzed.
In the first phase, as previously mentioned, access to the questionnaire was obtained via institutional email for 64 healthcare professionals working in the hospital's ICU, and 46 responses were obtained, representing 72% of the population, which constitutes the sample of our study.
For the treatment of the obtained data, quantitative statistical analysis was performed using the Microsoft Excel system.
3. Results and discussion
In this chapter, the collected data is presented, and its respective discussion is carried out based on available scientific evidence.
The first part of the questionnaire refers to the sociodemographic, academic, and professional characterization of the sample.
The age of the healthcare professionals included in the sample of this study ranges from 25 to 66 years, with an average age of 42.1 years; it can be observed that the sample is very young in age and is made up of 78% female professionals.
Regarding the professional category, 65% are nurses, 20% are doctors, 13% are operational assistants, and 2% are physiotherapists, with 46% having a bachelor's degree, 43% a master's degree, and 11% secondary education.
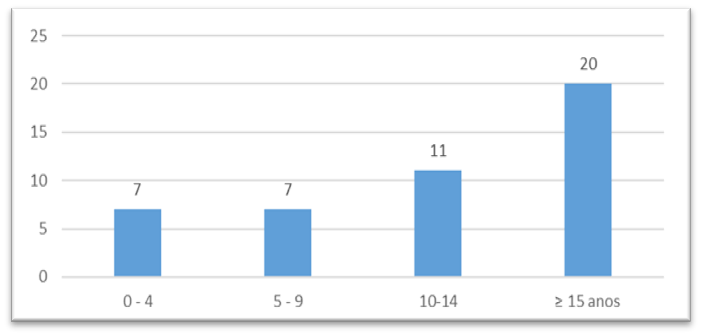
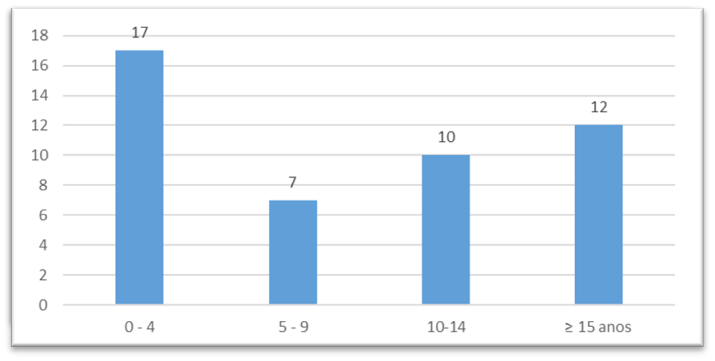
67% of professionals have more than 10 years of professional experience (Graph 1); however, 52% have been working in the ICU for less than 10 years (Graph 2). It can be concluded that, in addition to being a young team, they have professional experience. Nevertheless, 37% have been in the ICU for less than 4 years.
The second part of the questionnaire refers to understanding the relevance of the studied topic. To assess the perception of the multidisciplinary team regarding the importance of communication with critically ill patients, the following question was posed: "In your opinion, is communication a key tool in providing care to individuals in the context of ICU?" 89% stated that it is important, which aligns with a study by Yoo et al. (2020) where participants mentioned that communication, although challenging, is fundamental for safety and quality in care for critically ill patients, as advocated since 2010 by the Joint Commission. At that time, they changed their accreditation standards to include hospitals providing AAC tools to their patients with complex communication needs in a hospital setting (Lloyd et al., 2018; Encarnação et al., 2015). These standards include the requirement for trained personnel in cultural sensitivity and the use of communication tools:
Identification of patients' communication needs.
Meeting communication needs throughout the healthcare delivery process.
Provision of translation services and means.
ICU are thus encouraged to provide alternative means of communication to their patients so that they can communicate when they are unable to do so verbally (Encarnação et al., 2015).
The entire sample considers updating knowledge in the area of communication relevant, as defended by several authors who claim that training programs and communication skills training for healthcare professionals are essential (Dithole et al., 2017).
Only 37% of the sample was familiar with the AAC terminology, scientific evidence reveals that the lack of knowledge about AAC is widespread in other countries as well (Al-Yahyai et al., 2021).
The third part of the questionnaire relates to "Communication with Critically Ill Patients."
In question 1, 91.7% mentioned "difficulty in understanding the critically ill patient’s message," yet 95.6% "always try to understand what the critically ill patient wants," and 71.7% claim not to ignore the patient when they "want to communicate and are not understood." 52.1% mention that they "feel frustrated when trying to communicate with the critically ill patient.", thus 97.8% emphasize the importance of the "use of instruments/techniques that facilitate communication with the critically ill patient."
Frustration emerges as the most predominant feeling among healthcare professionals because the inability to understand the patient, coupled with the desire to provide the best care, generates a mix of emotions that are difficult to handle and result in insecurity in providing care (Handberg & Voss, 2018; Holm & Dreyer, 2018; Mortensen et al., 2019). Besides frustration, feelings of incompetence, dissatisfaction, guilt, stress, and despair are also indicated (Handberg & Voss, 2018; Happ et al., 2015a; Holm & Dreyer, 2018; Mortensen et al., 2019; Noguchi et al., 2019). The same authors reinforce that the context of providing care to critically ill patients poses a challenge for professionals and patients, as it often leads to misunderstandings, misinterpretations, and, in the worst case, disinterest in communication, causing the professional to abandon communication attempts and only focus on the physical and technical aspects of interaction.
Handberg and Voss (2018) mention that greater knowledge and use of AAC by professionals make them more competent and reduce their levels of frustration when communicating with critically ill patients.
In the question, 'Do you know some techniques to facilitate communication between you and the critically ill patient,' 83% responded affirmatively. Among the strategies mentioned were encouraging writing (providing paper and pen or a whiteboard and marker) (50%), alphabet boards (23%), picture albums (13%), and phrase tables (6%). Similar to the study by Noguchi et al. (2019), healthcare professionals were already using some AAC tools and strategies without being consciously aware of it. In the studies analyzed, the communication methods that professionals reported using were alphabet boards, picture boards, writing, gestures, pointing, and assistance in communication through family members (Happ et al., 2015b; Karlsen et al., 2018; Leung et al., 2018).
When asked about 'Which aspects do you prioritize in communicating with a patient unable to communicate verbally?' healthcare professionals referred to gestures/gestural expressions (25%), facial expressions (19%), eye contact (17%), touch (17%), smiling (12%), posture (7%), and silence (2%), which aligns with studies conducted by Al-Yahyai et al. (2021) and Handberg and Voss (2018). These studies mention that professionals primarily use communication through yes or no with gestures/gestural expressions, handshakes, or eye blinking.
The “main barriers to communication” mentioned are the patient's state of consciousness/anxiety/agitation (29%), lack of material resources to improve communication (20%), lack of training in communication/communication techniques (17%), workload overload (16%), noise (9%), lack of experience (7%), and physical space (1%). None of the professionals considered the Professional-Patient Relationship as a barrier or obstacle to communication. In this last aspect, it is evident that there is no understanding of what a Professional-Patient Relationship entails because it is only possible through effective, trustworthy communication and intentional communicative interaction with the patient aimed at helping them face their problems (Sequeira, 2016). The lack of training and experience among healthcare professionals in communication strategies with the patient becomes an obstacle to the patient's ability to communicate and interact (Handberg & Voss, 2018). Workload overload as a communication barrier was also mentioned by Noguchi et al. (2019), where professionals prioritized other activities they considered essential for life maintenance.
In the question "What are the main difficulties you face when communicating with patients with communication impairments?" the most common response was "Understanding patients who communicate through gestures, signs, or lip movements (non-verbal communication)" (31%), followed by "Understanding the patient's communication when they do not express themselves orally in a clear manner" (28%), "Doubts about the patient's perception of the received message" (27%), "Expressing oneself through non-verbal communication" (13%), and only 1% mentioned "Limited trust relationship between professional and patient". Nyhagen et al. (2023) also concluded that both healthcare professionals and patients have difficulties in agreeing on the interpretation of signs and gestures.
Yoo et al. (2020) reinforce that when communication is not effective, and the message is not adequately conveyed, some patients respond aggressively, making treatment and mechanical ventilation more difficult, thus prolonging the length of hospitalization.
A study that observed the interaction between healthcare professionals and critically ill patients on mechanical ventilation revealed that when professionals began using AAC with patients, they were able to better understand them and respond more appropriately to their needs in a timely manner. This change resulted in a decrease in negative feelings associated with communication for both healthcare professionals and patients and increased patient satisfaction levels (Noguchi et al., 2019).
Conclusion
Communication is a right for all individuals, even for those who suffer from speech impairments. Ineffective communication leads to treatments, recovery, and patient rehabilitation that are not tailored to their needs. Therefore, it becomes pertinent to implement AAC tools and strategies. Their consistent implementation and standardization in the ICU increase the safety and quality of care provided, making patients feel more confident and cooperative, thus overcoming existing communication barriers.
Healthcare professionals have gaps in knowledge regarding communication with critically ill patients. However, according to the literature, training actions on AAC are confirmed as an important learning strategy in knowledge transmission, which could contribute to reducing these knowledge gaps. The acquisition of communication boards, writing boards, AAC applications for tablets also proves to be fundamental resources to foster communication with critically ill patients. In the future, training actions should be carried out, and a communication protocol with critically ill patients should be implemented.
Therefore, the development of communication skills should be a priority for healthcare professionals because it is in communication that the essence of humanized care lies.
Author contributions
Conceptualization, A.C., D.S. and M.S.; data curation, A.C., D.S. and M.S.; formal analysis, A.C., D.S. and M.S.; investigation, A.C., D.S. and M.S.; methodology, A.C., D.S. and M.S.; project administration, A.C., D.S. and M.S.; resources, A.C., D.S. and M.S.; software, A.C., D.S. and M.S.; supervision, A.C., D.S. and M.S.; validation, A.C., D.S. and M.S.; visualization, A.C., D.S. and M.S.; writing-original draft, A.C., D.S. and M.S.; writing-review and editing, A.C., D.S. and M.S.