Introduction
The International Council of Nurses, through the International Classification of Nursing Practice, defines the concept of sleep as a bodily process, which refers to the "recurrent decrease in bodily activity, marked by reduced consciousness, not being awake, accompanied by inattention, with decreased metabolism, immobile posture, decreased physical activity and decreased sensitivity to external stimuli, but readily reversible" (Classificação Internacional para a Prática de Enfermagem, 2019).
Sleep is a basic physiological function, and well-being and quality of life depend on the quantity and quality of sleep (Mercadante et al., 2017). The onset and maintenance of the sleep process depends essentially on the suppression of activity in the ascending conduction systems, a process that is realised through the inhibition of neurons in the preoptic area, located in the lateral region of the cerebral ventricles. It is characterised by a period in which there is a loss of consciousness and, generally, a frank decrease or absence of bodily activity, in which the person remains with their eyes closed. Sleep, from its beginning to its end, is not a homogeneous process and essentially consists of two phases: the rapid eye movement (REM) phase, which is associated with active dreams, and the non-rapid eye movement (NREM) phase, where there is a significant reduction in skeletal muscle tone, which progresses to partial or complete atonia. Generally, the sleep sequence is cyclical, with periods of REM and NREM sleep alternating every 60 to 90 minutes (Carley & Farabi, 2016).
Among the many existing sleep disorders, the most prevalent in palliative care (PC) are insomnia and hypersomnia (Monteiro et al., 2017).
Insomnia is a heterogeneous complaint that can involve difficulty falling asleep (initial insomnia), difficulty maintaining the sleep cycle, characterised by frequent nocturnal awakenings (intermediate insomnia), inability to resume sleep after awakenings at the end of the night (terminal insomnia) or complaints that the sleep period was not restorative (Savard & Morin, 2001).
On the other hand, hypersomnia refers to the complaint of excessive and disabling daytime sleepiness. In this situation, patients find it difficult to remain alert during the main waking hours of the day, falling asleep unintentionally and at inappropriate times that interfere with their daily routine (Karna & Gupta, 2021).
Sleep disorders are a challenge in the context of PC, not only for the patients themselves but also for their families. Disturbances in this spectrum add a load of stress to the worries already inherent in managing an advanced, incurable and progressive disease. In palliative care patients, daytime activity is usually reduced, leading to a lack of definition in the sleep-wake cycle, especially when the daily routine involves long periods confined to bed. Mental agitation and restlessness at night can result in long periods without rest, which contribute to the development of problems related to the sleep cycle (Hajjar, 2008). In this context, insomnia is generally assumed to be an effect of other comorbidities, associated with depressive or anxiety disorders, assuming that it will be resolved with the treatment of these conditions. However, this assumption is erroneous and the lack of treatment for sleep-related disorders can contribute to an increase in the stress burden, which in turn can lead to the actual worsening of symptoms associated with these conditions (Mercadante et al., 2015).
Sleep patterns can be improved through the implementation of pharmacological and non-pharmacological interventions. However, the current existence of a wide range of targeted pharmacological therapies and their ease of application tends to neglect the implementation of non-pharmacological therapies.
As non-pharmacological interventions to promote the quality of sleep patterns, the evidence points to the possibility of teaching, instructing and applying the basic principles of sleep hygiene to patients with palliative needs, at the beginning of their illness course. On the other hand, cognitive and behavioural interventions have shown great promise in improving symptoms related to these disorders (Hajjar, 2008).
Considering the above, this Scoping Review aims to map and synthesise the evidence of autonomous nursing interventions to improve the quality of sleep patterns in patients undergoing PC, gathering information on existing interventions. The aim is to answer the following research question: Are there autonomous nursing interventions to improve the quality of sleep patterns in patients undergoing PC?
1. Methods
Generally, a scoping review is conducted with the aim of exploring or deepening the literature, mapping and summarising the existing evidence on a particular subject and identifying gaps in knowledge (Peters et al., 2020). A rigorous methodological protocol must be adopted to fulfil this objective (Peters et al., 2020).
The methodological framework of Arksey et al. (2005) recommends five stages for carrying out a scoping review, namely identifying a research question; identifying relevant studies in the research area; selecting the studies to be included; mapping the data collected and, finally, collecting, synthesising and presenting the results.
Since the aim of this methodology is not to find the best scientific evidence, but rather to map and synthesise existing scientific evidence, it does not aim to analyse the methodological limitations or risk of bias in the evidence of the included studies (Peters et al., 2020).
Its systematisation is based on the Joanna Briggs Institute framework, which uses the PCC mnemonic (population, concept, context) of the study to be carried out (Peters et al., 2020).
In this study, the population analysed is adult patients with alterations in the quality of their sleep pattern. The concept being analysed focuses on autonomous nursing interventions to improve the quality of sleep patterns in the context of CP. No distinction was made between patients who were hospitalised and those who remained at home.
Using PCC, it was possible to develop the research question: "Are there autonomous nursing interventions to improve the quality of the sleep pattern of patients undergoing PC?".
A clear research question should contain the elements identified in the PCC, which will influence the creation of specific inclusion criteria that facilitate the research process and provide a starting point for the development of the scoping review (Peters et al., 2020). In accordance with the question developed for the present research, this review included studies involving an adult population aged over 18 in need of PC and studies describing non-pharmacological interventions aimed at improving the quality of sleep patterns in patients with sleep disorders. We chose to include only primary studies (qualitative, quantitative or mixed). All studies involving paediatric and neonatal populations and interventions involving the administration of any type of drug aimed at improving the quality of patients' sleep patterns were excluded.
Search Strategy
The search strategy used began with a generic search in electronic databases, with words related to the topic identified and subsequent reading of the text of the titles and abstracts and the index terms used to describe the scientific studies found. The aim of the initial search was to identify possible search terms for the present investigation; once these had been identified, the scientific descriptors in the health library, MeSH Browser and CINAHL headings were identified, as well as a free term (Table 1); the search was conducted in two databases available on EBSCOhost (ESEP): CINAHL Complete and MEDLINE Complete, using the following Boolean phrases respectively: ("sleep*")AND("nursing intervention*")AND("palliative care") and ("sleep*")AND("nurs*")AND("palliative care")AND("intervention*").
To be included in this review, we considered studies published in the aforementioned databases until 27 April 2022 and which were available in Portuguese, English or Spanish, published in academic journals and subject to peer review. Grey literature was not considered in this review, which could be considered a limitation of the study.
Table 1 Search Terms
| DeCs | Mesh | Cinahl Headings | Free Terms |
| Sleep | Sleep | Sleep | Intervention |
| Nurse | Nurse | Nurse | |
| Palliative Care | Palliative Care | Palliative Care | |
| Nursing Interventions |
Initially, the relevance of the articles selected for this review was analysed by two independent reviewers (DS, AC), based on the information provided in the title and abstract of the studies.
In a second phase, the full text of all the studies that met the inclusion criteria explained above was analysed, also by two independent reviewers (AS, AC).
Data extraction
Data on the selected studies was extracted by two independent reviewers (DS, AS), based on a table developed by the researchers, which includes the name(s) of the author(s), date and place of publication of the study, participants and objective of the study, study design, interventions and results. Doubts and disagreements between the two reviewers involved in each stage were resolved using the third reviewer not involved.
2. Results
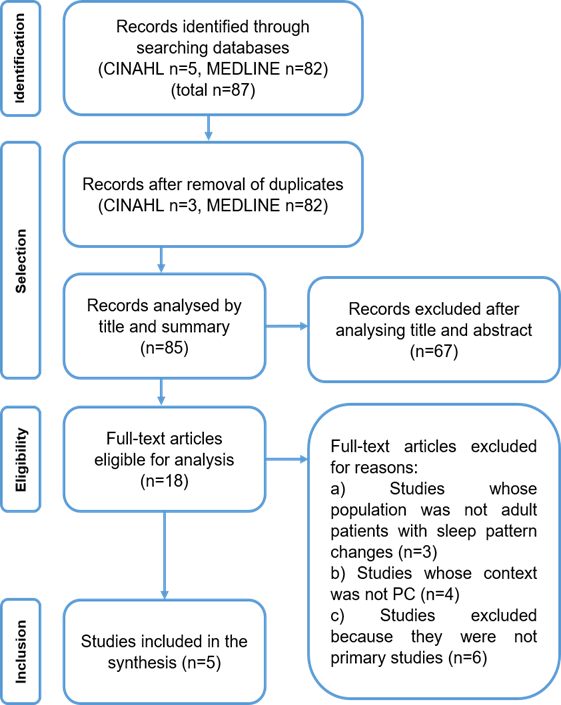
The results obtained after the screening process described above are presented according to the PRISMA Extension for Scoping Reviews. The flowchart shown in Figure 1 is intended to graphically represent the number of studies identified, included and excluded, as well as the reasons for exclusions (Tricco et al., 2018).
The search identified 87 studies from the aforementioned databases. After removing duplicates, a total of 85 studies were identified. Of this number, after reading the title and abstract of the studies, 67 were excluded. Of the remaining 18 studies, after reading the full text, 13 could be excluded as they did not meet the predefined inclusion criteria, ending up with a total of five studies included in this review.
The five eligible studies were fully analysed and the data that answers the research question and objective of this scoping review was extracted and synthesised from them. The following table (Table 2) summarises the data resulting from the analysis of the studies, in terms of authors, year and country of origin, study objective, method, participants, interventions and results.
Table 2 Answers to the review question presented by the study
| Author(s), date and country of origin | Participants | Objective | Study design | Interventions / Instruments | Results |
|---|---|---|---|---|---|
| Sela et al. 2005 Canada | 100 outpatient cancer patients receiving PC | To describe patterns of sleep disturbances, treatments and communication with health professionals in outpatients undergoing PC. | Descriptive correlational study | Completion of a retrospective questionnaire to collect information on sleep habits, concerns, sleep improvement strategies and communication with health professionals. | Sleep disorders are highly common among cancer patients in PC. 11% reported using at least one of the following non-pharmacological strategies: relaxation, visualisation and prayer. 9% said they used tea/milk, 7% said they watched TV or listened to the radio to induce sleep, 6% took a hot bath, 4% said changing position was an effective technique, 2% said exercise; reading was rated as the most effective strategy, but was used infrequently (2%). |
| Plaskota et al. 2012 United Kingdom | 11 hospice patients | To evaluate the benefits of hypnotherapy in the management of anxiety, depression and sleep disorders. | Observational study | Four hypnotherapy sessions; Completion of the following questionnaires: Hospital Anxiety and Depression Scale (HADS), Edmonton Symptom Assessment System (ESAS), and Verran and Snyder-Halpern Scale (VHS) at the beginning of the study, after the second session and after the fourth hypnotherapy session; assessment of sleep quality through actigraphy. | After the fourth hypnotherapy session, there was a significant improvement in sleep quality. Hypnotherapy can improve anxiety-related symptoms in patients receiving PC, which in turn has the benefit of improving their sleep pattern. |
| Bernatchez et al. 2018 Canada | Six patients diagnosed with cancer, receiving PC, living at home | To validate the reliability and accessibility of the Cognitive-Behavioural and Environmental Intervention (CBT-E) to improve insomnia and hypersomnia . | Observational study | Implementation of CBT-E: pre-treatment phase to collect data about the participants, deliver documents and devices needed to take part in the study; intervention phase, which consisted of administering individual CBT-E sessions; post-treatment phase, which consisted of collecting the sleep diaries and devices provided and distributing satisfaction questionnaires to the participants. | Behavioural strategies, including the control of external stimuli, were described by the participants as the most useful; CBT-E proved more useful in improving insomnia as the only symptom present, than in treating hypersomnia or when these were concurrently present. |
| Yildirim et al. 2020 Turkey | 68 patients hospitalised in a PC unit (34 in the experimental group and 34 in the control group) | To determine the effect of lavender oil on sleep quality and vital signs in patients undergoing PC. | Randomised controlled clinical trial | Experimental group - taking 10 deep breaths through a bowl with 3 ml of 100% pure lavender oil before going to bed at 10pm. The lavender solution was placed 1 metre away from the patients between 10pm and 6am. Vital signs were monitored at 4-hour intervals throughout the night, and sleep quality was assessed at 6am using the Richards-Campbell Sleep Questionnaire. | The frequency of awakenings decreased in the experimental group on the first day of the intervention compared to the control group. On the second day, it was observed that the experimental group slept more deeply, fell asleep more easily, the frequency of nocturnal awakenings decreased, the ability to fall asleep again after being woken up improved and the quality of sleep also improved, when compared to the control group. The use of lavender oil is an effective method for improving the overall quality of sleep in PC patients. |
| Aslan & Çetinkaya 2021 Turkey | 73 hospitalised patients (36 in the experimental group and 37 in the control group) | To investigate the effect of therapeutic touch on spiritual care and sleep quality in patients undergoing PC. | Randomised controlled trial | Application of therapeutic touch for 15 minutes, placing the patient's hand between the researcher's hands, making rhythmic and gentle movements on the patient's hand. Applied three times a week for a month, between 6pm and 9pm, in order to facilitate the process of falling asleep. Questionnaires were completed before the intervention and four weeks afterwards to assess its effectiveness. | Therapeutic touch had a positive effect on patients' sleep quality. Therapeutic touch can be described as a non-invasive intervention used to improve sleep quality, and nurses can play a crucial role in developing and implementing it for patients undergoing PC. |
3. Discussion
This scoping review aims to map and synthesise the available scientific evidence on autonomous nursing interventions to improve the quality of sleep patterns in patients undergoing PC. To achieve the proposed objective, five primary studies were included, with publication dates of 2005, 2012, 2018, 2020 and 2021, which allowed us to infer that the topic has been emphasised over the years. The articles selected are representative of a total of 258 patients who received PC from three different continents (Europe, America and Asia). This reinforces the relevance of this topic and its transversality to different cultures and societies. One study reports on the reality experienced in the United Kingdom, two studies were carried out in Turkey and two in Canada.
All the studies adopted a quantitative approach. In the case of the participants in this review, in two studies they were at home and were cancer patients (Sela et al., 2005; Bernatchez et al., 2018). In the other three studies, they were hospitalised (Plaskota et al., 2012; Yildirim et al., 2020; Aslan & Çetinkaya, 2021).
With regard to sample size, two studies had a sample of less than 15 participants and the remaining studies had a sample of between 60 and 100 participants.
In relation to the objective of the studies in the sample, it should be noted that Sela et al. (2005) sought to describe patterns of sleep disorders and possible treatments, while the remaining studies sought to determine the effect of a specific non-pharmacological intervention in the treatment of sleep disorders. The non-pharmacological interventions addressed are cognitive-behavioural and environmental intervention (Bernatchez et al., 2018), hypnotherapy (Plaskota et al., 2012), the use of lavender oil (Yildirim et al., 2020) and therapeutic touch (Aslan & Çetinkaya, 2021).
Non-pharmacological interventions are non-invasive, science-based interventions aimed at preventing, treating or curing a health problem (Plateforme CEPS, 2017). They take the form of a product, a method, a programme or a service whose content must be known by the user. They are linked to identified biological mechanisms and/or psychological processes and are the subject of efficacy studies. They have an observable impact on health, quality of life, behavioural and socio-economic indicators. Their implementation requires relational, communicational and ethical skills (Plateforme CEPS, 2017).
The results of the study by Sela et al. (2005) show that sleep disorders are highly frequent in cancer patients undergoing PC. Yildirim et al. (2020) corroborate this statement, adding that the quality of life of PC patients suffering from sleep disorders is compromised.
In their study, Sela et al. (2005) reported that 53% of patients identified strategies they had tried to solve sleep problems and 44% reported using more than one sleep induction/maintenance technique. The most commonly reported non-pharmacological strategies were relaxation, visualisation and prayer.
Furthermore, Sela et al. (2005) agree that, according to the effectiveness attributed to non-pharmacological interventions, patients should be encouraged to put them into practice, referring to them as adjuncts to pharmacological therapies. The authors refer specifically to relaxation techniques, visualisation, changing positions and reading.
Through their study, Plaskota et al. (2012) prove that hypnotherapy can improve sleep in palliative patients. However, the results are controversial, as they are validated by the VSH sleep scale, but not by actigraphy. It should also be noted that the results were only perceived by the patients after the fourth hypnotherapy session.
The study by Bernatchez et al. (2018) concludes that behavioural strategies, including the control of external stimuli, are very useful from the participants' perspective. These strategies require participants to be as active as possible during the day, carrying out activities that take into account their limitations, such as cooking or writing in a diary.
Monteiro et al. (2017) highlight psychological and behavioural therapies as a non-pharmacological treatment for sleep disorders, along with sleep hygiene and the correction of reversible factors.
The CBT-E (Cognitive-Behavioural and Environmental Intervention) used by Bernatchez et al. (2018) proved to be more useful for improving insomnia as the only symptom present, rather than treating hypersomnia or when these were present concomitantly. However, the authors suggest that when both insomnia and hypersomnia are present, improving one of these conditions can cause the other to worsen.
Yildirim et al. (2020) agree that the use of lavender oil is an effective method for improving the overall quality of sleep in PC patients, as they found several gains when comparing the experimental group with the control group, namely the frequency of awakening, greater ease of falling asleep, deeper and better quality sleep, fewer nocturnal awakenings and better ability to fall asleep again afterwards.
The study by Aslan and Çetinkaya (2021) emphasises therapeutic touch, stating that it has a positive effect on patients' sleep quality. It is described as a non-invasive intervention used to improve sleep quality, and nurses can play a crucial role in its development and implementation.
Although the aforementioned studies show that there are several non-pharmacological strategies that can help improve the sleep pattern of patients undergoing PC, Sela et al. (2005) conclude that this symptom is neglected by the patients themselves, who tend not to report it; for this reason, the authors recommend that patients should be frequently questioned about the quality of their sleep.
It is therefore crucial for nurses to be able to intervene in this area, collecting data on the patient's sleep pattern, so that they can make decisions within the scope of autonomous nursing interventions, based on the most up-to-date evidence. Article 9(2) of the Nursing Professional Practice Regulations (Decreto-Lei - Decree-Law 161/96, p. 2961) states that "autonomous actions are those carried out by nurses, under their sole and exclusive initiative and responsibility, in accordance with their professional qualifications, whether in the provision of care, management, teaching, training or counselling, with contributions to nursing research". This includes non-pharmacological interventions, which can play a major role in improving the quality of sleep of patients undergoing PC.
3.1 Limitations of the studies
The fact that this scoping review is based on information gathered from only five studies may be a limitation, since it totals an analysed population that can be considered not very significant in quantitative terms.
As already mentioned, it is also worth considering the fact that two of the studies were carried out with patients receiving PC at home (Sela et al., 2005; Bernatchez et al., 2018) and the remaining three with inpatients (Plaskota et al., 2012; Yildirim et al., 2020; Aslan & Çetinkaya, 2021), which immediately has an influence on the external factors experienced. In addition, two of the studies only reported on cancer patients (Sela et al., 2005; Bernatchez et al., 2018) and one of the studies included patients diagnosed with anxiety disorders (Plaskota et al., 2012). Two studies had small sample sizes as a limiting factor, namely the study by Bernatchez et al. (2018) with only six patients and the study by Plaskota et al. (2012) with 11 patients.
The fact that all the studies that make up the corpus of analysis in this review were conducted in care contexts other than Portugal does not allow us to draw direct conclusions that can be applied to the population we work with on a daily basis, which is a clear restriction on the conclusions and implications for direct clinical practice that may arise from this scoping review.
3.2 Limitations of the scoping review
In this scoping review, we included studies published in English, Portuguese and Spanish. It could therefore be hypothesised that articles published in other languages were important for this review. The fact that only two databases were used for the search may also be a limitation.
Given that the development of scoping reviews does not recommend assessing the methodological quality of the studies included, this review does not present implications for clinical practice, which is also a limitation.
Conclusion
Most of the authors of the studies analysed support sleep disorders as a problem that should be seriously considered in the context of PC.
In response to the aim of this review, it can be concluded that all the studies analysed identify non-pharmacological strategies that can be autonomous nursing interventions and that aim to improve the quality of the sleep pattern of patients undergoing PC.
Although the strategies applied were different, all the authors demonstrated an effective improvement in the quality of the participants' sleep patterns after implementing them.
This review made it possible to realise that the subject is relatively recent and has been highlighted in recent years.
Implications for research
The mapping carried out can be used as a basis for planning and developing interventions aimed at improving the sleep pattern and quality of patients requiring PC. However, further quantitative and qualitative studies on the factors that promote and inhibit sleep quality need to be carried out in order to target the interventions to be applied. The mapping also made it possible to identify the need for a systematic literature review in order to verify the best scientific evidence, since the methodology recommended for this scoping review does not include an analysis of the methodological quality of the studies included.
The previous research carried out for this study revealed that there is no available evidence on the subject in the Portuguese context, and that there are no defined standards for the implementation of non-pharmacological interventions aimed at improving sleep quality in palliative care patients. This fact makes it difficult to apply the results of this study to the Portuguese population as a whole, so there is an even greater need for research in this area in the Portuguese context.
Thus, as suggested by Aslan and Çetinkaya (2021), we are pleased to agree that nurses can play a vital role in the development and implementation of programs aimed at improving the quality of sleep of patients undergoing PC, contributing to the improvement of quality of life at this stage. In this sense, it is important for nurses to regularly monitor sleep quality in order to carry out appropriate and timely interventions.
Author contributions
Conceptualization, D.S., A.C. and A.S.; data curation, D.S., A.C. and A.S.; formal analysis, D.S., A.C. and A.S.; investigation, D.S., A.C. and A.S.; methodology, D.S., A.C. and A.S.; project administration, D.S., A.C. and A.S.; resources, D.S., A.C. and A.S.; software, .S., A.C. and A.S.; supervision, D.S., A.C. and A.S.; validation, D.S., A.C. and A.S.; visualization, D.S., A.C. and A.S.; writing-original draft, D.S., A.C. and A.S.; writing-review and editing, D.S., A.C. and A.S.