Introduction
The impact of practice environments on nurses has been widely studied and is a key factor in predicting outcomes such as job satisfaction, retention, and nurse engagement (Wei et al., 2018).
The current shortage of nursing professionals has brought increased attention to strategies aimed at recruiting and retaining staff nurses. However, the need to recruit and retain nurse managers has received much less attention (Laschinger et al., 2006).
Nurse managers play a crucial role in the healthcare system, serving as leaders in promoting quality care and fostering a positive work environment for nurses (Acob & Martiningsih, 2018).
In the current landscape where value-based healthcare is a central focus, nurse managers are entrusted with key responsibilities, including delivering high-quality, safe, effective, equitable, and efficient care; meeting the expectations of patients and their families; ensuring continuity of care; and contributing to cost reduction (Hughes et al., 2022). A positive practice environment for nurse managers can foster work engagement and enhance leadership, which, in turn, contributes to the development of a supportive environment for the nursing staff (Warshawsky et al., 2022). Nurse managers play a crucial role in the healthcare system, serving as leaders in promoting quality care (Acob & Martiningsih, 2018). However, many plan to leave their management positions within five years (Warden et al., 2021). This challenge is further exacerbated by high exposure to stressful situations, driven by factors such as excessive workloads, increased responsibilities, and limited resources (Penconek et al., 2024).
The purpose of this scoping review is to map the scientific evidence on the nurse manager’s practice environment in acute healthcare settings. Nurse managers are vital in healthcare systems, influencing staff retention, patient outcomes, and organizational efficiency. Much of the existing literature focuses on the work environment of staff nurses, with less attention given to nurse managers' unique challenges and needs.
A scoping review is particularly well-suited for this topic, providing a comprehensive overview of the available research.
1. Methods
The present review followed the methodology defined by the Joanna Briggs Institute (JBI) for scoping reviews. The Preferred Reporting Items for Systematic reviews and Meta-Analysis extension for Scoping Reviews (PRISMA-ScR) guideline (Tricco et al., 2018) will be used to structure the review report. The research question that guided this review was: "What is known about the practice environment of nurse managers in hospital settings?" According to JBI, a scoping analysis aims to map the existing evidence on a given topic, identify key issues, and support knowledge development (Aromataris et al., 2024).
Eligibility criteria
An inclusive approach was adopted for this review, encompassing all relevant types of available literature. This included both primary research studies presenting original data and systematic reviews offering comprehensive syntheses of existing evidence. The following inclusion criteria were defined: studies in Portuguese, English, or Spanish, with abstracts or full texts available. Given the scarcity of studies in this field, no time limit was set to ensure a more comprehensive review.
Sources, Information, and Search Strategies
To ensure the relevant selection of the literature and formulate the eligibility criteria, the review question was formulated based on the PCC strategy, which considered the following: population (P), nurse manager; concept (C), practice environment; and context (C), hospital (Table 1)
Table 1 Inclusion and exclusion criteria
| PCC Framework | Inclusion | Exclusion |
| P - Population | Nurse managers working in hospital settings (including unit managers and ward managers) | Directors of nursing chief, nursing Officer (CNO) or Nurse Executive. |
| C - Concept | The nurse manager practice environment refers to the conditions and factors that influence the work setting and effectiveness of nurse managers. This review will include the studies that explore how nurse managers evaluate their practice environment and the relation between nurse managers' practice environment and nurses' outcomes (engagement, professional satisfaction, burnout, and intent to leave) | Studies analyzing the relationship between the NMPE and patient outcomes and organizational outcomes will be excluded. |
| C - Context | Studies developed in hospital settings: acute care hospitals; specialized hospitals (e.g., paediatric, oncology, psychiatric hospitals); academic or teaching hospitals; rural and urban hospital environments | Studies that evaluate the nurse manager practice environment in rehabilitation centres, primary health facilities, nursing homes, or long-term care facility |
The research question that guided this review was "What is known about the practice environment of nurse managers in hospital settings?". The search strategy followed a three-stage approach to identify published and unpublished sources comprehensively.
The process began with an initial limited search in MEDLINE/PubMed and CINAHL (EBSCOhost) using key terms such as nurse manager and practice/work environment to explore existing literature on the topic.
Next, a comprehensive analysis of Health Sciences Descriptors (DeCS) and Medical Subject Headings (MeSH) was performed to improve the precision and scope of the search. The complete search was carried out using the following databases: CINAHL Complete, PubMed, and Web of Science. Unpublished sources/gray literature were searched in ProQuest Dissertations & Theses Index via Web of Science and Scientific Open Access Scientific Repositories of Portugal (RCAAP) via EBSCO Discovery Service. Finally, a snowball search strategy was employed, in which bibliographic references from all included articles were systematically reviewed to identify additional relevant studies
Table 2 presents a detailed breakdown of the search strategies used for each database. All database searches were conducted on December 23, 2024, maintaining the integrity of the review process.
Table 2 Search strategies used in each database
| Database/Results | Search Terms Used |
| CINAHL Complete (1211) | (TI (“Nurse manager*” OR “nurse leader*” OR “head nurs*” OR “Nurse Administrator*”) OR MH (Nurse managers+ OR Nurse Administrators)) AND (TI (“Practice environment*” OR “work environment*”) OR MH Work Environment) |
| PubMed (135) | (("Nurse manager*"[Title] OR "nurse leader*"[Title] OR "head nurs*"[Title] OR "Nurse Administrator*"[Title]) OR (Nurse Administrators [MeSH Terms])) AND (("Practice environment*"[Title] OR "work environment*"[Title]) OR (Working Conditions [Mesh:NoExp])) |
| Web of Science (2302) | “Nurse manager*” OR “nurse leader*” OR “head nurs*” OR “Nurse Administrator*” (Title) or “Nurse manager*” OR “nurse leader*” OR “head nurs*” OR “Nurse Administrator*” AND “Practice environment*” OR “work environment*” (Title) or “Practice environment*” OR “work environment*” |
| ProQuest Dissertations & Theses Index via Web of Science (18) | “Nurse manager*” OR “nurse leader*” OR “head nurs*” OR “Nurse Administrator*” (Title) AND “Practice environment*” OR “work environment*” (Title) |
| RCAAP via EBSCO Discovery Service (1) | TI (“Nurse manager*” OR “nurse leader*” OR “head nurs*” OR “Nurse Administrator*” OR "enfermeiro* gestor*" OR "enfermeiro* chefe*") AND TI (“Practice environment*” OR “work environment*” OR "ambiente de prática") |
Study Selection
The retrieved records were imported into Rayyan (Qatar Computing Research Institute, Doha, Qatar), which facilitated the removal of duplicates, organization, archiving, and study selection. Two researchers independently carried out the selection process, and no discrepancies arose that necessitated the intervention of a third reviewer.
Selection Process
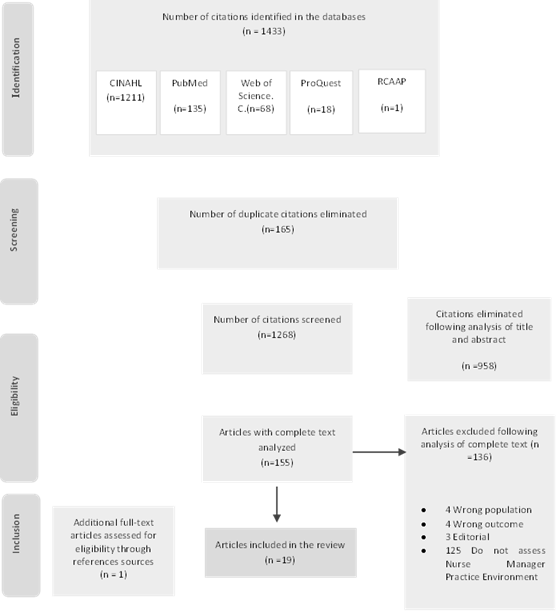
The final review thoroughly documented the results of the bibliographic search and study selection process using a PRISMA flowchart.
Data Collection Process
In accordance with the JBI scoping review methodology, data from the included articles were systematically extracted into a structured table. This table captured key information, including Author(s), Year of Publication, Country, methodological approach, purpose, sample size, and conclusions.
2. Results
Figure 1 presents the results of the analysis steps using the PRISMA flowchart model. A total of 1433 articles were initially retrieved from the selected databases. After removing 165 duplicates, 1268 articles remained for screening. A title and abstract screening was conducted, excluding 1113 articles without relevant search terms, leaving 155 articles for full-text analysis. Following a thorough full-text review, 19 articles met the inclusion criteria. One additional study was identified by analysing the selected articles' bibliographic references.
The articles included in this scoping review encompass the responses of 2072 nurse managers working in hospital settings. Most of these studies originate from the USA (74%), followed by Turkey (11%), Finland, China, and Brazil, with one study each. Quantitative methodology was the most frequent (68%). Four studies used a qualitative approach; one mixed-method study and an integrative literature review were also included. Two studies were doctoral theses.
Through the analysis of the nineteen included articles, six thematic categories emerged: instruments for evaluating the nurse manager's practice environment, how nurse managers assess their practice environment, factors influencing the practice environment for nurse managers, a comparison of the practice environments of nurse managers and direct care nurses, the impact of the nurse manager's practice environment on their outcomes, and the effect of the nurse manager's practice environment on the outcomes of direct care nurses.
Table 3 presents the detailed characteristics of the analysed studies.
Table 3 Characteristics of the reviewed studies
| Authors | Year | Country | Methodology | Purpose | Sample Size (NMs) | Conclusion |
| Aslan et al. | 2022 | Turkey | Quantitative | Explore the organizational silence behaviors of nurse managers, assess their practice environment, and analyze the influence of occupational and demographic variables on organizational silence. | 169 | Nurse Managers experience discomfort in openly expressing their opinions in practice environments where they and their staff feel unsupported. A positive work environment and the ability to voice opinions freely contribute to reducing organizational silence among Nurse Managers. |
| Chen, He & Liu | 2024 | China | Quantitative | Investigate the current status of the practice environment and its associated factors among nurse managers in China and to find the aspects that need to be improved the most. | 405 | Nurse manager practice environment in China has improved, reflecting a relatively high overall score. However, key challenges remain, including insufficient budgeted resources, an unbalanced workload, and strained nurse manager-physician relationships. |
| Gormley. | 2011 | USA | Quantitative | Examine differences in perceptions of work environment and quality of care between nurse managers and staff nurses, and the relationship between nurses perceptions of the work environment and intention to leave. | 40 | The study highlights a disparity in work environment perceptions, with nurse managers viewing it more favorably than staff nurses. This disconnect may impact retention, as factors like participative governance, job satisfaction, and perceived quality of care influence nurses' decisions to stay or leave. |
| Grandfield et al. | 2022 | USA | Quantitative | Evaluate how nurse manager job design factors and their experience relate to their practice environment and the direct and indirect effects on nurse and patient outcomes. | 541 | Overly wide spans of control among nurse managers negatively affect their work environment, staff retention, and patient outcomes. Fostering a positive practice environment for nurse managers is key to retaining both leadership and frontline nursing staff, ensuring sustainable, high-quality patient care. |
| Grubaugh | 2019 | USA | Quantitative | Examine the relationship between personal/positional demographics and the Nurse Manager Practice Environment (NMPE) and the relationship between NMPE and nurse manager (NM) outcomes. It also examines the mediating effect of work-family conflict (WFC), a measure of work-family balance (WFB) on the relationship between NMPE and NM outcomes. | 194 | The Nurse Manager Practice Environment significantly impacts job satisfaction, career recommendation, and turnover intentions. Enhancing the nurse manager practice environment can improve nurse manager retention, highlighting its importance for nursing policy and practice. |
| Huddleston & Gray | 2016 | USA | Quantitative | Assess the psychometric properties of the American Association of Critical-Care Nurses (AACN) Healthy Work Environment Assessment Tool (HWEAT) and to measure the nurse leaders’ and direct care nurses’ perceptions of a healthy work environment in na acute care setting. | 28 | Nurse leaders identified authentic leadership as the strongest aspect of their work environment, emphasizing the importance of genuine and effective leadership. However, they viewed appropriate staffing as the most challenging factor, recognizing its impact on both nurse well-being and patient care. Similarly, direct care nurses highlighted effective decision-making as a key strength but also cited staffing as a significant concern. |
| Huddleston & Gray | 2016 | USA | Qualitative | The purposes of these two qualitative research studies are to explore the nurse leaders’ and direct care nurses’ perceptions of the meaning of a HWE, to describe the nurse leaders’ and direct care nurses’ perceptions of a HWE, and to define the characteristics of a HWE in acute care settings. | 72 | A healthy work environment includes appropriate staffing, authentic leadership, effective decision-making, meaningful recognition, skilled communication, true collaboration, genuine teamwork, and both physical and psychological safety. |
| Huddleston, Mancini & Gray | 2017 | USA | Quantitative | Develop items on the healthy work environment (HWE) for nurse leaders and direct care nurses, to assess the validity and reliability of these new tools, and to describe the nurse leaders and direct acre nurses perceptions of a healthy work environment (HWE) using nonexperimental descriptive designs. | 341 | Nurse leaders established the importance of appropriate staffing, meaningful recognition, and skilled communication as parts of an HWE as identified as separate components on the tool. Direct care nurses established the importance of genuine teamwork and physical and psychological safety as parts of a HWE as identified as separate components on the tool. |
| Jäppinen et al. | 2022 | Finland | Quantitative | Examine nurse managers’ stress from workload and its associations to overall job stress, job satisfaction and practice environment. | 209 | One in five nurse managers faces high stress due to workload. Reducing stress through well-being initiatives, work-life balance, and self-management training can improve job satisfaction and retention. |
| Keith et al. | 2020 | USA | Integrated literature review | Understand factors that influence nurse manager job satisfaction. | na | Nurse manager job satisfaction depends on workload, organizational support, supervisor relationships, and training quality. Addressing these issues can improve retention by fostering a supportive practice environment with growth opportunities. |
| Montgomery and Patrician | 2022 | USA | Quantitative | Investigate the work environment, resilience, burnout, and turnover intention and examine how work environment and personal resilience impact burnout and turnover intention among nurse leaders in the midst of the COVID-19 crisis. | 56 | Findings show a strong negative relationship between resilience and burnout, indicating that more resilient nurse leaders experience less burnout. A supportive environment and resilience play key roles in retention, particularly during high-stress periods like the COVID-19 pandemic. |
| Ogashi | 2019 | USA | Qualitative | Explore nurse managers' perceptions of their work environments, including their views on how these environments influence staff nurse outcomes and impact patient outcomes | 17 | Nurse managers experience significant stress from high-acuity care, staffing challenges, and heavy workloads. While financial incentives help, the key motivator is seeing staff engagement and happiness. However, high patient-to-nurse ratios cause dissatisfaction. |
| Raso et al. | 2022 | USA | Quantitative | Determine the perceptions of clinical nurses and nurse leaders about authentic nurse leadership, work environment, pandemic impact, well-being and intent to leave their position and profession during the second year of the pandemic. | 300 | Nurse managers view their practice environment more positively than direct care nurses, but both groups cite "appropriate staffing" as the key challenge. The findings highlight the need for leadership interventions to improve staffing, work conditions, and nurse well-being. |
| Santos et al. | 2017 | Brazil | Mixed-methods | Compare the working environment of nurse managers and nursing assistants within the hospital context. | Quantitative: 12; Qualitative: 8 | Both nursing assistants and nurse managers view their work environments favorably. Strong collaboration was observed, consistent with previous Brazilian studies emphasizing teamwork as essential for nurse managers. Both quantitative and qualitative findings aligned on environmental control, physician relationships, and organizational support. However, despite autonomy scoring highest in the B-NWI-R subscales, many nurses felt their professional autonomy remained limited within the institution. |
| Shirey, | 2009 | USA | Qualitative | Showcase the relationship among authentic leadership, organizational culture, and healthy work environments using a stress and coping lens. | 21 | Findings suggest that organizational culture and leadership matter and that to create and sustain healthy work environments for practice, a positive organizational culture provides the desirable and catalytic milieu. |
| Tosun, & Yildirim | 2021 | Turkey | Quantitative | Determine the nurse managers’ opinions about their practice environments. | 211 | Nurse managers generally rated their practice environments positively. Unmarried nurse managers and those with over 11 years of experience reported more favorable perceptions, particularly in patient safety and NM-physician relations. Formal management education also contributed to more positive assessments, especially regarding physician collaboration. |
| Warshawsky et al. | 2013 | USA | Quantitative | Develop and test a scale designed to describe and assess nurse managers' practice environments. | 356 | The exploratory factor analysis identified 44 items grouped into eight distinct domains, confirming the scale’s reliability. The instrument mean scores indicated an overall positive perception of nurse managers' practice environments. Among the subscales, "effective NM-unit staff relationships" and "culture of generativity" received the highest ratings, while "adequate budgeted resources" received the lowest score. |
| Warshawsky, Lake & Brandford | 2013 | USA | Qualitative | Use the words of nurse managers to illustrate these domains of the environment that support nurse managers’ practice. | 127 | Nurse managers reported feeling overwhelmed by excessive workloads, limiting their ability to focus on patient care. They emphasized the need for empowerment in decision-making and a collaborative culture that prioritizes patient safety. They also sought administrative leaders who would align budget decisions with the institution's mission and values and expressed a strong desire for closer partnership with physicians to improve patient outcomes. |
| Warshawsky, Wiggins, Rayens | 2016 | USA | Quantitative | Explore the influence of the practice environment on nurse managers job satisfaction and intent to leave | 248 | Nurse managers generally evaluate their practice environment positively, with greater job satisfaction in settings where executive leaders promote patient safety, directors empower decision-making, and workloads are balanced. Conversely, they are more likely to seek new positions when lacking time for staff development, experiencing micromanagement, or perceiving workload inequities. |
3. Discussion
This scoping review explores the scientific literature on nurse manager practice environments. To achieve this objective, eighteen primary studies and one integrative literature review were included.
Nurse leaders and direct care nurses defined a healthy work environment as appropriate staffing, authentic leadership, effective decision-making, meaningful recognition, skilled communication, true collaboration, genuine teamwork, and physical and psychological safety (Huddleston & Gray, 2016a).
Instruments to evaluate nurse manager practice environment
Warshawsky & Rayens (2013) developed the nurse manager practice environment scale with eight key factors influencing its structure and dynamics. Empowering administrative leadership emerged as a critical factor, emphasizing the role of executive leaders in fostering a culture of patient safety. The relationship between nurse managers and directors was also highlighted, focusing on clear communication, expectations, and constructive feedback. Another essential factor was the culture of generativity, which underscores the importance of staff development and professional growth. Adequate budgeted resources were recognized as vital for ensuring sufficient support and efficient processes in patient care areas. The culture of meaning linked nurse managers' work to the organization's mission, vision, and values, reinforcing their sense of purpose. Strong collegial relationships between NMs and physicians were essential for achieving quality patient outcomes. Additionally, effective NM-unit staff relationships were emphasized, reflecting the significance of teamwork and collaboration. Lastly, the workload factor, associated with work-life balance, was redefined as a fair and manageable workload, addressing concerns about job demands and responsibilities.
This instrument has also been used to evaluate the Nurse Manager Practice Environment (NMPE) in seven more studies (Aslan et al., 2022; Grandfield et al., 2023; Grubaugh, 2019; Montgomery & Patrician, 2022; Warshawsky et al., 2016). This instrument was adapted for Turkey (Aslan et al., 2022; Tosun & Yildirim, 2021) and China (Chen et al., 2024).
The American Association of Critical-Care Nurses (AACN) developed the Healthy Work Environment Assessment Tool (HWEAT) to align with nurse leaders' perceptions of a healthy work environment, resulting in the Healthy Work Environment Scale for nurse leaders (Huddleston et al., 2017; Huddleston & Gray, 2016a, 2016b).
Some studies did not employ tools tailored to nurse managers' views on their practice environment (Gormley, 2011; Jäppinen et al., 2022; Santos et al., 2018).
How nurse managers assess their practice environment
The evaluation of the nurse manager's practice environment was consistently favorable across the studies. The subscale “effective nurse manager-unit staff relationships” of the Nurse Manager Practice Environment Scale received high ratings in several studies (Aslan et al., 2022; Chen et al., 2024; Grubaugh, 2019; Montgomery & Patrician, 2022; Tosun & Yildirim, 2021; Warshawsky et al., 2016), representing the partnership between nurse managers and their front-line staff to achieve quality patient outcomes. In a different study employing the AACN Healthy Work Environment Assessment Tool, nurse managers considered the subscale of “true collaboration” to be the most positive (Huddleston et al., 2017).
In contrast, the subscales concerning human, material, or budget resources were often assessed as the lowest (Chen et al., 2024; Grubaugh, 2019; Huddleston & Gray, 2016; Montgomery & Patrician, 2022; Raso et al., 2022; Santos et al., 2018; Tosun & Yildirim, 2021; Warshawsky et al., 2016; Warshawsky & Rayens, 2013).
The results of the studies were consistent, including those carried out in diverse geographical and cultural settings.
Factors affecting the practice environment for nurse managers
A positive organizational culture creates and maintains a supportive environment that fosters healthy workplaces for practice. In negative organizational cultures, nurse managers become exhausted while trying to fulfill their roles, battling the prevailing culture and hindering their ability to create a healthy work environment (Shirey, 2009).
The span of control (SOC), availability of support positions, and experience and tenure are key factors shaping the nurse manager practice environment. A wide span of control, where a nurse manager oversees many direct reports, can create significant challenges in management, leading to increased stress, decreased effectiveness, and a negative impact on the overall work environment (Grubaugh, 2019; Warshawsky et al., 2016). A previous study identified role overload as the most critical predictor of nurse manager stress (Kath et al., 2013). The nurse managers also describe that an overwhelming workload often arises from too many daily tasks in insufficient time, leading to stress (Ogashi, 2019) and a more negative perception of the practice environment (Jäppinen et al., 2022). In the qualitative research of Warshawsky et al. (2013)Nurse managers described being overwhelmed by the sheer volume of work and lacking sufficient time to focus on patient care issues.
Chen et al. (2024) found a negative correlation between perceived stress levels and the nurse manager practice environment, which suggests that higher stress levels contribute to a more challenging and less favourable work environment
Conversely, adequate support positions can help mitigate these challenges by redistributing the workload, allowing nurse managers to focus more on leadership and staff development (Grandfield et al., 2023). Nurse managers wanted administrative leaders to set organizational priorities and make budgetary decisions that align with the organization's mission, vision, and values. Nurse managers need administrative leaders to foster organizational cultures that promote collaboration and ensure safe patient care (Warshawsky et al., 2013).
Also, career growth opportunities show a positive correlation, indicating that more significant opportunities for professional advancement enhance nurse managers' perceptions of their work environment (Chen et al., 2024). These results emphasize the need for organizational strategies to reduce workplace stressors while promoting career development pathways, ultimately fostering a more supportive and sustainable practice environment for nurse managers.
Comparison of Nurse Manager and Direct Care Nurse Practice Environments
Some studies indicate that nurse managers evaluate their practice environment more favorably than direct care nurses, with significant differences in how each group perceives key work settings. Gormley (2011) found that nurse managers rated all subscales higher than direct care nurses, except for nurse-physician collaboration. Similarly, Raso et al. (2022) reported that both groups identified "appropriate staffing" as the most critical challenge. Ogashi (2019) found that nurse leaders viewed authentic leadership as the strongest characteristic of a healthy work environment, while direct care nurses emphasized the significance of effective decision-making. Nonetheless, both groups agreed that appropriate staffing was the weakest area.
Despite these differences, other research indicates consistency among nursing roles. Santos (2018) found that nursing assistants and nurse managers perceived their work environments positively, suggesting that institutions may provide a relatively uniform practice setting regardless of managerial influence status.
These findings highlight the importance of considering differing perceptions between nurse managers and direct care nurses when assessing the overall health of the work environment. Addressing shared concerns, particularly staffing adequacy, while acknowledging role-specific priorities, may be key to improving job satisfaction, retention, and the overall work environment.
The impact of the nurse manager's practice environment on nurse manager outcomes
Nurse managers feel uneasy about expressing their opinions in practice environments where both they and their staff experience a lack of support (Aslan et al.,2022).
NMPE was a significant positive predictor of job satisfaction (Grubaugh, 2019; Warshawsky et al., 2016). In the study by Warshawsky et al. (2016), nurse managers report higher job satisfaction in practice environments where executive leaders foster a culture of patient safety, directors empower them in decision-making, provide sufficient time for staff mentorship, and ensure that workloads are balanced and equitably distributed. Organizational traits like social support, team cohesion, and approaches to alleviate job stress are linked to increased job satisfaction (Penconek et al., 2024).
The integrated literature review identified that administrative support, which fosters a healthy work environment, and the provision of resources, ensuring that nurse managers have the necessary tools and personnel, influence job satisfaction. A supportive organizational culture and a healthy practice environment further boost satisfaction. Conversely, insufficient institutional support for complex initiatives can hinder success and reduce job satisfaction. Collectively, these factors impact nurse manager retention and overall work experience (Keith et al., 2021). Nurse managers in better work environments are also more likely to recommend a career in nursing management. (Grubaugh, 2019).
In Warshawsky et al.'s (2016) study, intention to leave was predicted by three key factors: a culture of generativity, positive NM-director relationships, and a fair, manageable workload. All relationships were negative, meaning nurse managers were less likely to consider leaving when these elements were more prevalent in the organization. The intention to leave is linked to work overload, an inability to ensure quality patient care, insufficient resources, and a lack of empowerment and recognition (Ogashi, 2019). Managers who intended to leave reported significantly lower job satisfaction, poorer perceptions of their supervisor’s resonant leadership, and higher levels of burnout (Hewko et al., 2015). The study conducted during the COVID-19 pandemic also revealed that better work environments were linked to higher resilience, lower burnout, and a decreased likelihood of nurse leaders leaving their jobs (Montgomery & Patrician, 2022).
Impact of nurse manager practice environment on direct care nurses' outcomes
The impact of the nurse manager's work environment on direct care nurses is underexplored. Only one study examined this, revealing that it directly influences direct care nurses' job satisfaction, intent to stay, and sense of joy and meaning in their work. The study also uncovered significant positive indirect effects of supportive roles on job satisfaction, intent to stay, and sense of joy and meaning, which are mediated by the nurse manager's practice environment (Grandfield et al., 2023).
Conclusion
The scientific evidence about nurse managers' practice environments is limited. While the role of nurse managers in fostering a positive workplace is recognized, more research is needed to comprehend their practice environment and how it affects direct care nurses' outcomes.
Nurse managers positively evaluate their practice environment and rate it higher than direct care nurses. It seems they have different perceptions of the practice environment. Studies comparing nurse managers and direct care nurses are scarce.
The studies highlight that nurse managers' wider spans of control negatively affect job satisfaction, intent to stay, and quality of care, while supportive leadership positively impacts these outcomes.
Conversely, negative work environments characterized by high stress, excessive workloads, and a lack of administrative support obstruct their capacity to establish healthy practice settings. The key factors that shape the nurse manager's practice environment include manageable workloads, strong relationships with supervisors, sufficient opportunities for career growth, and the presence of support positions to ease role overload. Organizational strategies to enhance these areas, such as mentorship programs, leadership development initiatives, and structural changes like reducing the span of control, are crucial for cultivating a sustainable nurse manager workforce.
Validated instruments like the Nurse Manager Practice Environment Scale (Warshawsky & Rayens, 2013) and the Healthy Work Environment Assessment Tool (AACN) can help organizations identify areas for improvement, ensuring that interventions align with nurse managers' needs. Adapting these instruments across healthcare contexts underscores their relevance in evaluating and strengthening nurse manager practice environments globally.
Implications for Nursing Management and Research
Organizations should implement stress management training, career development programs, and leadership training to better support nurse managers and mitigate psychosocial stress while fostering professional growth. Addressing the workload of nurse managers is crucial. However, although narrowing the span of control by increasing nurse manager positions or adopting a co-manager model may initially incur higher costs, it can result in long-term benefits, such as improved outcomes for both nurse managers and direct care nurses.
It is important to recognize the need for further research studies to better understand how nurse managers perceive their practice environment and its impact on direct care nurses' outcomes.
Limitations
Some studies were published in languages other than English, Portuguese, or Spanish, leading to potential exclusion. This scoping review focuses only on acute care settings. Scoping reviews focus on mapping existing literature rather than assessing causal relationships. The quality of the studies wasn’t addressed.
Authors' contribution
Conceptualization, A.N., E.J. and B.A.; data curation, A.N. and E.J.; formal analysis A.N., E.J. and B.A.; investigation, A.N. and E.J.; methodology, A.N., E.J. and B.A.; project administration, A.N., E.J. and B.A.; resources, A.N., E.J. and B.A.; supervision, E.J. and B.A.; validation, E.J. and B.A.; visualization, A.N.; writing-original draft, A.N.; writing-review and editing, E.J. and B.A.